Women and CV Disease: Beyond the Bikini
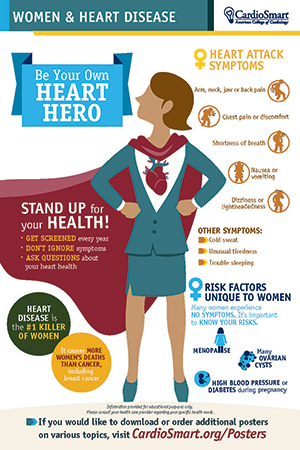
Cardiovascular disease is the leading killer of both men and women in the United States. For women alone, 1 in 4 will die from cardiovascular disease. That’s more than the number of women who will die from cancer, including breast cancer.
Given these statistics, the obvious question arises: Are we doing enough to prevent and treat cardiovascular disease in women? There are some great initiatives focused on raising awareness about women and heart disease, including the American Heart Association’s Go Red for Women campaign and The Heart Truth program from the National Heart, Lung, and Blood Institute. These programs have made significant progress over the years in drawing attention to this issue at national and local levels; however, more work is needed.
More than three decades ago, Nanette Wenger, MD, MACC, coined the term “bikini medicine.” She noted that when it comes to treating women medical professionals tend to focus on the bikini-defined areas, concentrating on the breasts and the reproductive organs, while essentially ignoring the rest of the woman. Today, one can argue that “bikini medicine” is still largely the norm, with women continuing to be less likely to get adequate screening and treatment for cardiovascular risk factors, and more likely to experience delays in diagnosis and treatment. As a result, women are more likely to die in the first year after a heart attack compared with men.
As a woman, who also happens to be a cardiologist and editor-in-chief of CardioSmart, finding ways to encourage women and health care professionals to look beyond the bikini zone is a priority. Ensuring that women understand that their heart attack symptoms can (and will likely be) different from men is a first step. Women’s symptoms may occur more often when they are resting, or even when they’re asleep. They are also easier to downplay, causing women to show up in the emergency room after heart damage has already occurred.
Additionally, making sure that women get screened each year and know their risks is another vital step. Many women don’t experience any symptoms at all, so understanding that diabetes, smoking, inactivity, depression and stress place them at greater risk of heart disease than men is key. Additionally, menopause and pregnancy complications, which are obviously unique to women, can pose significant risk factors for cardiovascular disease.
Women need to feel comfortable standing up for their health. In today’s health care environment where team-based care and increased physician/patient interaction is increasingly the norm, there are new opportunities for all parties to work more closely together to understand signs, symptoms and risks. If we are going to turn the tide on heart disease in women, we need to go beyond the red dress and the bikini and look at the whole woman. It’s our job and, for my fellow women cardiovascular professionals, it’s also our lives.
Visit CardioSmart.org/WomenHeartDisease for a comprehensive selection of patient tools and resources focused on women and heart disease, including tips for staying healthy, a list of questions to ask health care professionals and a closer look at the myths surround women and heart disease.
 Read the full May 2017 issue of Cardiology at ACC.org/Cardiology Read the full May 2017 issue of Cardiology at ACC.org/Cardiology |
Keywords: ACC Publications, Cardiology Magazine, American Heart Association, Attention, Breast, Breast Neoplasms, Cardiovascular Diseases, Depression, Diabetes Mellitus, Emergency Service, Hospital, Female, Heart Diseases, Menopause, Myocardial Infarction, National Heart, Lung, and Blood Institute (U.S.), Pregnancy, Pregnancy Complications, Risk Factors, Smoking
< Back to Listings
