Feature | Closing the Gap on Understanding Patent Foramen Ovale and Cryptogenic Stroke?
Stroke is a leading cause of death and long-term disability worldwide. Nearly 40 percent of young patients who have an embolic or ischemic stroke have no identifiable cause.1 Imaging studies to assess cardiac shunting using transthoracic echocardiography and transesophageal echocardiography (TEE) is recommended by guidelines for early management of patients with acute ischemic stroke.2 The current guidelines from the American Heart Association (AHA) and the ACC/AHA recommend intensive cardiovascular risk control with statins, antihypertensive therapy, standard dose antiplatelet therapy and lifestyle modifications for secondary prevention of ischemic stroke.3,4
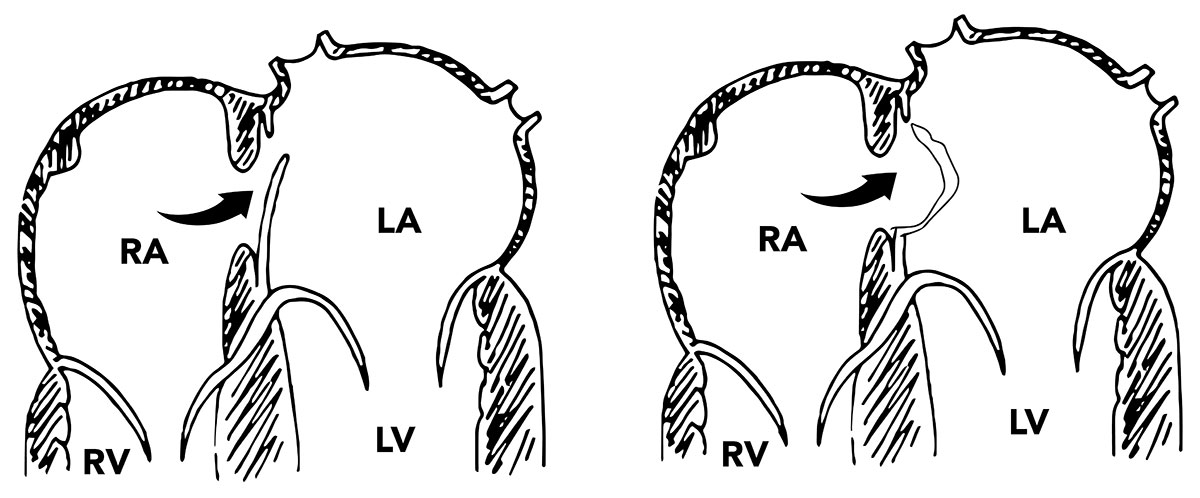
Patent foramen ovale, an intra-atrial anatomical communication that’s an embryonic remnant, is relatively common among the general population. Normally, PFO closes at birth, however, in about 25 percent it fails to close.5 The average risk of a recurrent stroke is 3.8 percent in patients with a PFO and cryptogenic ischemic stroke.6
The association between unexplained “cryptogenic” stroke and the presence of PFO has been reaffirmed by results from three studies of transcatheter PFO closure published in late 2017 — CLOSE, Gore REDUCE and the long-term results from RESPECT — and more recently the DEFENSE-PFO study presented at ACC.18 and published in the Journal of the American College of Cardiology.7 At least four meta-analyses, excluding DEFENSE-PFO, have been published since.
Transcatheter closure is not recommended by the ACC/AHA guidelines, written before these study results were available, for the routine closure of PFOs. While perhaps mostly limited to use in clinical trials, what does the recent evidence tell us about the benefit and safety of PFO closure for preventing a secondary stroke?
Three early studies (CLOSURE I, PC, RESPECT) failed to show benefit with PFO closure over medical therapy alone to prevent recurrent stroke.8, 9, 10 However, results from CLOSE and Gore REDUCE and the long-term follow-up of the RESPECT study demonstrated a significant reduction in stroke recurrence with PFO combined with antiplatelet therapy compared with antiplatelet therapy alone.11,12,13 Theoretically, this difference in the results of trials has been blamed on the size of PFO being closed by the transcatheter method, because the PFO size was bigger in these most recent trials. Also, suboptimal PFO closure was seen in 14 percent of patients in the CLOSURE trial.
The CLOSE trial included 663 patients with cryptogenic stroke and PFO with the goal of evaluating PFO closure vs. anticoagulation vs. antiplatelet therapy in patients with high-risk characteristics for recurrent stroke. After 5.3 years of follow-up, the study showed no fatal or nonfatal ischemic strokes in the PFO closure group compared with 14 strokes in the antiplatelet-only group (hazard ratio [HR], 0.03; p<0.001). The data from CLOSE suggest that at five years one stroke is avoided for every 20 closures.
However, the avoided stroke may not be a disabling stroke. None of the 238 patients in the closure group had a disabling stroke; one of 235 patients in the antiplatelet group had a disabling stroke. Despite lower rates of stroke in the PFO closure group, there was a higher rate of atrial fibrillation (AFib) requiring anticoagulation which confounded the association between PFO closure and recurrence of stroke. Overall results of the CLOSE trial were in favor of PFO closure — but left the question of the long-term impact of AFib on young patients unanswered. With a nearly similar number of patients the REDUCE trial included 664 patients. After 24 months of follow-up, REDUCE indicated that PFO closure with the Gore Septal Occluder was superior to medical management (1.4 vs. 5.4 percent; HR, 0.23; p=0.002). The data from REDUCE suggest that for every 28 patients who undergo PFO closure one stroke is avoided at two years.
Finally, on long-term follow-up (mean 5.9 years), the RESPECT trial showed there was a significant reduction in recurrent ischemic strokes in favor of PFO closure (0.58 vs. 1.07 per 100 patient-years; HR, 0.55; p=0.046). Based on these findings, the U.S. Food and Drug Administration (FDA) approved the use of the Amplatzer PFO occluder in patients between ages 18-60 years with a cryptogenic stroke.
A recently published meta-analysis of five studies with 3,440 patients (1,829 patients randomized to device closure and 1,611 to medical therapy) found that PFO closure was superior to medical therapy for prevention of stroke (HR, 0.32; p=0.018).14 The risk of AFib, however, was significantly increased with device closure (risk ratio, 4.68; p<0.001; heterogeneity I2=27.5 percent). Moreover, in patients with large shunts, PFO closure was associated with a significant reduction in stroke (HR, 0.33; p=0.005), while there was no significant reduction in stroke in patients with a small shunt (HR, 0.90; p=0.712). There was no effect from the presence or absence of an atrial septal aneurysm on outcomes. This suggests careful patient selection for PFO closure given the risk of AFib associated with PFO closure compared with medical therapy. This is especially important because the population treated with PFO closure are often young and the burden of AFib and long-term anticoagulation is not identified.
The results from DEFENSE-PFO were consistent in showing a benefit of adding PFO closure to medical therapy. However, the small sample size, premature termination of enrollment (because of evidence of benefit from the recent trials) as well as the high rate of crossover in both arms are major limitations of the study.
The DEFENSE-PFO study was an attempt to define the high-risk features of PFO morphology in patients with cryptogenic stroke — a study question inspired by the CLOSURE I and RESPECT trials, which had negative results but had subset analyses that pointed to a signal of benefit in patients with morphological features of high-risk PFO. These features include a PFO with a large shunt, atrial septal aneurysm or hypermobile septum.
Indeed, in his presentation of the DEFENSE-PFO study, Jae-Kwan Song, MD, PhD, suggested the improved selection of patients with high-risk morphology may help to explain the effective prevention of recurrent stroke found in the CLOSE, RESPECT and Gore REDUCE studies.
In the open-label DEFENSE-PFO trial, 120 patients with high-risk PFO were randomized 1:1 to transcatheter PFO device closure plus medical therapy or medical therapy alone. High-risk PFO was defined as PFO with atrial septal aneurysm, hypermobility or PFO size ≥2 mm. Medical therapy included anticoagulants (excluding direct oral anticoagulants) or antiplatelet drugs as determined by the patients’ physicians.
After a median follow-up of 2.8 years, no primary endpoint events — defined as composite of stroke, vascular death or TIMI-defined major bleeding — occurred in the device group, but there were six events in the medical therapy group. The two-year event rate was 13 percent in the medical therapy group (log-rank p=0.013). Transient ischemic attack was reported in one patient receiving medical therapy alone. In the device group, procedural complications included atrial fibrillation (n=2), pericardial effusion (n=1) and puncture site reaction (n=1).
Along with the results from the CLOSE, RESPECT and Gore REDUCE studies, these findings from DEFENSE-PFO confirm the clear importance of optimizing patient selection. These trials provide important data in the work to best define who will and will not benefit from transcatheter PFO closure.
Based on these results, patients with atrial septal aneurysm, hypermobility or PFO size ≥2 mm appear to be benefit and may be considered candidates for PFO closure.
Comprehensive assessment to select optimal candidates after a cryptogenic stroke should include an extensive and systematic evaluation by a neurologist and cardiologist to exclude atherosclerotic vascular disease, an intracardiac embolic source, a stroke associated with major intracranial and extracranial vascular pathologies, and a hypercoagulable status.
We must be mindful that the optimal medical therapy after PFO closure is not well defined. More studies are needed to clarify this. In the meantime, careful patients selection through identification of high-risk morphology is essential. Shared decision-making with each patient that includes a careful review of the current evidence and discussion of the risks and expectation is a must.

This article was authored by M. Chadi Alraies, MD, a fellow in interventional cardiology at Wayne State University, Detroit Medical Center, Detroit Heart Hospital, Detroit, MI.
References
- Goldstein LB, Bushnell CD, Adams RJ, et al. Stroke 2011;42:517-84.
- Jauch EC, Saver JL, Adams HP Jr, et al. Stroke 2013;44:870-947.
- Furie KL, Kasner SE, Adams RJ, et al. Stroke 2011;42:227-76.
- Smith SC Jr, Benjamin EJ, Bonow RO, et al. J Am Coll Cardiol 2011;58:2432-46.
- Bang OY, Lee MJ, Ryoo S, et al. J Stroke 2015;17:229-37.
- Kitsios GD, Dahabreh IJ, et al. Stroke 2012;43:422-31.
- Lee PH, Song J-K, Kim JS, et al. J Am Coll Cardiol 2018;March 12:[Epub ahead of print].
- Furlan AJ, Reisman M, Massaro J, et al. N Engl J Med 2012;366:991-9.
- Meier B, Kalesan B, Mattle HP, et al. N Engl J Med 2013:368:1083-91.
- Carroll JD, Saver JL, Thaler DE, et al. N Engl J Med 2013;368:1092-1100.
- Mas J-L, Derumeaux G, Guillon B, et al. N Engl J Med 2017;377:1011-21.
- Sondergaard L, Kasner SE, Rhodes JF, et al. N Engl J Med 2017;377:1033-42.
- Saver JL, Carroll JD, Thaler DE, et al. N Engl J Med 2017;377:1022-32.
- Ahmad Y, Howard JP, Arnold A, et al. Eur Heart J 2018;0:1-12.
Keywords: ACC Publications, Cardiology Interventions, American Heart Association, Aneurysm, Anticoagulants, Antihypertensive Agents, Atherosclerosis, Atrial Fibrillation, Brain Ischemia, Cardiovascular Diseases, Cause of Death, Decision Making, Echocardiography, Echocardiography, Transesophageal, Embolism, Follow-Up Studies, Foramen Ovale, Patent, Heart Septal Defects, Atrial, Hemorrhage, Hydroxymethylglutaryl-CoA Reductase Inhibitors, Infant, Newborn, Ischemic Attack, Transient, Life Style, Patient Selection, Pericardial Effusion, Platelet Aggregation Inhibitors, Risk, Risk Factors, Sample Size, Secondary Prevention, Septal Occluder Device, Stroke, Thrombolytic Therapy, United States Food and Drug Administration
< Back to Listings