Perfusion Imaging With CMR for the Assessment of Ischemic Heart Disease
A 64-year-old male patient with a history of ischemic heart disease, several risk factors for coronary artery disease (dyslipidemia, smoking, hypertension, and diabetes mellitus type 2), chronic kidney disease stage 3b, anemia, and paroxysmal atrial fibrillation was referred for further evaluation due to recurrent stable chest pain and novel abnormalities in the standard 12-lead electrocardiogram (ECG).
The patient had undergone two-vessel coronary artery bypass grafting 14 years earlier that included a saphenous vein graft to the left circumflex artery and the left internal mammary artery to the left anterior descending artery (LAD). This was followed by percutaneous coronary intervention of the LAD with stent implantation 1 year later.
On admission, the patient had mild chest pain on exertion (Canadian Cardiovascular Society grade II), fatigue, and exertional dyspnea. Physical examination was normal. The ECG demonstrated sinus rhythm with new T-wave inversions in the inferolateral leads. Echocardiography demonstrated normal regional wall motion and left ventricular (LV) ejection fraction (60%).
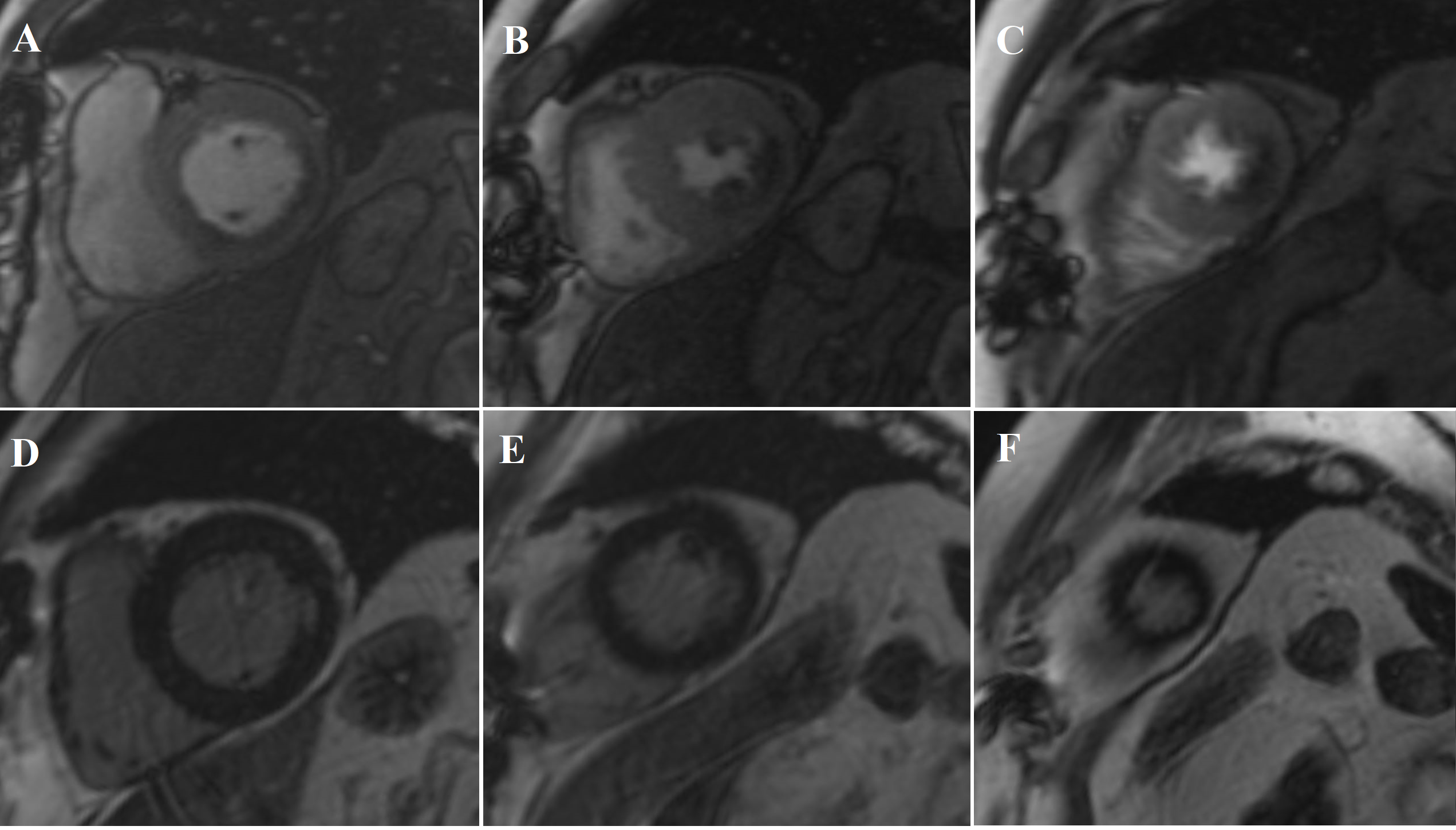
Cardiovascular magnetic resonance (CMR) with cine imaging, scar imaging (late gadolinium enhancement [LGE]), and perfusion CMR during regadenoson stress were performed. The cine images showed borderline increased LV volumes with normal global LV systolic function (ejection fraction = 60%) without regional wall motion abnormalities. Right ventricular volumes and global systolic right ventricular function were normal. In the LGE images, an ischemic subendocardial scar in the basal-medial inferolateral segments with a maximum of 50% transmurality was found. Perfusion imaging demonstrated myocardial ischemia with a transmurality of 50-75% in the basal inferoseptal, inferior, and inferolateral; medial inferior and inferolateral; and apical inferior segments (9 of 32 subsegments total: basal = 3 subendocardial segments [3 subsegments]; mid = 2 transmural segments [4 subsegments]; apex = 1 transmural segment [2 subsegments]). The ischemic area during stress extended well beyond the scar seen in the LGE images, covering >10% of non-infarcted myocardium. Based on the CMR findings, the patient was referred for invasive coronary angiography because an ischemic burden of >10% myocardium or any peri-infarct ischemia is regarded as prognostically relevant; therefore, revascularization was recommended. During invasive angiography, a mid-distal total occlusion of the circumflex artery and a high-grade stenosis of the right coronary artery were found. The right coronary artery lesion was stented. A follow-up perfusion CMR is planned to assess the amount of remaining myocardial ischemia.
Figure 1
Video 1
Video 2
Video 3
Which of the following statements about perfusion CMR is true?
Show Answer