ACS Management in a Patient in Need of Noncardiac Surgery
Introduction
Patients with acute coronary syndrome (ACS) benefit from potent antithrombotic therapy and, for those with high-risk clinical features, early invasive risk stratification. This strategy reduces short- and long-term major adverse cardiac events, but it also increases the risk for bleeding. In some scenarios, the risk of bleeding may be particularly acute and predictable. For example, the care of patients who require noncardiac surgery and develop ACS preoperatively involves a careful balance between ischemia and bleeding.1
Case Report
A 70-year-old male patient with a history significant for T4N2 rectal cancer treated with resection, radiation, and chemotherapy presented with melena for 3 weeks and intermittent chest pain for 2 weeks. On arrival, the troponin I was 0.24 ng/mL (upper limit of normal 0.04 ng/mL). The patient's hemoglobin was 8.3 g/dL, significantly decreased from his baseline of 12 g/dL 3 months prior to presentation. The mean corpuscular volume was consistent with microcytic anemia. The patient was admitted to the hospital for further workup of gastrointestinal bleeding and non-ST-segment elevation myocardial infarction (MI).
Due to the gastrointestinal bleeding and anemia, P2Y12 inhibition and antithrombin therapy was withheld. Gastroenterology performed upper endoscopy, which revealed a 5-cm friable mass in the esophagus. Biopsies were consistent with esophageal adenocarcinoma. An oncology evaluation indicated that this was a second primary malignancy. Computed tomography and positron emission tomography scans were negative for metastasis. Prior to treatment, which included surgical resection, chemotherapy, and radiation therapy, it was recommended that the patient undergo coronary angiography to define the burden of coronary artery disease (CAD).
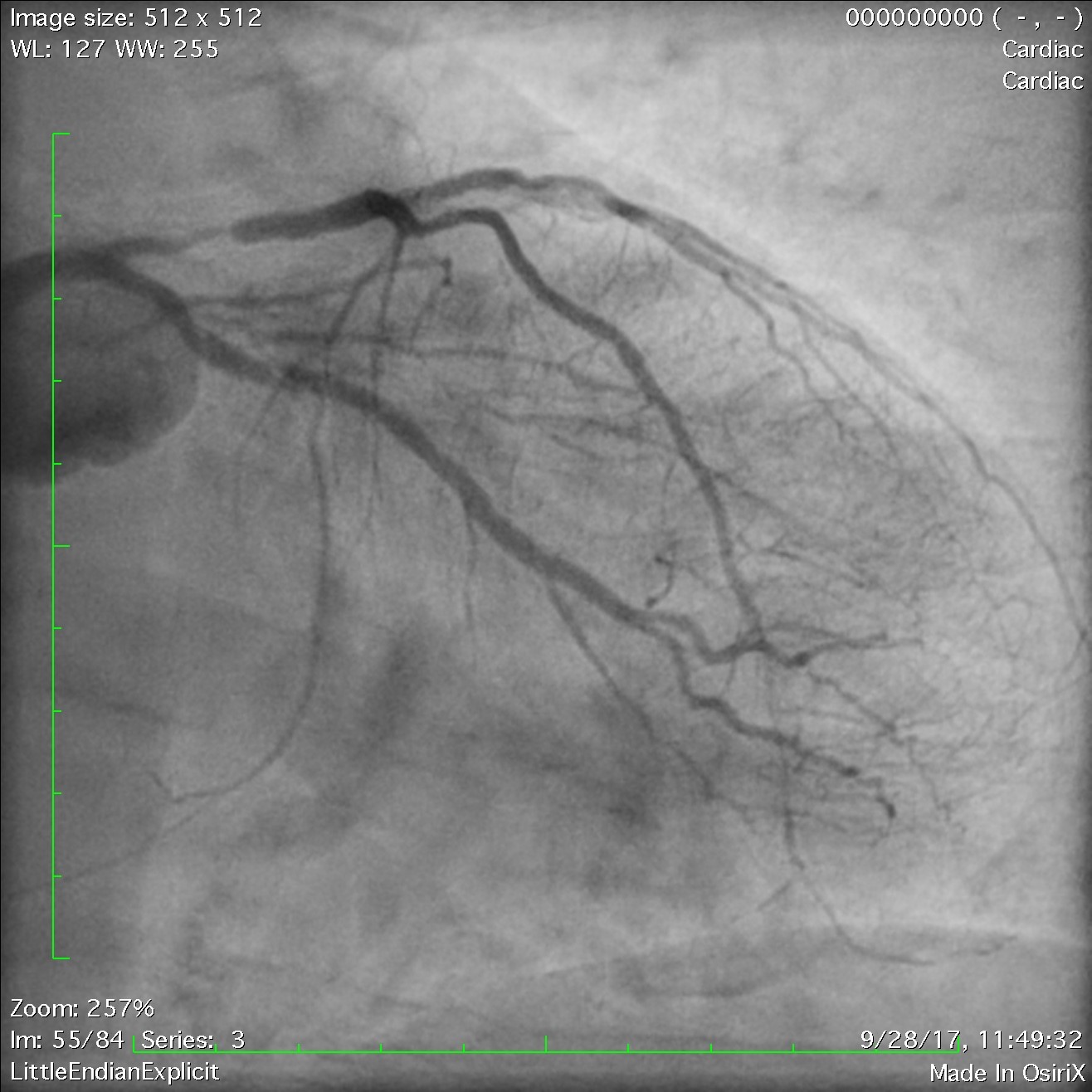
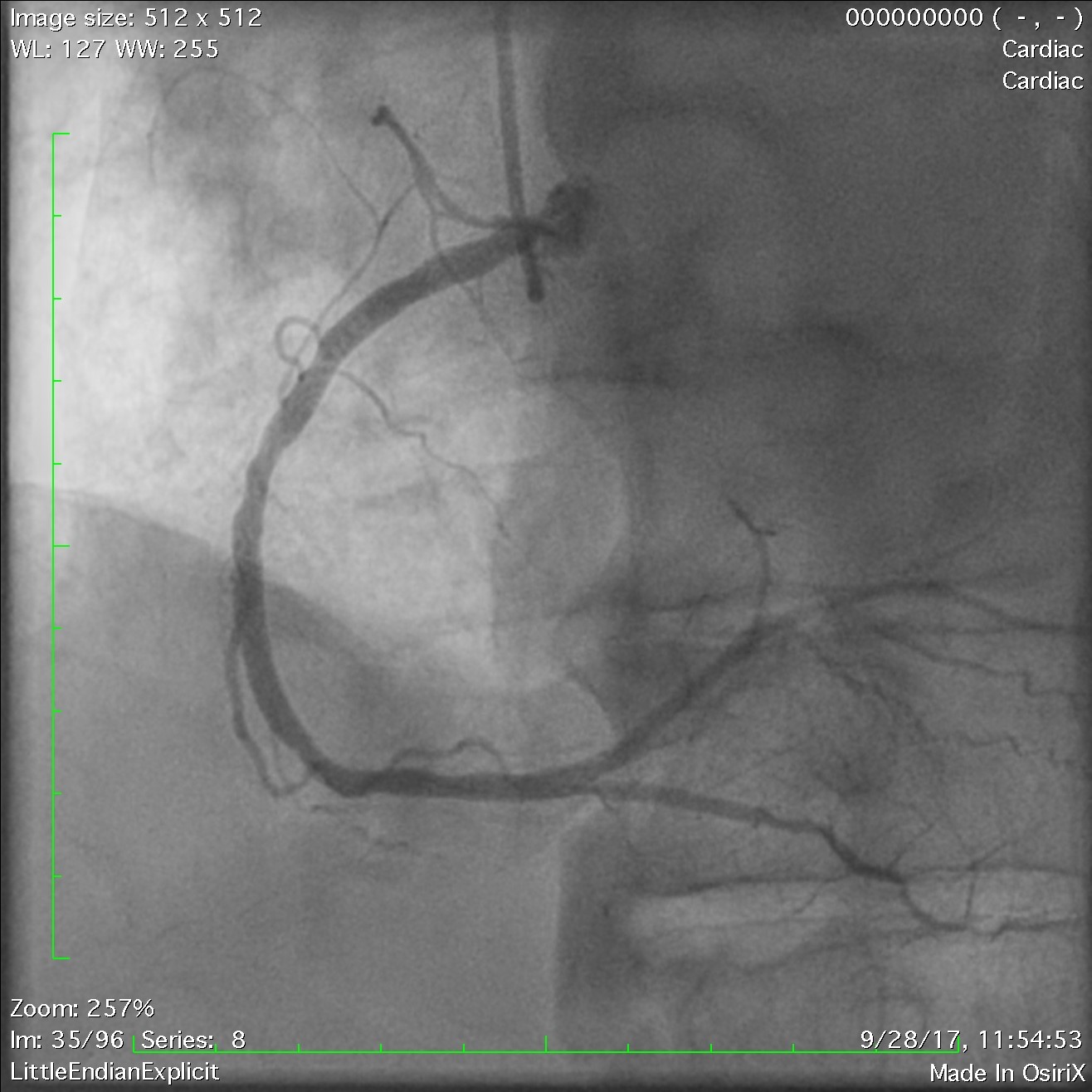
Subsequent left heart catheterization revealed two-vessel CAD with disease located in the left anterior descending and left circumflex arteries with a low SYNTAX score of 11 (Figures 1-2). Due to the requirement for impending surgery, the decision was made to attempt optimal medical therapy including aspirin, statin, angiotensin-converting enzyme inhibitor, nitrates, and ranolazine. Beta-blocker therapy was held due to bradycardia. P2Y12 inhibition was not prescribed to reduce bleeding risk because surgery may be required. Unfortunately, the patient continued to have exertional and rest angina.
Figure 1
Figure 2
After discussion of risks and benefits, patient underwent percutaneous coronary intervention (PCI) of the diseased vessels. The decision regarding stent type needed to balance long-term efficacy with safety, in particular the risk of stent thrombosis with early discontinuation of dual antiplatelet therapy (DAPT) that would be required for esophageal surgery. Although contemporary drug-eluting stents (DES) are safer than bare-metal stents (BMS) with respect to late and very late stent thrombosis, it is unclear whether this safety advantage extends to acute and subacute stent thrombosis. Because the plan was to perform surgical resection as soon as possible, the patient underwent PCI with BMS (Figure 3). The patient was subsequently discharged home after PCI on aspirin and clopidogrel with planned therapy lasting 2 weeks with close follow-up. The patient remained chest-pain free with no further angina or melena 2 days after PCI and was discharged home with a plan to pursue surgical resection of his esophageal malignancy after completion of his course of DAPT.
Figure 3
Discussion
CAD is one of the most prevalent diseases in the country and a leading cause of mortality. ACS is defined by the presence of unstable angina or MI from plaque rupture leading to thrombus formation in the coronary artery. For this reason, DAPT with aspirin and P2Y12 receptor antagonists is foundational for the management of ACS. In addition, invasive risk stratification with coronary angiography and revascularization for high-risk patients reduces long-term morbidity and mortality. If revascularization with PCI is pursued, then DAPT is indicated to also reduce the risk of stent thrombosis. An important risk of DAPT is bleeding, which can occur both acutely and during long-term therapy. This balance of ischemic benefit and bleeding risk is a common clinical challenge seen in ACS patients and can be particularly vexing when a patient with recent ACS and/or PCI requires noncardiac surgery.2
The incidence of noncardiac surgery after undergoing PCI, as seen in our case, is roughly 5-10%.3 This poses a difficult scenario for the clinician when an ACS/PCI patient requires urgent noncardiac surgery. There are two clinical challenges on both initial management of ACS and handling of DAPT after PCI. Current guidelines recommend delaying noncardiac surgery if possible based on stent type chosen during PCI. For BMS, current recommendations are delaying surgery for at least 4-6 weeks; for DES, the delay is thought to be between 6 and 12 months.4 This time frame is derived from the difference in time to stent endothelialization, which can affect the risk of stent thrombosis.5
BMS was reportedly used more frequently in patients with planned noncardiac surgery at the time of PCI. In our case, the decision was made to use BMS because of the known urgency of noncardiac surgery, increased surgical bleeding risk with continued DAPT, and the inability to delay surgery much longer than 1 month. Use of BMS allowed for the patient to stop DAPT sooner so that he could proceed with surgery. The patient was still at high risk for complications, but the benefits of noncardiac surgery outweighed the risks. In a study by Holcomb et al. of patients with PCI for ACS with MI, patients had the greatest risk of adverse events 30 days following surgery and highest overall risk within 3 months of PCI regardless of stent type.5
In a different scenario in which noncardiac surgery is not planned or can be delayed longer, DES may be a more fitting option for PCI. There are several recent reports that current generation DES may be associated with lower rate of stent thrombosis and are as safe as BMS prior to noncardiac surgery if the surgery is more than 6 months after PCI.6 A comparison of DES versus BMS within 1 year prior to noncardiac surgery by Bangalore et al. revealed no higher adverse events following DES implantation for 30-day postsurgical outcomes.7 In a study by Egholm et al., the comparison was made between patients treated with DES and patients with no ischemic heart disease who both required noncardiac surgery. Patients who had undergone PCI with DES had higher risk for MI within 1 month after intervention but no higher risk of overall mortality. Interestingly, the risk difference was the same if surgery was delayed at least 1 month after PCI.8
Patients who have PCI and then require urgent noncardiac surgery also need careful management of DAPT, which is the next clinical challenge to our case. Over the last 2 decades, there has been a reduction in adverse events after PCI due to evolution in device technology and pharmacotherapy.9 The risks of perioperative and postoperative complications of noncardiac surgery depend on timing of the surgery, patient overall status, magnitude of the surgery, control of other comorbidities, and other factors.10 Multiple studies have shown that shortening duration of DAPT reduces the bleeding risks, and longer time on DAPT is shown to reduce the risk of stent thrombosis and further ischemia.4 Preoperative administration of short-acting antiplatelet agents has been suggested as a bridging therapy to prolong time on DAPT and reduce risk for stent thrombosis; however, it has very limited study. In a meta-analysis of patients undergoing surgery after PCI by Warshauer et al., bridging therapy with glycoprotein IIb/IIIa inhibitors did not lower the risk of perioperative stent thrombosis. In our case, the patient had a high bleeding risk, so bridging therapy was not considered.11
In all cases, DAPT should be restarted after surgery as soon as possible to minimize further risk of cardiac events if surgery cannot safely be delayed. The risk of stent thrombosis is intensified by the stress of surgery. Reddy and Vaitkus retrospectively studied patients who underwent noncardiac surgery after PCI, revealing similar risks of thrombosis in the postsurgical state even after resumption of DAPT.12 Aspirin therapy can likely be continued safely for most types of noncardiac surgery. Graham et al. recently looked at a subgroup analysis of the POISE-2 (Perioperative Ischemic Evaluation 2) trial, with results suggesting that patients with prior PCI have reduction in postoperative MI when aspirin is continued perioperatively.13
Conclusion
Ultimately, the decision on length of DAPT and type of coronary intervention is best made on an individualized basis. If a patient has ACS and has known urgent noncardiac surgery in the near future, as seen in the case presented, it is reasonable to use BMS with early discontinuation of DAPT. If the surgery is non-urgent, then DES is more advantageous than BMS. Our case underscores the need for more evidence regarding safest management of patients with ACS and those undergoing PCI needing urgent noncardiac surgery.
References
- Wessler JD, Kirtane AJ. Patients who require non-cardiac surgery in acute coronary syndrome. Curr Cardiol Rep 2013;15:373.
- Schulman-Marcus J, Pashun RA, Feldman DN, Swaminathan RV. Coronary Angiography and Revascularization Prior to Noncardiac Surgery. Curr Treat Options Cardiovasc Med 2016;18:3.
- Sanon S, Rihal CS. Non-cardiac surgery after percutaneous coronary intervention. Am J Cardiol 2014;114:1613-20.
- Vidula MK, Secemsky EA, Yeh RW. Duration of Dual Antiplatelet Therapy for Stented Patients: An Update for the Clinician. Prog Cardiovasc Dis 2018;60:491-9.
- Holcomb CN, Hollis RH, Graham LA, et al. Association of Coronary Stent Indication With Postoperative Outcomes Following Noncardiac Surgery. JAMA Surg 2016;151:462-9.
- Armstrong EJ, Graham L, Waldo SW, Valle JA, Maddox TM, Hawn MT. Patient and lesion-specific characteristics predict risk of major adverse cardiovascular events among patients with previous percutaneous coronary intervention undergoing noncardiac surgery. Catheter Cardiovasc Interv 2017;89:617-27.
- Bangalore S, Silbaugh TS, Normand SL, Lovett AF, Welt FG, Resnic FS. Drug-eluting stents versus bare metal stents prior to noncardiac surgery. Catheter Cardiovasc Interv 2015;85:533-41.
- Egholm G, Kristensen SD, Thim T, et al. Risk Associated With Surgery Within 12 Months After Coronary Drug-Eluting Stent Implantation. J Am Coll Cardiol 2016;68:2622-32.
- Spoon DB, Lennon RJ, Psaltis PJ, et al. Prediction of Cardiac and Noncardiac Mortality After Percutaneous Coronary Intervention. Circ Cardiovasc Interv 2015;8:e002121.
- Saia F, Belotti LM, Guastaroba P, et al. Risk of Adverse Cardiac and Bleeding Events Following Cardiac and Noncardiac Surgery in Patients With Coronary Stent: How Important Is the Interplay Between Stent Type and Time From Stenting to Surgery? Circ Cardiovasc Qual Outcomes 2016;9:39-47.
- Warshauer J, Patel VG, Christopoulos G, Kotsia AP, Banerjee S, Brilakis ES. Outcomes of preoperative bridging therapy for patients undergoing surgery after coronary stent implantation: a weighted meta-analysis of 280 patients from eight studies. Catheter Cardiovasc Interv 2015;85:25-31.
- Mangels DR, Nathan A, Tuteja S, Giri J, Kobayashi T. Contemporary Antiplatelet Pharmacotherapy in the Management of Acute Coronary Syndromes. Curr Treat Options Cardiovasc Med 2018;20:17.
- Graham MM, Sessler DI, Parlow JL, et al. Aspirin in Patients With Previous Percutaneous Coronary Intervention Undergoing Noncardiac Surgery. Ann Intern Med 2018;168:237-44.
Keywords: Acute Coronary Syndrome, Adenocarcinoma, Anemia, Angina Pectoris, Angina, Unstable, Angiotensin-Converting Enzyme Inhibitors, Aspirin, Biopsy, Bradycardia, Cardiac Catheterization, Comorbidity, Coronary Angiography, Coronary Artery Disease, Drug-Eluting Stents, Endoscopy, Erythrocyte Indices, Esophagus, Factor X, Fibrinolytic Agents, Follow-Up Studies, Gastroenterology, Hemoglobins, Hydroxymethylglutaryl-CoA Reductase Inhibitors, Myocardial Infarction, Myocardial Ischemia, Percutaneous Coronary Intervention, Platelet Aggregation Inhibitors, Platelet Glycoprotein GPIIb-IIIa Complex, Positron-Emission Tomography, Postoperative Complications, Purinergic P2Y Receptor Antagonists, Rectal Neoplasms, Retrospective Studies, Risk Assessment, Stents, Thrombosis, Ticlopidine, Tomography, Troponin I
< Back to Listings