Feature | Interventional Imagers and Radiation Safety

Exposure to ionizing radiation has become an accepted occupational risk related to cardiac interventions. As the field has advanced and procedures have become more complex, the heart team has expanded to include anesthesiologists, cardiovascular surgeons and ancillary staff members. In concert with each of these additions, contemporary research has explored the members’ radiation exposure and methods through which it can be minimized. The interventional echocardiographer is a key player on every structural heart team. In the March issue of the Journal of the American College of Cardiology (JACC), James A. Crowhurst, BS, et al., studied radiation exposure of the interventional echocardiographer, a previously under-recognized entity.
The authors noted that radiation exposure of the TEE operator (TEEO) was not significantly different than that of the primary interventional cardiologist (2.62 μSv vs. 1.91 μSv , respectively). They further implemented and measured the effect of operator position and additional shielding techniques through which the TEEO exposure could be reduced by 82 percent. While shielding was the primary method of reducing radiation exposure, attention should have also been paid to the other fundamental methods of dose reduction such as time and distance. Innovative methods that implement the basic radiation safety principles of time, distance and shielding should be optimized to limit exposure in accordance with the “ALARA” principle — As Low As Reasonably Achievable. Designing cardiac laboratory shielding with the ALARA principle in mind for every team member and coordinating active cardiac imaging times are two major opportunities to limit exposure.
Cardiac Lab Design
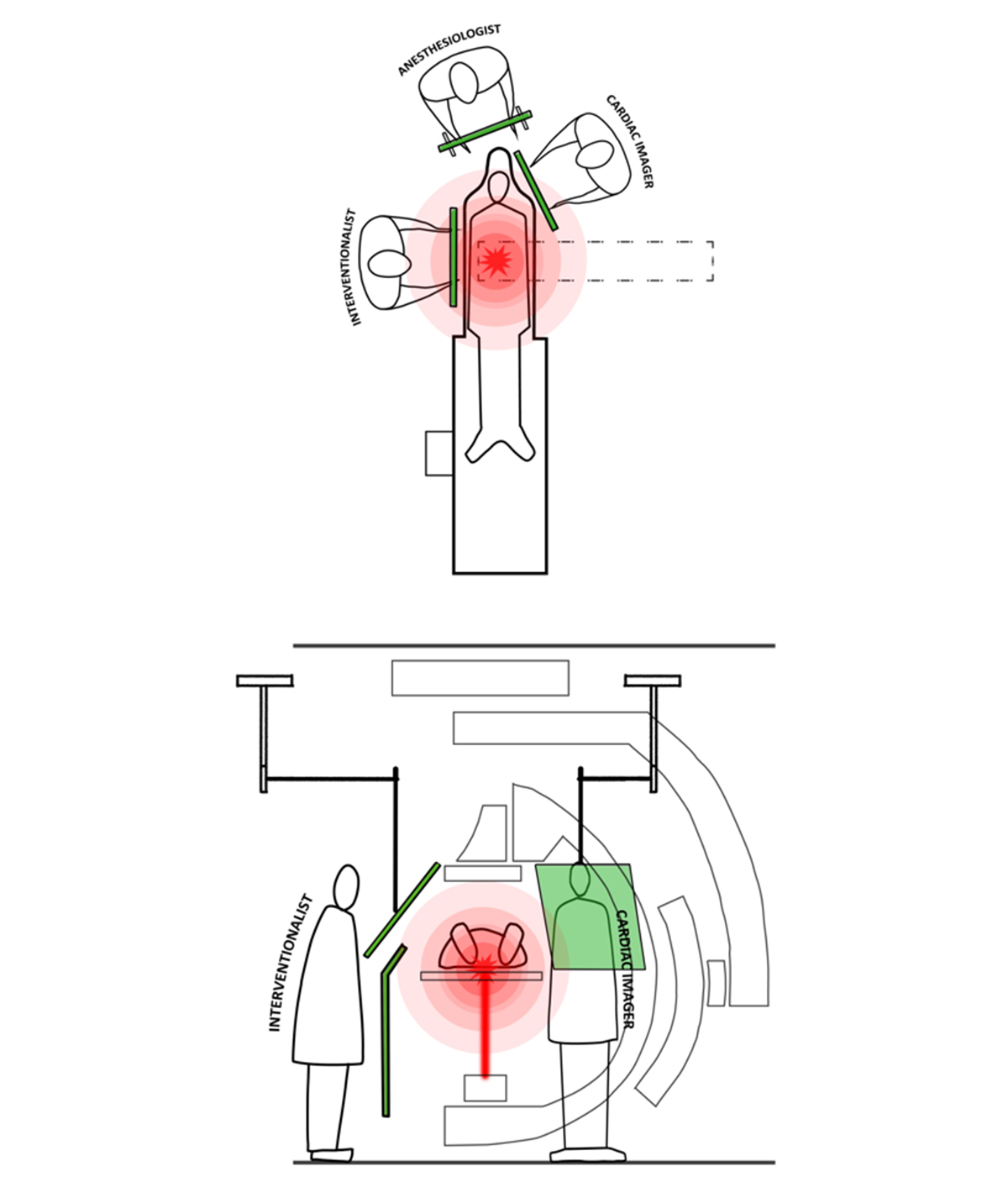
The design of hybrid cardiac interventional laboratories has become increasingly important given the growing numbers of structural heart disease cases. Early iterations focused on having enough space to accommodate multiple operating room tables and multiple standalone cardiac support devices, with their numerous diagnostic cables and cannulas. However, from a radiation safety perspective, the key in design seems to be identifying the position of each operator and developing an appropriate and effective shielding solution (Figure 1).
Plans inclusive of the interventional echocardiographer at the patient’s side are critical to an optimal design. Interventional imagers are often the closest provider to the x-ray beam source and, in many cases, the patient. While the x-ray beam is highly collimated from the source, a key concept in shielding is to protect the providers — both interventionalists and imagers — from scatter (Figure 1). Most cardiac images are positioned in the “northeast” corner of the table to allow a machine to be rolled into place. The ceiling-mounted shield suggested by Chowhurst and colleagues has become standard for interventionalist use but has not yet been integrated into standard lab design to protect the cardiac imager. The number of ceiling-mounted lights and monitors may limit the available real estate for an additional shield.
Coordinated Cardiac Imaging
Within the cardiac interventional lab, the common goal of the multidisciplinary team is a successful procedure. By creating a more coordinated acquisition protocol for structural interventional procedures, the TEEO is increasingly free to leave their position tethered to the patient by the TEE probe and move to the outskirts of the room — potentially to stand behind a full-length shield elsewhere.
In an editorial comment published in JACC, John W. Hirshfeld Jr., MD, FACC, et al., suggested increasing the distance (length of the TEE probe) from the patient as a non-shielding technique to reduce exposure, with another possibility being a robotic remote-controlled TEE probe. While these may be effective at reducing dose by increasing distance, as a cardiovascular imager it seems that communication is paramount and coordinating efforts is the key. Depending on the procedure, there are only certain moments where simultaneous direct manipulation of the TEE probe and cinefluoroscopic imaging are needed. With ALARA principles in mind, these coordinated efforts can be effective at reducing time and distance for the TEEO.
Advanced techniques that employ fused interventional imaging during structural interventions can potentially reduce overall fluoroscopy time. This can be accomplished with echocardiographic or computed tomography imaging that is registered to fluoroscopy at the time of the procedure. Using this technique can allow the imager to establish a fused image and potentially step further away from the x-ray source and patient while the co-registered images guide the interventionalist, thereby reducing the simultaneous imaging time at short distances from the patient.
Expert Consensus
The 2018 ACC/HRS/NASCI/SCAI/SCCT Expert Consensus Document on Optimal Use of Ionizing Radiation in Cardiovascular Imaging: Best Practices For Safety and Effectiveness was recently published in JACC. Writing committee members provided the comprehensive document on the above concepts in radiation safety inside and outside of the interventional lab and across imaging modalities, from nuclear cardiology to x-ray fluoroscopy and computer tomography. Given that most interventional echocardiographers are multi-modality imagers, these radiation safety and exposure concepts are important as we work to minimize the ionizing radiation exposure to ourselves and our patients.
This article was authored by Pravin Patil, MD, FACC, cardiologist at Lewis Katz School of Medicine at Temple University in Philadelphia, PA, and Russell Rosenberg, MD, Fellow in Training at Temple University Hospital in Philadelphia, PA.