Current Key Questions on COVID-19 and Cardiovascular Disease
The following is a digest of ACC's clinical guidance on the cardiac implications of COVID-19.
Organized in an FAQ format for easy navigation, this guidance is summarized from more extensive documents and approved by the ACC Science and Quality Committee. This FAQ is intended to be topical, not comprehensive.
- Vaccine-induced Thrombotic Thrombocytopenia (VITT) and COVID-19 Vaccines: What Cardiovascular Clinicians Need to Know
- What are the considerations for cardiomyopathy and heart failure in COVID-19?
- What are considerations for long-term management of COVID-19-related myocarditis?
- What is home-based cardiac rehabilitation, and how could it be used during the COVID-19 pandemic?
- How best to use telehealth to manage CV conditions during the pandemic?
- What are thrombosis risk and management considerations in COVID-19?
- How can clinician wellness be maintained?
- How best to manage CV operations (e.g., EP procedures, interventional cardiology procedures, etc.) during the pandemic?
- How should patients with cardiovascular conditions manage potential workplace exposure to COVID-19?
Vaccine-induced Thrombotic Thrombocytopenia (VITT) and COVID-19 Vaccines: What Cardiovascular Clinicians Need to Know

Category: COVID Vaccination
Patient Type: COVID-19 Vaccinated
Prevalence: Extremely rare
Principal Guidance: In extremely rare cases, the Johnson & Johnson/Jansen and Astra Zeneca COVID-19 vaccinations may cause vaccine-induced thrombotic thrombocytopenia (VITT), a condition characterized by simultaneous acute thrombosis and thrombocytopenia. The condition is similar to heparin-induced thrombocytopenia. Specific risk factors for VITT have yet to be determined given the extremely low case count, though presentation seems to appear between 5-28 days post vaccination. Patients should be reassured that the benefits of vaccination against COVID-19 far outweigh any potential risk. Diagnostic, therapeutic, and patient communication recommendations are included below.
Authors: Geoffrey D. Barnes, MD, MSc, FACC; Adam Cuker, MD, MS; Gregory Piazza, MD, MS, FACC; Deborah Siegal, MD, MSc
SQC Approval Date: April 21, 2021
What is VITT and how common is it?
Vaccine-induced thrombotic thrombocytopenia (VITT) also has been referred to as vaccine-induced prothrombotic immune thrombocytopenia (VIPIT). This condition is similar to heparin-induced thrombocytopenia (HIT) but is associated with prior administration of the Johnson & Johnson/Janssen or AstraZeneca COVID-19 vaccines without prior exposure to heparin. To date (April 21, 2021), this condition has not been reported in patients who have received the Moderna or Pfizer COVID-19 vaccines.
VITT is characterized by the presence of two conditions concurrently: thrombosis (often in unusual sites like the cerebral sinus veins or splanchnic veins) AND thrombocytopenia. Early mechanistic evaluations have identified antibodies to the platelet factor 4 (PF4)-heparin complex, similar to HIT antibodies. Detection of the PF4 antibodies can be done using a HIT ELISA test, but not reliably with other HIT laboratory tests.
The incidence of VITT is not certain, but it appears to be extremely rare. The Centers for Disease Control and Prevention (CDC) announced 6 cases among more than 6 million people vaccinated with Johnson & Johnson COVID-19 vaccine. Ongoing investigations will help to better describe the incidence of VITT and inform the CDC's future decision on vaccine administration based on overall benefits and risk. The risk of death and serious outcomes of COVID-19 (including thrombosis) far outweigh the small risk of VITT.
Who is at risk for VITT?
Early data suggest that VITT occurs only following a COVID-19 vaccination with Johnson & Johnson or AstraZeneca vaccine. Note that AstraZeneca vaccine is NOT available in the United States. Furthermore, the small number of reported events occurred between 5-28 days following the vaccine. They have not been reported to occur immediately (within 1-2 days) or longer-term (beyond 3-4 weeks) after vaccination. It will be important to re-evaluate the "at risk" window as more is learned about VITT.
Demographic and clinical risk factors for the development of VITT are uncertain. Most patients who developed VITT were younger (age <60 years). While all of the cases following Johnson & Johnson vaccine in the United States occurred in women, both men and women have been diagnosed with VITT following AstraZeneca vaccine in other parts of the world.
Specific clinical risk factors for VITT have not been identified. There is no evidence that patients with a history of thrombosis, thrombophilia, or HIT are at increased risk for VITT.
What should I do if I suspect a case of VITT?
The first thing to do for a suspected case of VITT is to verify COVID-19 vaccine details – which vaccine and when was it administered? Only patients who have received Johnson & Johnson or AstraZeneca vaccine 5-28 days previous to symptoms onset are at risk based on current information.
Next, imaging appropriate to their symptoms (e.g., CT or MR venogram of the head for suspected cerebral sinus vein thrombosis) and an urgent complete blood count (including platelet count) are appropriate. If either test is normal (no thrombosis or thrombocytopenia), then VITT can be excluded. If BOTH tests are abnormal (acute thrombosis and thrombocytopenia), hospitalization for further evaluation and treatment guided by a hematologist or other thrombosis expert is appropriate.
What should I tell my patients who call with questions about VITT and COVID-19 vaccines?
First, provide reassurance that these events are extremely rare. In the rare event that VITT occurs, hospitals and doctors have the tools to diagnose and treat this condition.
Second, remind them that VITT has only been seen with the Johnson & Johnson and AstraZeneca COVID-19 vaccines. Note that AstraZeneca's vaccine is not available in the United States and the Johnson & Johnson vaccine program has been placed on hold. Furthermore, VITT has not been reported in patients who received the Moderna or Pfizer vaccines. Overall, the available COVID-19 vaccines are very safe and highly effective at preventing COVID-19 infection. All patients should be encouraged to get their first available COVID-19 vaccine given the ongoing pandemic and known risks of COVID-19 infection. Finally, the apparent risk of VITT with a COVID-19 vaccine is greatly outweighed by the risk of complications from COVID-19 infection (including hospitalization, thrombosis and death).
Third, if a patient did receive the Johnson & Johnson vaccine, the presumed window of risk is narrow – between 5 and 28 days after vaccination. Based on our initial understanding of this condition, patients outside that window can be further reassured.
Finally, use of any medication to prevent VITT (e.g., aspirin) is not recommended. These events are extremely rare and there is no evidence that any medication would prevent them from occurring.
Where can I get more information?
Published References
- Greinacher A, et al. Thrombotic thrombocytopenia after ChAdOx1 nCov-19 vaccination. N Engl J Med 2021;April 9:[Epub ahead of print]. DOI: 10.1056/NEJMoa2104840
- Schultz NH, et al. Thrombosis and thrombocytopenia after ChAdOx1 nCoV-19 vaccination. N Engl J Med 2021;April 9:[Epub ahead of print]. DOI: 10.1056/NEJMoa2104882
- Muir KL, et al. Thrombotic thrombocytopenia after Ad26.COV2.S vaccination. N Engl J Med 2021;April 14:[Epub ahead of print]. DOI: 10.1056/NEJMc2105869
- Tacquet M, et al. Cerebral venous thrombosis: a retrospective cohort study of 513,284 confirmed COVID-19 cases and a comparison with 489,871 people receiving a COVID-19 mRNA vaccine. Preprint available here.
- Cines DB, Bussell JB. SAR-CoV-2 vaccine-induced immune thrombotic thrombocytopenia. N Engl J Med 2021;April 16:[Epub ahead of print]. DOI: 10.1056/NEJMe2106315
What are the considerations for cardiomyopathy and heart failure in COVID-19?
Category: CARDIAC COMPLICATIONS OF COVID
Patient Type: COVID+
Prevalence: MODERATELY COMMON
Principal Guidance: Cardiac dysfunction is moderately common among hospitalized patients with COVID-19 and confers a worse prognosis; focused imaging and other cardiac diagnostics are warranted to guide differential management; clinical management remains supportive although experimental strategies continue to be evaluated.
Author: Ashwin Ravichandran, MD, MPH, FACC; Joel Schilling, MD, PhD; Stacy Mandras, MD, FACC
SQC Approval Date: February 16, 2020
Both de novo cardiomyopathy and worsening of underlying cardiomyopathy can be observed with COVID-19.
Human cardiomyocytes express the viral entry receptor, ACE2, and can be directly infected by SARS-CoV-2. Growth of the virus can cause contractile dysfunction and death of cardiomyocytes. Autopsy studies have revealed evidence of replicating virus in cardiomyocytes.1,2
Myocarditis or inflammatory cardiac dysfunction should be considered in patients with COVID-19 who have elevated cardiac biomarkers with worsening hemodynamics and/or arrhythmias. Elevated NT-proBNP, elevated cardiac troponin and a history of preexisting heart failure are particularly important risk factors for mortality.3
An ECG should be employed to screen for evidence of ST-T wave changes.
Maintain a low threshold for point-of-care ultrasound in patients with the above clinical features.
If there is evidence of cardiac dysfunction, consider select views for transthoracic echocardiography to define left ventricular/right ventricular (LV/RV) size and function, wall motion abnormalities, and/or pericardial effusion.
Stable patients with suspected cardiovascular involvement should continue guideline-directed medical therapy for heart failure. Importantly, the BRACE CORONA trial demonstrates suspending ACE inhibitor/ARB in hospitalized patients was not associated with improvement in days alive AND out of the hospital through 30 days.
A high index of suspicion is necessary for diagnosis of myocarditis as the time course is variable. Cardiac MRI studies in patients who have recovered from COVID-19 suggest that cardiac involvement may be more frequent than suspected. Current data remain limited by selection bias and the inability to evaluate asymptomatic COVID-19 individuals.4
In patients with refractory shock, consider pulmonary artery catheterization to help guide the use of inotropes, vasopressors or mechanical support.
Patients with isolated RV dysfunction related to respiratory failure may benefit from pharmacological RV support with inotropic agents, selective pulmonary vasodilators or mechanical circulatory support/ECMO. Data are emerging regarding outcomes, cannulation strategies and duration of support for patients receiving ECMO for COVID-19.
Endomyocardial biopsy may have a role in differentiating stress-induced cardiomyopathy from inflammatory myocarditis, thus allowing for appropriate consideration for clinical trials of anti-inflammatory therapy. Current autopsy data suggest that the inflammatory infiltrate associated with COVID-19 is macrophage predominant with a minor T-cell infiltrate.1,5
Though hydroxychloroquine was widely adopted early in the pandemic due to its anti-inflammatory properties and in vitro studies suggesting antiviral activity, in a multicenter, blinded, randomized placebo-controlled trial, hydroxychloroquine did not improve clinical outcomes in patients hospitalized for COVID-19.6
An algorithm for evaluation and treatment of patients with COVID-19 and suspected myocarditis is included below and is available here.
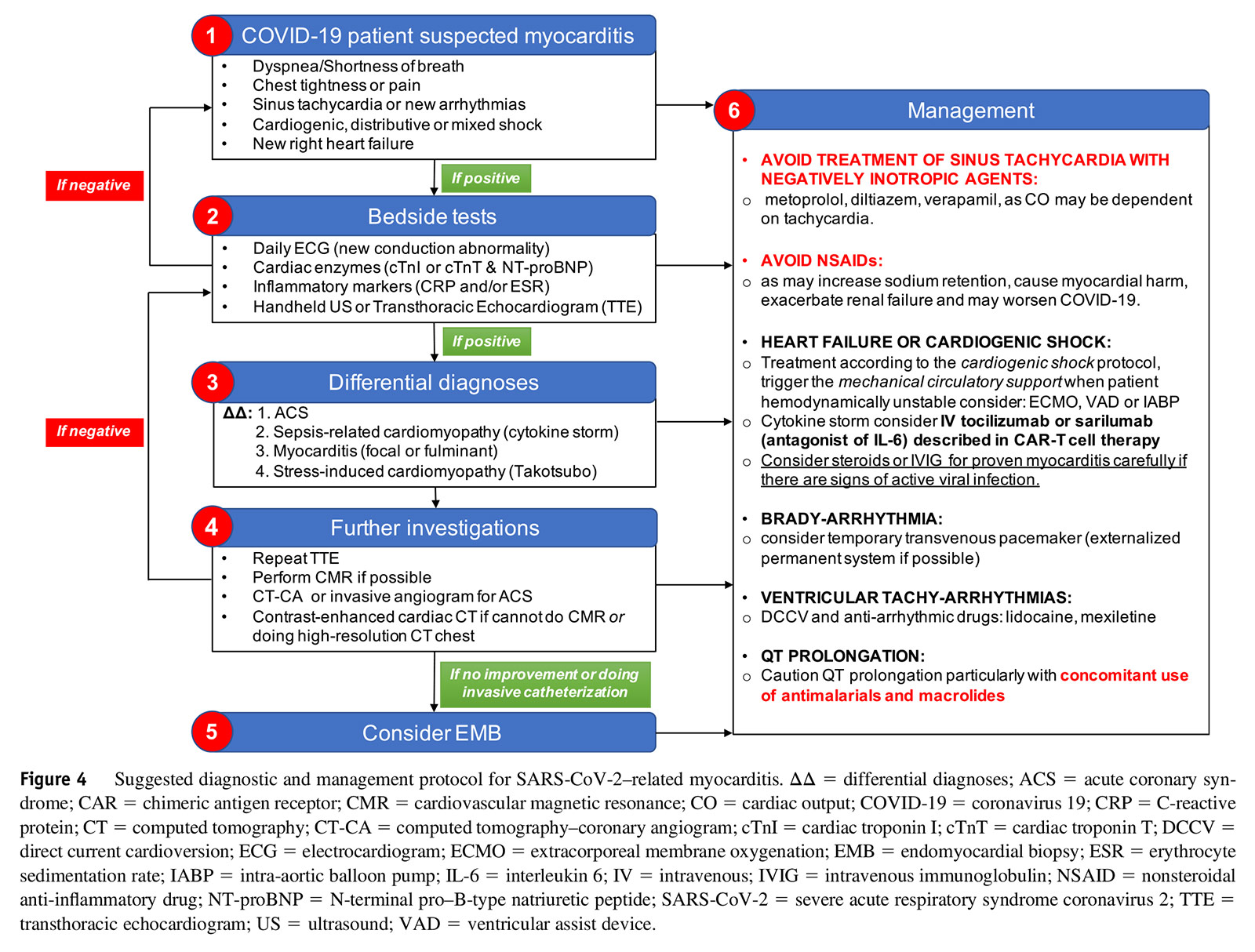 Reprinted from Heart Rhythm 2020;17:1463-71, with permission from Elsevier. Click the image above for a larger view.
Reprinted from Heart Rhythm 2020;17:1463-71, with permission from Elsevier. Click the image above for a larger view.
References
- Bailey AL, Dmytrenko O, Greenberg L, et al. SARS-CoV-2 infects human engineered heart tissues and models COVID-19 myocarditis. JACC Basic Transl Sci 2021;Feb 26:[Epub ahead of print].
- Sharma A, Garcia G Jr, Wang Y, et al. Human iPSC-derived cardiomyocytes are susceptible to SARS-CoV-2 infection. Cell Rep Med 2020;1(4):100052.
- Rey JR, Caro-Codon J, Rosillo SO, et al. Heart failure in COVID-19 patients: prevalence, incidence and prognostic implications. Eur J Heart Fail 2020;22:2205-15.
- Puntmann VO, Ludovica Carerj M, Wieters I, et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020;5:1265-73.
- Weckbach LT, Curta A, Bieber S, et al. Myocardial inflammation and dysfunction in COVID-19-associated myocardial injury. Circ Cardiovasc Imag 2021;Jan 19:[Epub ahead of print].
- Self WH, Semler MW, Leither LM, et al. Effect of hydroxychloroquine on clinical status at 14 days in hospitalized patients with COVID-19: a randomized clinical trial. JAMA 2020;324:2165-76
What are considerations for long-term management of COVID-19-related myocarditis?
Category: CARDIAC COMPLICATIONS OF COVID
Patient Type: COVID+
Prevalence: UNKNOWN
Principal Guidance: Clinical and imaging evidence indicates myocarditis may be present in patients recovering from COVID, though the prevalence and clinical significance remains uncertain; diagnosis should be reserved for patients exhibiting syndromic myocarditis and treatment should be in accordance with current guidelines for heart failure and arrhythmia; return to sport or strenuous exercise should be delayed for three to six months post diagnosis, conditional on nominal diagnostic findings.
Author: Jeffrey J. Hsu, MD, PhD, FACC
SQC Approval Date: February 16, 2020
Early in the COVID-19 pandemic, case reports of acute myocarditis raised concerns about the capacity and likelihood of the SARS-CoV-2 virus to directly invade the cardiomyocytes of infected patients.1–3 While this mechanism of myocardial injury remains an area of debate,4 the incidence of COVID-19-related myocarditis appears to be less common than initially feared.5 However, cardiac magnetic resonance imaging (CMR) studies in recovered COVID-19 patients have famously elicited further discussion about the prevalence of myocarditis in this population.6–8
While the clinical utility of these CMR findings alone is not entirely clear at this time, there are indeed patients who demonstrate the clinical syndrome of myocarditis during their recovery from COVID-19. One study found that 10% of patients hospitalized with COVID-19 were found to have a left ventricular ejection fraction (LVEF) <50%,9 slightly higher than the 5% prevalence of asymptomatic LV systolic dysfunction seen in similarly aged hospitalized patients.10 With more than 20 million people in the U.S. diagnosed with COVID-19 to date, the cardiology community will continue to see more recovered COVID-19 patients who carry a new diagnosis of myocarditis.
Data for optimal management of COVID-19-related myocarditis are currently lacking, but the general consensus at this time is to follow the AHA/ACC guidelines for the management of fulminant myocarditis for patients with an acute presentation in the setting of severe COVID-19.11 For recovered COVID-19 patients with ongoing evidence of myocarditis, guidelines and recommendations for heart failure and arrhythmia should be followed,12,13 with additional aspects discussed below.
While data are still emerging, it has been proposed that the diagnosis of myocarditis in recovered COVID-19 patients should be reserved for those who have a clinical syndrome of myocarditis, including symptoms (e.g., chest pain, dyspnea, exercise intolerance) and objective evidence of myocardial injury (e.g., serum troponin elevation, new arrhythmias or conduction abnormalities, LV wall motion abnormalities on echocardiography, characteristic inflammatory findings on CMR).14 While inflammatory features on CMR have been seen in patients recovering from COVID-196,7 and may help to support the diagnosis of myocarditis, we currently do not have enough data to support that these findings alone should be used to make the diagnosis in the absence of a clinical syndrome.14,15
An endomyocardial biopsy is not usually needed in this setting, though more data are needed to determine its utility in COVID-19-related myocarditis. Additionally, evaluation for significant epicardial coronary artery disease with coronary angiography (via computed tomography or cardiac catheterization) can be considered if clinical suspicion is high.
For recovered COVID-19 patients in the ambulatory setting with a diagnosis of myocarditis, an assessment of LVEF should be performed by transthoracic echocardiography or CMR, and guideline-directed medical therapy for heart failure initiated accordingly.12 There is inadequate evidence at this time to support the use of immunosuppressive or antiviral agents for the treatment of myocarditis in recovered COVID-19 patients, though it should be noted that there may be a role for corticosteroids in the treatment of myocarditis seen in pediatric patients with multisystem inflammatory syndrome in children (MIS-C).16 Biomarkers of myocardial injury (e.g., troponin, brain natriuretic peptide) and inflammation (e.g., C-reactive protein, erythrocyte sedimentation rate) may be helpful in the initial assessment and for monitoring trajectory during treatment and recovery, although there are no data at this time showing that such monitoring impacts outcomes in this population.
Due to concerns for myocarditis-related ventricular arrhythmias that may occur in the setting of ongoing inflammation, it is recommended that athletic patients avoid competition for three to six months after the initial diagnosis of COVID-19-related myocarditis.14,15 Return to competition can be considered after that time if LVEF and cardiac/inflammatory biomarkers have normalized and no concerning findings are seen on maximal exercise treadmill testing and ambulatory ECG monitoring. Similarly, non-athlete patients should refrain from strenuous exercise, with a similar workup performed prior to increasing the intensity of their exercise regimen. Notably, as a reminder, these recommendations are for those patients who have a clinical syndrome of myocarditis after COVID-19 diagnosis, and not for patients who have isolated imaging or biomarker abnormalities. Consideration for device therapy should follow the AHA/ACC guidelines for heart failure and arrhythmia management.12,13
Meanwhile, as we continue to learn more about the long-term cardiovascular sequelae of COVID-19, patients with related myocarditis should continue to be followed closely by a cardiologist, with implementation of newly recommended therapies and management strategies as they arise in clinical studies.
References
- Inciardi RM, Lupi L, Zaccone G, et al. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020;5:819.
- Hua A, O'Gallagher K, Sado D, Byrne J. Life-threatening cardiac tamponade complicating myo-pericarditis in COVID-19. Eur Heart J 2020;41:2130.
- Sala S, Peretto G, Gramegna M, et al. Acute myocarditis presenting as a reverse Tako-Tsubo syndrome in a patient with SARS-CoV-2 respiratory infection. Eur Heart J 2020;41:1861-2.
- Ozieranski K, Tyminska A, Jonik S, et al. Clinically suspected myocarditis in the course of severe acute respiratory syndrome novel coronavirus-2 infection: fact or fiction? J Card Fail 2021;27:92-6.
- Basso C, Leone O, Rizzo S, et al. Pathological features of COVID-19-associated myocardial injury: a multicentre cardiovascular pathology study. Eur Heart J 2020;41:3827-35.
- Puntmann VO, Carerj ML, Wieters I, et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020;5:1265-73.
- Rajpal S, Tong MS, Borchers J, et al. Cardiovascular magnetic resonance findings in competitive athletes recovering from COVID-19 infection. JAMA Cardiol 2021;6:116-8.
- Clark DE, Parikh A, Dendy JM, et al. COVID-19 myocardial pathology evaluation in AthleTEs with Cardiac Magnetic Resonance (COMPETE CMR). Circulation 2021;143:609-12.
- Szekely Y, Lichter Y, Taieb P, et al. Spectrum of cardiac manifestations in COVID-19: a systematic echocardiographic study. Circulation 2020;142:342-53.
- Martin LD, Mathews S, Ziegelstein RC, et al. Prevalence of asymptomatic left ventricular systolic dysfunction in at-risk medical inpatients. Am J Med 2013;126:68-73.
- Ommen SR, Mital S, Burke MA, et al. 2020 AHA/ACC Guideline for the Diagnosis and treatment of patients with hypertrophic cardiomyopathy: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol 2020;76:e159-e240.
- Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA Guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol 2017;70:776-803.
- Al-Khatib SM, Stevenson WG, Ackerman MJ, et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 2018;72:e91-e220.
- Kim JH, Levine BD, Phelan D, et al. Coronavirus disease 2019 and the athletic heart: emerging perspectives on pathology, risks, and return to play. JAMA Cardiol 2021;6:219-27.
- Maron BJ, Udelson JE, Bonow RO, et al. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: task force 3: hypertrophic cardiomyopathy, arrhythmogenic right ventricular cardiomyopathy and other cardiomyopathies, and myocarditis: A Scientific Statement from the American Heart Association and American College of Cardiology. J Am Coll Cardiol 2015;66:2362-71.
- Most ZM, Hendren N, Drazner MH, Perl TM. Striking similarities of multisystem inflammatory syndrome in children and a myocarditis-like syndrome in adults: overlapping manifestations of COVID-19. Circulation 2021;143:4-6.
What is home-based cardiac rehabilitation, and how could it be used during the COVID-19 pandemic?
Category: CV THERAPEUTICS
Patient Type: COVID+/COVID-
Prevalence: COMMON
Principal Guidance: Home-based cardiac rehabilitation (CR) has demonstrated comparable benefits to traditional hospital-based programs and may serve as a viable alternative during COVID-19; reimbursement for formal home-based CR programs is now more prevalent than early in the pandemic; the role of home-based CR for recovering COVID patients with cardiac sequelae is currently uncertain, at minimum requiring thorough physician evaluation before referral.
Author: Brittain Heindl, MD; Vera Bittner, MD, MSPH, FACC
SQC Approval Date: February 16, 2020
Cardiac rehabilitation (CR) combines patient education, health behavior modification, and exercise training to improve outcomes in patients with established cardiovascular disease. Clinical trials, observational studies and meta-analyses have shown that traditional center-based CR programs can reduce cardiovascular mortality, rehospitalization rates, and improve quality of life for adults with ischemic heart disease, heart failure, and after cardiac surgery.1 CR is recommended for the following groups (with evidence grade):2-4
- Within 12 months of a myocardial infarction (IA)
- Within 12 months of percutaneous coronary intervention (IA)
- Within 12 months of coronary artery bypass graft surgery (IA)
- In patients with chronic stable angina, who have not already participated in CR (IA)
- In patients with symptomatic peripheral arterial disease (IA)
- In patients with heart failure, not limited by phenotype or symptom burden (IIA).
The core interventions of center-based CR (ideally provided by a multidisciplinary team of a physician, nurse, exercise physiologist, dietitian, pharmacist, psychologist) include patient assessment (medical history, exam, functional assessment), exercise training, dietary counseling, medication adherence, risk factor management (with emphasis on smoking, blood pressure, lipids, weight, diabetes), and psychological support. The COVID-19 pandemic abruptly ended center-based programs for many. A transition to home-based CR was subsequently endorsed by multiple preventive cardiology societies.5-9 Home-based CR involves remote coaching and indirect exercise supervision, provided outside of the traditional center-based setting.
In the U.S., only the Veterans Affairs and Kaiser Permanente health systems have traditionally reimbursed for tele-rehabilitation services.10 Prior to the COVID-19 pandemic, home-based CR was not reimbursed by the Centers for Medicare and Medicaid Services (CMS), except when provided as part of home health services for homebound patients.5 However, as part of the Hospitals with Walls waiver, CMS has opened the door to reimbursement for the duration of the public health emergency as long as CR sessions are delivered using real-time interactive audio and video technology with all other CR requirements met, including hospital conditions of participation (CMS-5531-IFC, published May 8, 2020, Federal Register, Vol 85, No 90).
Standards previously established for center-based CR11 have been adapted, to varying degrees, by trial protocols evaluating home-based programs. The ideal home-based program includes three to five exercise sessions per week for eight to 12 weeks, with each core intervention addressed.12 Beneficial equipment may include a heart rate monitor, blood pressure monitor, bathroom scale and a pill box. Home-based protocols vary in degree of supervision, but appear to be safe for low-to-moderate risk patients.12
During the pandemic, eligible patients should continue to be referred to established CR centers. Many center-based programs may have already transitioned to a home-based or hybrid model. For communities without an established CR program, the core interventions can be addressed via online resources. Quality options include the UK Heart Manual,13 which is available digitally or via hard copy, and the University of Toronto CR website,14 which has online resources available to the public.
Many patients hospitalized for COVID-19 will develop indications for CR. Phenotypes described in the literature include type I and type II myocardial infarctions, myocarditis, myocardial injury and heart failure.15 It is unknown to what degree each might benefit from CR, how long after a diagnosis of COVID-19 it is safe to commence CR, or whether exercise prescriptions should be modified (especially in individuals with persistently positive troponins or abnormalities on cardiac imaging). For now, referrals of such patients to CR should be preceded by a thorough physician evaluation, including a clinician/patient discussion about potential benefits and risks.
References
- Anderson L, Taylor RS. Cardiac rehabilitation for people with heart disease: an overview of Cochrane systematic reviews. Cochrane Database Syst Rev 2014(12):CD011273.
- Drozda J Jr, Messer JV, Spertus J, et al. ACCF/AHA/AMA–PCPI performance measures for adults with coronary artery disease and hypertension. J Am Coll Cardiol 2011;58:316-36.
- Gerhard-Herman MD, Gornik HL, Barrett C, et al. 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2017;69:e71-e126.
- Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol 2017;70:776-803.
- Khera A, Baum SJ, Gluckman TJ, et al. Continuity of care and outpatient management for patients with and at high risk for cardiovascular disease during the COVID-19 pandemic: a scientific statement from the American Society for Preventive Cardiology. Am J Prev Cardiol 2020;1:100009.
- Kemps HMC, Brouwers RWM, Cramer MJ, et al. Recommendations on how to provide cardiac rehabilitation services during the COVID-19 pandemic. Neth Heart J 2020;28:387-90.
- Mureddu GF, Ambrosetti M, Venturini E, et al. Cardiac rehabilitation activities during the COVID-19 pandemic in Italy. Position Paper of the AICPR (Italian Association of Clinical Cardiology, Prevention and Rehabilitation). Monaldi Arch Chest Dis 2020;90(2).
- Nicholls SJ, Nelson M, Astley C, et al. Optimising secondary prevention and cardiac rehabilitation for atherosclerotic cardiovascular disease during the COVID-19 pandemic: a position statement from the Cardiac Society of Australia and New Zealand (CSANZ). Heart Lung Circ 2020;29:e99-e104.
- Scherrenberg M, Wilhelm M, Hansen D, et al. The future is now: a call for action for cardiac telerehabilitation in the COVID-19 pandemic from the secondary prevention and rehabilitation section of the European Association of Preventive Cardiology. Eur J Prev Cardiol 2020:2047487320939671.
- Scott-Sheldon LA, Gathright EC, Wu W-C. Promoting social connectedness among cardiac rehabilitation patients during the COVID-19 pandemic and beyond. R I Med J (2013) 2020;103(9):34-35.
- Balady GJ, Williams MA, Ades PA, et al. Core components of cardiac rehabilitation/secondary prevention programs: 2007 update: a scientific statement from the American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee, the Council on Clinical Cardiology; the Councils on Cardiovascular Nursing, Epidemiology and Prevention, and Nutrition, Physical Activity and Metabolism; and the American Association of Cardiovascular and Pulmonary Rehabilitation. Circulation 2007;115:2675-82.
- Thomas RJ, Beatty A, Beckie T, et al. Home-based cardiac rehabilitation: a scientific statement from the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. J Am Coll Cardiol 2019;74:133-53.
- The Heart Manual Programme (NHS Lothiam). Available here. Accessed Feb. 25, 2021.
- UHN Toronto Rehab Foundation Cardiac College. Available here. Accessed Feb. 25, 2021.
- Driggin E, Madhavan MV, Bikdeli B, et al. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol 2020;75:2352-71.
How best to use telehealth to manage CV conditions during the pandemic?
Category: CV THERAPEUTICS
Patient Type: COVID+/COVID-/CV
Prevalence: COMMON
Principal Guidance: Telehealth is now a permanent part of cardiovascular medicine, augmenting but not displacing traditional care delivery; effective telemedicine requires similar attention to workflow design and management, team-based care, and longitudinal follow-up as in-person care, adapted to the advantages and limitations of virtual patient interaction; expect rapid change as the provider, payer and technology ecosystem all adapt to increased telehealth demand.
Author: Ami Bhatt, MD, FACC
SQC Approval Date: February 16, 2020
Why TeleCardiology will last beyond the pandemic.
- Telehealth is not a disruptor of the practice of health care but rather it:
- augments the traditional delivery of health care
- enables a more agile and continuous mechanism of care provision
- engages the patient as an equal partner in their care.
- Outpatient cardiovascular care now includes: 1) in-person visits, 2) virtual synchronous visits between clinician and patient, 3) asynchronous communication (such as patient reported outcomes), 4) electronic consultation (between clinicians), and 5) remote monitoring, digital tracking, wearables and use of data.
- A blend of virtual and in-person visits ensures high-quality, safe care. The question is not whether to adopt telemedicine rather how to best use it in your practice.
- Sustainable telehealth implementation is possible. Ratios of care and use cases will vary based on clinician, disease entity and patient preference.
What are thrombosis risk and management considerations in COVID-19?
Category: COVID THERAPEUTICS
Patient Type: COVID+
Prevalence: MODERATELY COMMON
Principal Guidance: Thromboembolism risk in COVID-19 patients is sufficient to recommend pharmacological venous thromboembolism (VTE) prophylaxis in all hospitalized patients unless contraindicated; multiple randomized trials now suggest therapeutic-level anticoagulant dosing in hospitalized patients, unless otherwise clinically indicated, is of only modest and selective benefit; for example, non-ICU hospitalized patients receiving therapeutic dosing may be less likely to require later intensive care or organ support, while ICU patients do not appear to benefit from the higher dosing; VTE prophylaxis is generally not recommended in non-hospitalized and post-discharge COVID-19 populations given the much lower documented risk of VTE in the ambulatory setting, unless otherwise clinically warranted.
Authors: Geoffrey D. Barnes, MD, MSc, FACC; Gregory Piazza, MD, MS, FACC; Deborah Siegal, MD, MSc; Leben Tefera, MD; Barbara S. Wiggins, PharmD, BCPS, FACC
SQC Approval Date: Aug. 30, 2021
1. Should ambulatory (nonhospitalized) patients diagnosed with COVID-19 be given any antithrombotic therapy?
The risk of venous thromboembolism (VTE) in COVID-19 patients varies based on illness severity. In COVID-19 patients with mild symptoms who are deemed safe to recover at home, the observed rate of thrombotic events is low. As such, for nonhospitalized patients with COVID-19, antithrombotic and/or antiplatelet therapy should not be initiated solely for the prevention of thrombotic events. It should be noted however, that this only applies to patients without another indication for antithrombotic or antiplatelet therapy.
The randomized, double-blind, U.S. National Heart, Lung, and Blood Institute (NHLBI) sponsored study, ACTIV-4b (COVID-19 Outpatient Thrombosis Prevention Trial), enrolled ambulatory (nonhospitalized) patients who tested positive for COVID-19 with mild symptoms and randomized them (1:1:1) to apixaban 5 mg twice daily, apixaban 2.5 mg twice daily, or aspirin 81 mg once daily for the prevention of thrombotic events. In this study population, investigators found no thrombotic events after enrollment of 657 patients, leading to early trial termination.
There are no available data regarding the incidence of thrombotic events in nonhospitalized COVID-19 patients with a prior history of VTE with which to inform specific recommendations for this population. We recommend using this as an opportunity to review the signs and symptoms of acute VTE with patients and re-assess the appropriateness of secondary VTE prevention.
2. What antithrombotic strategy should be given to patients hospitalized for COVID-19 who do not require ICU-level care with organ support?
There have been two published trials evaluating different anticoagulant regimens in this population. The ACTION trial compared treatment-dose rivaroxaban 20 mg daily to prophylactic-dose enoxaparin 40 mg daily in hospitalized patients with COVID-19 and elevated D-dimer.1 The majority of these patients did not require intensive care unit (ICU)-level care organ support. There was no difference in the rate of death, duration of hospitalization, or duration of supplemental oxygenation between the two treatment groups.
In the multi-platform randomized controlled trial (ATTACC, ACTIV-4a, REMAP-CAP), patients with moderate illness from COVID-19 (hospitalized, but not requiring ICU-level care or organ support) were randomized to receive treatment-dose unfractionated heparin (UFH) or low molecular weight heparin (LMWH) or standard prophylactic dose UFH or LMWH heparin.2 This trial, which enrolled patients during the first waves of the COVID-19 pandemic (April 2020-January 2021) included an older population (mean age ~60 years) than is currently being hospitalized with the delta variant. The population was stratified by D-dimer level based on initial data suggesting a strong association with thromboembolic risk and outcomes. Importantly, the inclusion criteria were limited to patients hospitalized for COVID-19 infection with an expected length of stay of >48-72 hours and without the need for dual antiplatelet therapy or ongoing anticoagulant therapy. Patients requiring ICU-level organ support were not included in this analysis.
The main findings of the multi-platform trial are that the patients randomized to treatment-dose UFH or LMWH had more days without organ support than those randomized to prophylactic-dose UFH or LMWH (80.2% vs. 76.4%). However, there was no statistically significant difference in overall survival until discharge (adjusted risk difference, 1.3%; 95% CI, 1.1%-3.2%). Major thromboembolic events were slightly lower (1.1% vs. 2.1%) while major bleeding was higher (1.9% vs. 0.9%) in the treatment-dose group. Of note, in-hospital mortality was much more common (7.3%-8.2%) than major thrombotic event (1.1-2.1%).
A few points should be considered when applying the results to clinical practice. In this open-label trial, treating physicians were aware of treatment allocation which could lead to ascertainment bias (i.e., threshold for investigation of thrombosis and bleeding events) and/or differential use of other treatments (i.e., supportive treatments). It is unclear why the rates of thrombotic events (in both groups) were much lower than those reported in numerous previous observational studies.3 It is also unclear what proportion of thrombotic events were proximal vs. distal (e.g., below-the-knee deep vein thrombosis [DVT], subsegmental pulmonary embolism) a distinction which may be prognostically important. Finally, as this study was conducted early in the COVID-19 pandemic, it is possible that some patients were unable to get full imaging to diagnose thrombotic events due to concerns for patients and/or staff safety.
Based on current evidence, treatment-dose UFH or LMWH should be considered a therapy that reduces the need for ICU-level care but has not been shown to conclusively reduce thrombotic events among moderately ill hospitalized COVID-19 patients. In particular, treatment-dose UFH or LMWH may be most helpful for patients deemed at risk of disease progression or organ failure but at relatively low risk for bleeding complications. This approach may be particularly helpful in settings where the volume of patients with COVID-19 is great enough to overwhelm available ICU resources. Furthermore, no currently available biomarker is available to discern which patients are most likely to benefit from treatment-dose heparin therapy. Based on the results of the ACTION trial, the use of treatment-dose rivaroxaban cannot be recommended as a thromboprophylaxis strategy in hospitalized patients with COVID-19. Other ongoing and recently completed randomized trials may further define the role of treatment-dose UFH or LMWH for patients hospitalized with COVID-19.
3. What antithrombotic strategy should be given to patients hospitalized for COVID-19 who require ICU-level care or organ support?
Hospitalized patients with COVID-19 treated in the critical care setting have the highest risk of thromboembolic complications compared with those who are hospitalized but not requiring the ICU.4,5 While intermediate- or therapeutic-LMWH dosing was proposed for prophylaxis in this population early in the pandemic, some guidelines, such as from the American College of Chest Physicians (ACCP), suggested standard-dose LWMH based on the absence of randomized clinical trial data and concerns about an increased risk of bleeding with therapeutic dosing.6 In contrast, guidance from the International Society on Thrombosis and Haemostasis (ISTH) suggested that intermediate therapeutic-dose LMWH (1 mg/kg once daily) be considered for prophylaxis in high-risk patients with COVID-19.7 Part of the rationale for augmented dosing of thromboprophylaxis was that critically ill patients with COVID-19 may have in situ small vessel thrombosis, such as in the pulmonary vasculature, contributing to respiratory compromise.8,9
Early in 2021, several clinical trials were designed to provide clarity on the optimal dosing of thromboprophylaxis in patients with COVID-19 in the critical care setting. The INSPIRATION trial of 600 patients admitted to the ICU with COVID-19 showed that intermediate-dose prophylactic anticoagulation (enoxaparin 1 mg/kg daily), compared with standard-dose prophylactic anticoagulation (enoxaparin 40 mg daily), did not result in a significant difference in the primary outcome of a composite of adjudicated venous or arterial thrombosis, treatment with extracorporeal membrane oxygenation, or mortality within 30 days.10 Results from the multi-platform randomized clinical trial (REMAP-CAP, ACTIV-4a, ATTACC) demonstrated that therapeutic anticoagulation did not offer significant benefit over standard prophylactic dose anticoagulation for the primary outcome of organ support-free days.11 Furthermore, there was an increase in the rate of major bleeding among patients who were randomized to treatment-dose anticoagulation (3.8% vs. 2.3%). While thrombosis may be a key contributor to adverse outcomes in the ICU, other competing risks, such as infection and respiratory failure, are likely to play key roles such that therapeutic-dose antithrombotic therapy does not provide a net clinical benefit.
4. How should antithrombotic therapy be managed when patients transfer between the floor and ICU?
Early in the COVID-19 pandemic, intermediate- and treatment-dose anticoagulation was being utilized in many patients admitted to the ICU. However, since this time, multiple clinical trials have failed to prove benefit with these higher intensity anticoagulation regimens among these patients. Therefore, when patients are admitted to the ICU, standard thromboprophylaxis is generally recommended. Furthermore, the benefit of treatment-dose anticoagulation from the multi-platform randomized trials was largely for the prevention of ICU-level organ support.2 Additionally, when a patient's condition improves enough to no longer require ICU-level organ support, they are unlikely to realize benefit from treatment-dose anticoagulation. Therefore, most patients who transfer between the floor and the ICU can be treated with standard thromboprophylaxis. More data have become available that has failed to demonstrate benefit of these regimens compared to standard prophylaxis dosing. Should therapeutic dose or intermediate dose pharmacologic prophylaxis be utilized in COVID-19 patients admitted to the ICU, the doses should be modified to standard doses once the patients is transferred to the floor.
5. Should patients who are hospitalized with COVID-19 be given post-hospital antithrombotic therapy?
Current evidence from retrospective observational studies suggests that the risk of VTE after hospitalization for COVID-19 is low (0.14%-1.55%), which is similar with patients hospitalized for other acute medical illnesses.11-14 There are currently no validated risk prediction models to identify patients with COVID-19 who may be at higher risk of VTE after hospitalization and prospective studies are ongoing.
Post-discharge prophylactic dose anticoagulation reduces the risk of VTE after hospitalization for acute medical illness, but this is counterbalanced by a 2-fold increase in the risk of major bleeding. Based on current knowledge, the net clinical benefit of thromboprophylaxis after hospitalization for COVID-19 is not well established and its routine use is not recommended.
The eligibility criteria of recent trials evaluating thromboprophylaxis after hospitalization for acute medical illness (e.g., MARINER, MAGELLAN15,16) can be used to guide decisions regarding the use of thromboprophylaxis for select patients at low risk of bleeding, as recommended in current guidelines from the American Society of Hematology.17
6. In patients who develop VTE during a hospitalization for COVID-19, how long should anticoagulation be given?
Hospitalization is a well-known risk factor for the development of VTE. At the same time, most patients recover from their hospitalization and there is little ongoing risk of recurrent VTE beyond ~3 months following discharge. Therefore, most patients can be treated with a short course of anticoagulation when they develop a hospital-associated VTE event, even in the setting of COVID-19. This practice aligns with the most recent guideline recommendations from the American Society of Hematology.18
All patients with COVID-19 who develop hospital-associated VTE should receive therapeutic anticoagulation for a minimum of 3 months unless they are at prohibitively high bleeding risk. Direct oral anticoagulants are recommended as first-line therapy once the patient has been medically stabilized and should be started before hospital discharge. Warfarin can be considered as an alternative strategy in select patients (e.g., severe renal dysfunction, prohibitive cost, drug interactions). Most patients who develop hospital-associated VTE do not require ongoing secondary prevention for VTE following the initial 3-month period. However, in the presence of persistent risk factors (e.g., long-term immobility), longer courses of anticoagulation may be considered.
7. What does standard VTE prophylaxis mean for patients across the weight spectrum?
All patients hospitalized with COVID-19 should receive pharmacologic prophylaxis for VTE unless contraindicated (e.g., active bleeding) Current guidelines recommend standard prophylactic dosing of LMWH or UFH in most patients (those with creatinine clearance >30 mL/min and BMI <40 kg/m2) admitted with COVID-19-related illness in the absence of suspected or confirmed VTE using standard prophylactic dosing (e.g., enoxaparin 40 mg subcutaneously once daily, UFH 5000 units every 8 hours or every 12 hours).17 In the setting of heparin-induced thrombocytopenia, fondaparinux at a dose of 2.5 mg subcutaneously once daily may be used. The choice of agent will likely be determined by institutional guidelines and formularies.
Obese patients (BMI >40 kg/m2) may benefit from higher doses for VTE prophylaxis. The recommendation in this patient population is to consider increasing the dose of enoxaparin to 40 mg subcutaneously twice daily, provided renal function is normal.
A list of available drugs and doses for VTE prophylaxis is available in the American Society of Hematology (ASH) Guidelines.17
References
- Lopes RD, de Barros ESPGM, Furtado RHM, et al. Therapeutic versus prophylactic anticoagulation for patients admitted to hospital with COVID-19 and elevated D-dimer concentration (ACTION): an open-label, multicentre, randomised, controlled trial. Lancet 2021;397:2253-63.
- ATTACC Investigators, ACTIV-41 Investigators, REMAP-CAP Investigators, Lawler PR, Goligher EC, Berger JS, et al. Therapeutic anticoagulation with heparin in noncritically ill patients with Covid-19. N Engl J Med 2021;385:790-802.
- Jimenez D, Garcia-Sanchez A, Rali P, et al. Incidence of VTE and bleeding among hospitalized patients with coronavirus disease 2019: A systematic review and meta-analysis. Chest 2021;159:1182-96.
- Piazza G, Campia U, Hurwitz S, et al. Registry of arterial and venous thromboembolic complications in patients with COVID-19. J Am Coll Cardiol 2020;76:2060-72.
- Piazza G, Morrow DA. Diagnosis, management, and pathophysiology of arterial and venous thrombosis in COVID-19. JAMA 2020;324:2548-9.
- Moores LK, Tritschler T, Brosnahan S, et al. Prevention, diagnosis, and treatment of VTE in Patients with coronavirus disease 2019: CHEST Guideline and Expert Panel Report. Chest 2020;158:1143-63.
- Spyropoulos AC, Levy JH, Ageno W, et al. Scientific and Standardization Committee Communication: Clinical guidance on the diagnosis, prevention, and treatment of venous thromboembolism in hospitalized patients with COVID-19. J Thromb Haemost 2020;18:1859-65.
- Bikdeli B, Madhavan MV, Jimenez D, et al. COVID-19 and Thrombotic or thromboembolic disease: Implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J Am Coll Cardiol 2020;75:2950-73.
- Bikdeli B, Madhavan MV, Gupta A, et al. Pharmacological agents targeting thromboinflammation in COVID-19: Review and implications for future research. Thromb Haemost 2020;120:1004-24.
- INSPIRATION Investigators, Sadeghipour P, Talasaz AH, Rashidi F, et al. Effect of intermediate-dose vs standard-dose prophylactic anticoagulation on thrombotic events, extracorporeal membrane oxygenation treatment, or mortality among patients with COVID-19 admitted to the intensive care unit: The INSPIRATION randomized clinical trial. JAMA 2021;325:1620-30.
- Roberts LN, Whyte MB, Georgiou L, et al. Postdischarge venous thromboembolism following hospital admission with COVID-19. Blood 2020;136:1347-50.
- Patell R, Bogue T, Koshy A, et al. Postdischarge thrombosis and hemorrhage in patients with COVID-19. Blood 2020;136:1342-6.
- Giannis D, Allen SL, Tsang J, et al. Postdischarge thromboembolic outcomes and mortality of hospitalized patients with COVID-19: the CORE-19 registry. Blood 2021;137:2838-47.
- Hill JB, Garcia D, Crowther M, et al. Frequency of venous thromboembolism in 6513 patients with COVID-19: a retrospective study. Blood Adv 2020;4:5373-7.
- Cohen AT, Spiro TE, Buller HR, et al. Rivaroxaban for thromboprophylaxis in acutely ill medical patients. N Engl J Med 2013;368:513-23.
- Spyropoulos AC, Ageno W, Albers GW, et al. Rivaroxaban for Thromboprophylaxis after hospitalization for medical illness. N Engl J Med 2018;379:1118-27.
- Cuker A, Tseng EK, Nieuwlaat R, et al. American Society of Hematology 2021 guidelines on the use of anticoagulation for thromboprophylaxis in patients with COVID-19. Blood Adv 2021;5:872-88.
- Ortel TL, Neumann I, Ageno W, et al. American Society of Hematology 2020 guidelines for management of venous thromboembolism: treatment of deep vein thrombosis and pulmonary embolism. Blood Adv 2020;4:4693-738.
How can clinician wellness be maintained?
Category: CV WELL-BEING
Patient Type: HEALTH CARE WORKERS
Prevalence: COMMON
Principal Guidance: Clinicians should maintain self-care, cultivate their community, and practice self-compassion to preserve wellness during the pandemic; the buddy system may be helpful in monitoring for signs of workplace fatigue; additional resources are available from the ACC and other trustworthy sources, including where to seek professional help if necessary.
Authors: Laxmi S. Mehta, MD, FACC
SQC Approval Date: February 16, 2020
Clinicians are facing unprecedented conditions with the pandemic. As a result, clinicians are highly stressed and at risk of adverse mental health conditions. Recent survey data of health care workers from Mental Health America demonstrated a high prevalence of experiencing stress (93%), anxiety (86%), frustration (77%), exhaustion and burnout (76%). More than half reported physical symptoms of stress (headaches, stomachache), appetite change, and compassion fatigue. Self-care, both physical and emotional, is essential to caring for your patients, caring for your family and colleagues, and increasing your professional fulfillment, as well as reducing your risk of being overwhelmed by the onslaught of grim news, uncertainty and chaos.
It is critical to manage the pillars of your health, (nutrition, physical activity, sleep and social connection) to address your stress. Participation in exercise and hobbies can be helpful methods to combat stress and anxiety. Workplace fatigue can be reduced with getting adequate sleep and using a buddy system to monitor each other for signs of fatigue or increased work demands. Please refer to the CDC recommendations regarding workplace fatigue, found here.
Maintaining social connections with friends and family is important to avoid social isolation and can allow one to mentally separate from work. However, professional community is equally important. Clinicians participate in meaningful work with each other in teams and share a unique opportunity to support and share with each other, specifically in the care of patients and when they mourn the loss of patients, loved ones and colleagues. Expressing gratitude is more important now than ever before and can help improve clinician mood and optimism.
Furthermore, rather than self-criticizing when confronted with personal failure or feelings of inadequacy, it is necessary to practice self-compassion to prevent burnout. Those who are understanding and accepting of their imperfections and short comings have fewer negative emotions and are emotionally balanced during challenging situations. Everyone is challenged and struggling, especially as the period of stress, fear, uncertainty and loss extends indefinitely. It is important for clinicians to be as kind to themselves as they are to others in their personal and professional life.
Finally, while self-care is important to our well-being, personal resilience is one contributor to your well-being and professional fulfillment. The ACC recognizes the Stanford WellMD Professional Fulfillment Model which highlights efficiency of practice (workplace systems) and working in a culture of wellness (shared values prioritizing personal and professional growth) as important aspects of the well-being equation.
As part of its clinician well-being strategy, the ACC will continue to advocate for policies, practices and partnerships to improve wellness, reduce burnout and reduce the stigma of seeking mental health support as appropriate.
The ACC has provided resources for our members that address well-being, including COVID-related tips.
Examples from ACC's Clinician Well-being library include:
- Counseling Resources For Health Care Workers During COVID 19
- Tips to Cope With COVID-19 Stress
- Stress management Resources
- Resilience Building in Times of Crisis
- Crisis Communications For the CV Professional
- Self-Compassion Mantra to Ease Stress
- Mental Health and COVID Crisis: Developing Your Resilience Beyond Burnout
How best to manage CV operations (e.g., EP procedures, interventional cardiology procedures, etc.) during the pandemic?
Category: CV OPERATIONS
Patient Type: CV PATIENTS
Prevalence: COMMON
Principal Guidance: Under pressure to preserve inpatient capacity while protecting medical staff and non-COVID patients, many hospitals and health systems have adopted or expanded same-day discharge (SDD) for common cardiovascular procedures; SDD can also decrease costs and improve patient satisfaction; careful pre-planning and program management are essential to preserve quality and capture operational efficiencies.
Authors: Ginger Biesbrock, PA-C, MPH, MPAS, FACC
SQC Approval Date: February 16, 2020
The COVID pandemic of 2020 has brought an incredible amount of change as programs have worked hard to transform their care delivery models to minimize exposure for patients and staff, improve efficiency, and maintain high quality outcomes. The procedural areas have seen a similar transition with an increase in same-day discharge (SDD)of common cardiovascular procedures including percutaneous coronary intervention (PCI), device implants (pacer and ICD), and complex electrophysiology (EP) ablations.
The utilization of SDD has been proven to be safe for certain patient populations with a significant amount of research performed in the last decade.1-3 In addition, SDD for these procedures can decrease the cost of care, provide high patient satisfaction, and allow the previously utilized inpatient beds to be used for other patient types. These benefits are even more valuable in the middle of a pandemic. A MedAxiom listserv inquiry showed that several programs have increased their SDD for these procedures by as much as 70% when compared with 2019.
There are several key considerations to providing SDD in a controlled, safe environment:
- Effective SDD starts with defining which patient population would qualify for same-day discharge. The proceduralists should come together and decide on specific patient criteria that includes procedure type, comorbidities, and patient specific criteria such as socioeconomic and location considerations. Patient definitions and subsequent identification are the beginning of developing a strong protocol.
- SDD planning starts at the time the procedure is ordered. The ordering provider should discuss SDD as an option with the patient and outline expectations. Developing clinical decision tools to assist is a great best practice for reliable and effective patient identification.
- Smart procedural scheduling will assure that SDD is an option for the right patients. Identifying specific schedule blocks for SDD early in the day that allow for appropriate recovery monitoring and time is necessary.
- Pre-procedure planning that aligns both the ambulatory practice and the procedural teams is another best practice. Patient education, pre-procedure diagnostics, and patient instructions should all be aligned and provided to the patient prior day of procedure. This practice minimizes delays and cancellations.
- Post-procedure follow-up should be defined and scheduled as part of the pre-procedure process. SDD patients may need an early follow-up visit in addition to a next day phone call. Aligning and scheduling follow-up prior to the procedure day will improve compliance.
- Performance management for the SDD process is also a best practice. One key metric is to measure the percentage of patients who qualify for SDD vs. the percentage of patients who experience SDD. Second, patient tracking and follow-up to assure patient satisfaction and quality outcomes are maintained. Post-procedure emergency department visits and readmissions are important to track to assure the SDD process is safe and outcomes are optimal.
The COVID pandemic has forced many programs to re-address their use of same-day discharge. Some had never performed SDD while others had not realized the full potential of SDD for their patients. Most programs have increased their utilization of SDD significantly while adding other cardiovascular procedures beyond PCI, device implants and EP ablations. Programs are describing piloting SDD for TAVR, LAAO, and other structural heart procedures.
However, whether SDD is a consideration or not, the best practices outlined around patient definitions, process development, and performance management are key to effective procedural management. Creating an aligned, cohesive pre-procedure planning process will benefit all CV procedural patients regardless of SDD.
References
- Brayton KM, Patel VG, Stave C, et al. Same-day discharge after percutaneous coronary intervention. J Am Coll Cardiol 2013;62:275-85.
- Deyell MW, Leather RA, Macle L, et al. Efficacy and safety of same-day discharge for atrial fibrillation ablation. JACC: Clin Electrophysiol 2020;6:609-19.
- Hess PL, Greiner MA, Al-Khatib SM, et al. Same-day discharge and risks of mortality and readmission after elective icd placement for primary prevention. J Am Coll Cardiol 2015 65:955-7.
How should patients with cardiovascular conditions manage potential workplace exposure to COVID-19?
Category: COVID-19 PREVENTION
Patient Type: CV PATIENTS
Prevalence: COMMON
Principal Guidance: Patients with cardiovascular disease are at increased risk for severe COVID-19 and should be counseled to avoid exposure; if telework is not possible, all CDC-recommended public health measures should be stringently followed; vaccination is recommended upon availability.
Authors: Friederike Keating, MD, FACC; Joseph E. Marine, MD, FACC; Daniel M. Philbin, Jr., MD, FACC
SQC Approval Date: February 16, 2020
Patients with cardiovascular conditions who are at higher risk for complications from COVID-19,1 such as those over the age of 50 or with marginal clinical compensation, should be counseled to avoid environments that would increase the risk of SARS-CoV-2 exposure. It is reasonable for cardiovascular specialists to advise those patients and their employers about workplace mitigation strategies such as:
- Using face masks as advised by the Centers of Disease Control and Prevention (CDC) Guidance.
- Minimizing close contact between employees (particularly in situations that interfere with donning masks or with marginal ventilation, such as eating together in break rooms).
- Rearranging workflow to allow the maintenance of a six-foot distance between workers, customers, and visitors.
- Working remotely, when possible.
All employees, particularly those with cardiovascular conditions, should be encouraged to undertake vaccination against SARS-CoV-2 when available. The ACC Health Policy Statement on Cardiovascular Disease Considerations for COVID-19 Vaccine Prioritization is available here.
For patients who work in health care settings, minimizing direct exposure to COVID-19 should be attempted. Lastly, all patients with cardiovascular illnesses should be assured of adequate personal protective equipment appropriate to their work environment. Please refer to the CDC recommendations regarding workplace accommodations, found here.
Reference
- Larochelle MR. Is it safe for me to go to work? Risk stratification for workers during the COVID-19 pandemic. N Engl J Med 2020; 383:e28.
Clinical Topics: Acute Coronary Syndromes, Anticoagulation Management, Arrhythmias and Clinical EP, Cardiac Surgery, Congenital Heart Disease and Pediatric Cardiology, COVID-19 Hub, Diabetes and Cardiometabolic Disease, Dyslipidemia, Geriatric Cardiology, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Pericardial Disease, Prevention, Pulmonary Hypertension and Venous Thromboembolism, Sports and Exercise Cardiology, Stable Ischemic Heart Disease, Valvular Heart Disease, Vascular Medicine, Anticoagulation Management and ACS, Implantable Devices, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Cardiac Surgery and Arrhythmias, Cardiac Surgery and CHD and Pediatrics, Cardiac Surgery and Heart Failure, Cardiac Surgery and SIHD, Cardiac Surgery and VHD, Congenital Heart Disease, CHD and Pediatrics and Arrhythmias, CHD and Pediatrics and Imaging, CHD and Pediatrics and Interventions, CHD and Pediatrics and Prevention, Acute Heart Failure, Pulmonary Hypertension, Interventions and ACS, Interventions and Imaging, Interventions and Structural Heart Disease, Interventions and Vascular Medicine, Angiography, Nuclear Imaging, Hypertension, Sleep Apnea, Sports and Exercise and Congenital Heart Disease and Pediatric Cardiology, Sports and Exercise and ECG and Stress Testing, Sports and Exercise and Imaging, Chronic Angina
Keywords: Acute Coronary Syndrome, Anticoagulants, Arrhythmias, Cardiac, Cardiac Surgical Procedures, Metabolic Syndrome, Angina, Stable, Heart Defects, Congenital, Dyslipidemias, Geriatrics, Heart Failure, Angiography, Diagnostic Imaging, Pericarditis, Secondary Prevention, Hypertension, Pulmonary, Sleep Apnea Syndromes, Sports, Angina, Stable, Exercise Test, Heart Valve Diseases, Aneurysm, COVID-19, Coronavirus, Coronavirus Infections, Cardiology Magazine, ACC Publications
< Back to Listings