Cardiovascular Issues in Elite American-Style Football Participants
Background
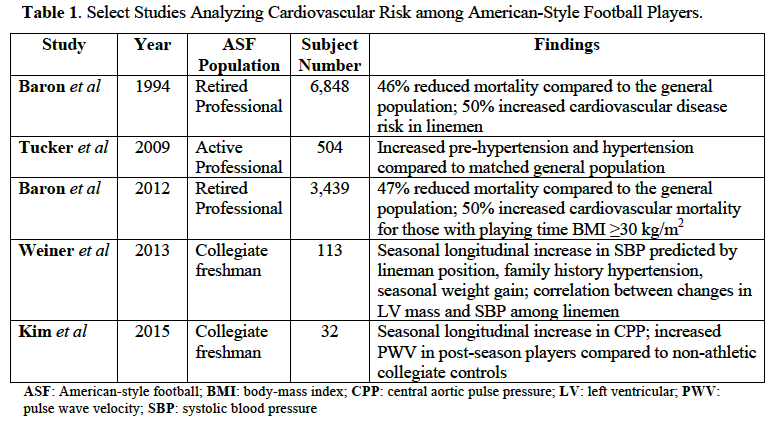
American-style football (ASF) is the most popular team sport in the United States, based on participation estimates and general public interest.1,2 Despite these trends, adverse health outcomes among retired professional ASF participants have lead to growing concerns regarding the safety of ASF participation. In particular, neurologic ASF outcomes and the posthumous diagnosis of chronic traumatic encephalopathy in retired, professional ASF players have been well documented in both the scientific literature and mainstream media.3 Although not as heavily publicized, long-term adverse cardiovascular outcomes have also been demonstrated among retired, professional ASF participants.4-6 In addition, studies focused on collegiate ASF players have demonstrated the development of hypertension and sub-clinical vascular dysfunction after one competitive ASF season.7,8 A summary of select studies analyzing cardiovascular outcomes among ASF participants is shown in Table 1. This Expert Analysis will highlight the evidence regarding cardiovascular issues in elite ASF participants, clinical perspectives based off these data, and ongoing and potential research endeavors within this focused arena.
ASF Cardiovascular Outcomes
The increased size of elite ASF players – particularly those classified as linemen position players – has always generated questions relating to the overall cardiovascular health of ASF athletes. The first analysis that evaluated cardiovascular outcomes in retired professional ASF players was conducted in 1994 by the National Institute for Occupational Safety and Health.4 Among 6,848 retired players, all cause mortality was reduced by close to 50% in ASF players compared to the general population.4 However, for the linemen (offensive and defensive), cardiovascular disease risk was increased by 50%.4 Moreover, mortality in this population was primarily attributable to hypertension and coronary artery disease.4 Further study of active professional ASF players continued with important data from Tucker and colleagues in 2009.5 In this cross-sectional analysis of 504 professional ASF players (first year players excluded), hypertension (13.8%, 95% confidence interval [CI]: 11-16.7%) and pre-hypertension (64.5%, 95% CI: 58.3-70.7%) were significantly more common in the ASF cohort compared to age-matched controls (5.5%, 95% CI: 4.6-6.6%; and 24.2%, 95% CI: 22.3-26.1%, respectively).5 Interestingly, there was not increased prevalence of impaired fasting glucose or hyperlipidemia among the ASF cohort.5 Finally, in a follow-up epidemiologic study of retired ASF players from Baron and colleagues in 2012, similar results to the analysis from 1994 were obtained.6 Out of 3,439 former players, those with a playing time body mass index ≥30 kg/m2 and former defensive linemen had increased risk of cardiovascular disease mortality compared to age and race matched controls from the general population.6
Data from collegiate ASF players emerged in 2013 from longitudinally followed freshman studied as a part of the Harvard Athletic Initiative (led by Dr. Aaron Baggish), a research group that previously included the author of this review. Data from 113 freshman ASF players were collected over six years, and obtained at pre- and post-season time points.7 In addition to significant increases observed in systolic (116±8 vs. 125±13 mm Hg, P<0.001) and diastolic blood pressure (64±8 vs. 66±10 mm Hg, P<0.001), 61% of the total cohort met criteria for either pre-hypertension or stage 1 hypertension at the post-season time point.7 Intriguingly, among linemen, changes in systolic blood pressure correlated with the changes (increases) in left ventricular mass, suggesting the possibility of maladaptive cardiac structural remodeling in hypertensive ASF players.7
Vascular Function
With the demonstration of increased blood pressure in collegiate ASF players,7 the next logical question addressed the presence of arterial stiffening in this athletic population. Important data from the general population have previously shown that arterial stiffness, as measured by the gold standard pulse wave velocity (PWV), is an important mechanistic precursor to the development of hypertension.9 In a collaborative study between a sports cardiology research group at Emory University/Georgia Tech led by this author and the Harvard Athletic Initiative, vascular function among ASF participants was addressed.8 In a small cohort of 32 freshmen collegiate ASF players from Georgia Tech and Harvard, increases in central aortic pulse pressure (27±4 vs. 34±8 mmHg, P<0.001), another measure of aortic stiffness, was observed.8 In addition, PWV was increased in the post-season ASF cohort compared to a non-athletic undergraduate control cohort (6.2±0.9 vs. 5.6±0.7 m/s, P=0.002), and ASF participation retained independent association with increased post-season PWV in multivariable analysis (β=0.33, P=0.04).8 Findings from this small cohort suggest that the presence of early sub-clinical vascular dysfunction may predispose to the increased prevalence of pre-hypertension and hypertension observed in elite collegiate and professional ASF players. However, given the small numbers of subjects studied, replication of these data is necessary in larger cohorts of ASF participants.
Clinical Implications
Despite the overall limited amounts of ASF cardiovascular-based research, there remain clinical implications taken from prior compelling data. To date, the compilation of evidence suggests elite-level ASF participants are at higher risk for the development of early hypertension. In addition, this risk may be amplified in certain ASF sub-groups, namely the linemen. Further limited data also suggest early sub-clinical vascular dysfunction develops in first year collegiate ASF players. As such, clinical efforts aimed at identifying players with increased blood pressure and ensuring close monitoring of those athletes as well as players deemed at high risk should be considered. Given the profound impact youthful hypertension imparts on later life cardiovascular morbidity and mortality,10 practitioners and athletic trainers involved in the care of ASF athletes should be aware of pre-hypertensive blood pressures measured during pre-season ASF physical assessments, and consider developing algorithms for blood pressure monitoring and follow-up throughout the season.
Management strategies may be best focused on preventive measures such as limitations in sodium intake, minimization of non-steroidal anti-inflammatory (NSAID) medication use, focused overall dietary assessments, and perhaps alterations in training regimens with the inclusion of more aerobic-based exercise. While pharmacologic management regimens have not been studied in this population, guideline-based treatment algorithms should be followed with active sports cardiology consultation as deemed appropriate. Currently, there is tremendous opportunity afforded athletic trainers, sports medicine practitioners, and sports cardiologists in identifying high-risk ASF players that could lessen cardiovascular risk upon completion of these athletes' ASF career.
Future Research Directions
While it is evident cardiovascular issues in elite ASF players require attention, many questions remain unanswered. The prevalence of hypertension in high school cohorts of ASF participants is unknown. In addition, further characterization of the temporal changes in vascular function from high school through college and potentially professional ASF is a critically important issue that requires dedicated study. These studies will require comparisons to both athletic (endurance athletes) and non-athletic control cohorts.
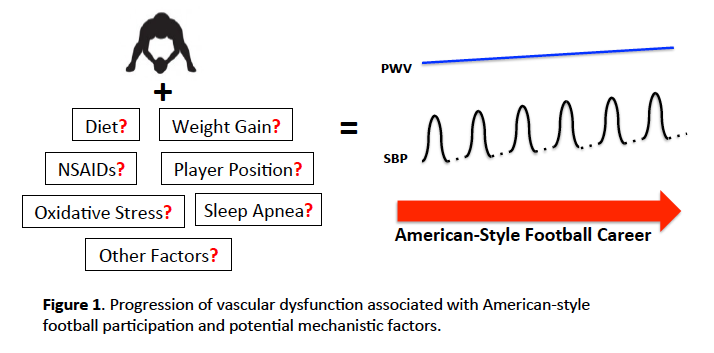
Figure 1
Mechanisms underlying both arterial stiffness and hypertension in ASF players remain speculative and represent important areas of future research. Potential etiologies worthy of study include overused NSAIDs, weight gain, changes in lean and fat body mass, excessive static/isometric training loads, oxidative stress, and undiagnosed obstructive sleep apnea (Figure 1). Each of these mechanistic analyses will require both longitudinal and observational study designs and careful inclusion of adequate controls. In addition, use of newer and sensitive methodologies for the measurement of biochemical markers and metabolomics may assist in defining molecular pathways associated with these vascular disturbances. Recent data from this author have demonstrated proof of concept with the use of high-resolution metabolomics in exhibiting training-related changes in pre- and post-season ASF metabolic profiles obtained from a small cohort of Georgia Tech ASF players.11 These preliminary results set the stage for further utilization of this methodology in upcoming future study designs.
Finally, further epidemiologic analyses investigating the impact of collegiate ASF participation on future cardiovascular morbidity and mortality remains a critically important and unresolved issue. These studies will likely require detailed and large registries of ex-collegiate ASF players. While this represents a daunting task, this could clarify the long-term impact of ASF-induced vascular dysfunction and hypertension on cardiovascular health outcomes in youthful ASF participants, the majority of whom do not embark on a professional career.
References
- National Federation of State High School Associations. Participation statistics. Available at: http://www.nfhs.org/ParticipationStatics/ParticipationStatics.aspx. Accessed 07/12/2016.
- Rose B. NFL ranked as most popular American sport for 30th consecutive year. 2014. Available at: http://www.si.com/nfl/audibles/2014/04/14/nfl-ranked-as-most-popular-american-sport-for-30th-consecutive-year. Accessed 07/12/2016.
- McKee AC, Cantu RC, Nowinski CJ, et al. Chronic traumatic encephalopathy in athletes: progressive tauopathy after repetitive head injury. J Neuropathol Exp Neurol 2009;68:709-35.
- Baron S, Rinsky R. National Institute of Occupational Safety and Health, Department of Health and Human Services, National Football League causes of death, Letter, January 10, 1994.
- Tucker AM, Vogel RA, Lincoln AE, et al. Prevalence of cardiovascular disease risk factors among National Football League players. JAMA 2009;301:2111-9.
- Baron SL, Hein MJ, Lehman E, Gersic CM. Body mass index, playing position, race, and the cardiovascular mortality of retired professional football players. Am J Cardiol 2012;109:889-96.
- Weiner RB, Wang F, Isaacs SK, et al. Blood pressure and left ventricular hypertrophy during American-style football participation. Circulation 2013;128:524-31.
- Kim JH, Sher S, Wang F, et al. Impact of American-style football participation on vascular function. Am J Cardiol 2015;115:262-7.
- Kaess BM, Rong J, Larson MG, et al. Aortic stiffness, blood pressure progression, and incident hypertension. JAMA 2012;308:875-81.
- McCarron P, Okasha M, McEwen J, Davey Smith G. Blood pressure in early life and cardiovascular disease mortality. Arch Intern Med 2002;162:610-1.
- Kim JH, Banton SA, Awad M, et al. Training-Related Metabolic Adaptations in American-Style Football Participants. Ann Sports Med Res 2015;2:1048.
Keywords: Anti-Inflammatory Agents, Non-Steroidal, Arterial Pressure, Athletes, Biomarkers, Blood Pressure, Blood Pressure Determination, Body Mass Index, Brain Injury, Chronic, Coronary Artery Disease, Fat Body, Football, Glucose, Hyperlipidemias, Hypertension, Metabolome, Metabolomics, Oxidative Stress, Prehypertension, Pulse Wave Analysis, Registries, Risk Factors, Sleep Apnea, Obstructive, Sports Medicine, Vascular Stiffness, Weight Gain
< Back to Listings