Approaches to Echocardiographic Assessment of Left Ventricular Mass: What Does Echocardiography Add?
Introduction
Left ventricular mass (LVM) is a well-established measure that can independently predict adverse cardiovascular events and premature death.1-3 Population-based studies have revealed that increased LVM and left ventricular hypertrophy (LVH) as assessed by two-dimensional (2D) M-mode echocardiography measurements provide prognostic information beyond traditional cardiovascular disease (CVD) risk factors.4-6 In the pioneering Framingham Heart Study, after adjusting for age and traditional risk factors, the relative risk for coronary disease per 50 g/m increment in LVM was 1.67 in men and 1.60 in women.4 Similarly, in the Cardiovascular Health Study's elderly cohort, the multiple-risks-adjusted hazard ratio for the highest quartile of gender-specific LVM was 3.36 compared to the lowest quartile.5 Additionally, a low traditional CVD risk profile in young adults has been associated with lower LVM and, consequently, lower CV morbidity and mortality.7 Therefore, LVM has been touted as a suitable measure for CVD risk stratification and a marker for subclinical disease.4,8 Moreover, the regression of LVH in patients with hypertension treated with antihypertensive medication, or after aortic valve replacement in patients with severe aortic valve stenosis, has been associated with improved CVD outcomes.9,10
Key Factors Affecting LVM
LVM is strongly influenced by body size. However, even after adjustment for anthropometric variables, males have larger LVM than females.11 Similarly, athletes have increased LVM compared to nonathletes,12 and black men and women have larger LVM than their white or Asian counterparts.11,13 Likewise, obesity is associated with increased LVM. The aforementioned body size- , ethnic-, and exercise-related factors are associated with increased LVM, as well as proportional increases in left ventricular (LV) volume, which initially maintains normal LV wall stress.12 Consequently, LV relative wall thickness (RWT), defined as the ratio of twice the LV inferolateral wall thickness to the LV internal diameter measured at end-diastole, initially remains unchanged. Other factors to be considered are age and blood pressure.
Body Size Indexation Methods for LVM
Normal values for LVM are derived from studies of the general population without hypertension or obesity.12,14 Separate cutoff values for body size-adjusted LVM have been used for men and women.12,15 In order to allow comparison of LVM among subjects of different body sizes, different allometric approaches have been suggested to normalize LVM.14 However, there is controversy about the best method for indexing LVM.
Body surface area (BSA) was the first anthropometric variable used to index LVM and has shown a stronger statistical correlation than height with LVM16 and better identification of hypertension-related LVH.17 However, indexing by BSA has been noted to minimize the effect of obesity on LVM, and, therefore, it underestimates the prevalence of obesity-related LVH.18 Consequently, height has also been used for indexing (either height alone or height raised to an allometric power of 1.7 or 2.7).15,18-20 Indexation of LVM to height raised to an allometric exponent of 2.7 (LVM/height2.7), in comparison to BSA or height alone, has shown better predictive value for CVD outcomes, better detection of obesity-related LVH, and less variability of LVM among normal individuals.19,21 Chirinos et al. demonstrated that indexation to LVM/height1.7 was the best method, in comparison to BSA and height2.7, to identify obesity-related LVH and was more consistently associated with CVD outcomes and all-cause mortality.15 In a population with a low prevalence of obesity, there was no significant difference in the risk attributed to LVH regardless of the method of indexation.20 BSA has been widely adopted by the American Society of Echocardiography (ASE) and European Association of Cardiovascular Imaging as the preferred method for indexing LVM.14
Echocardiography LVM Measurements Method and Comparison to Cardiovascular Magnetic Resonance (CMR)
Given the clinical importance of LVM, it is essential to have a reliable method for its estimation. Echocardiography offers a reliable, noninvasive, rapidly available, and relatively inexpensive method for estimation of LVM. Regardless of the method used, LVM estimation is derived by converting myocardial volume to mass by multiplying the volume by the myocardial density of 1.05 g/mL.14
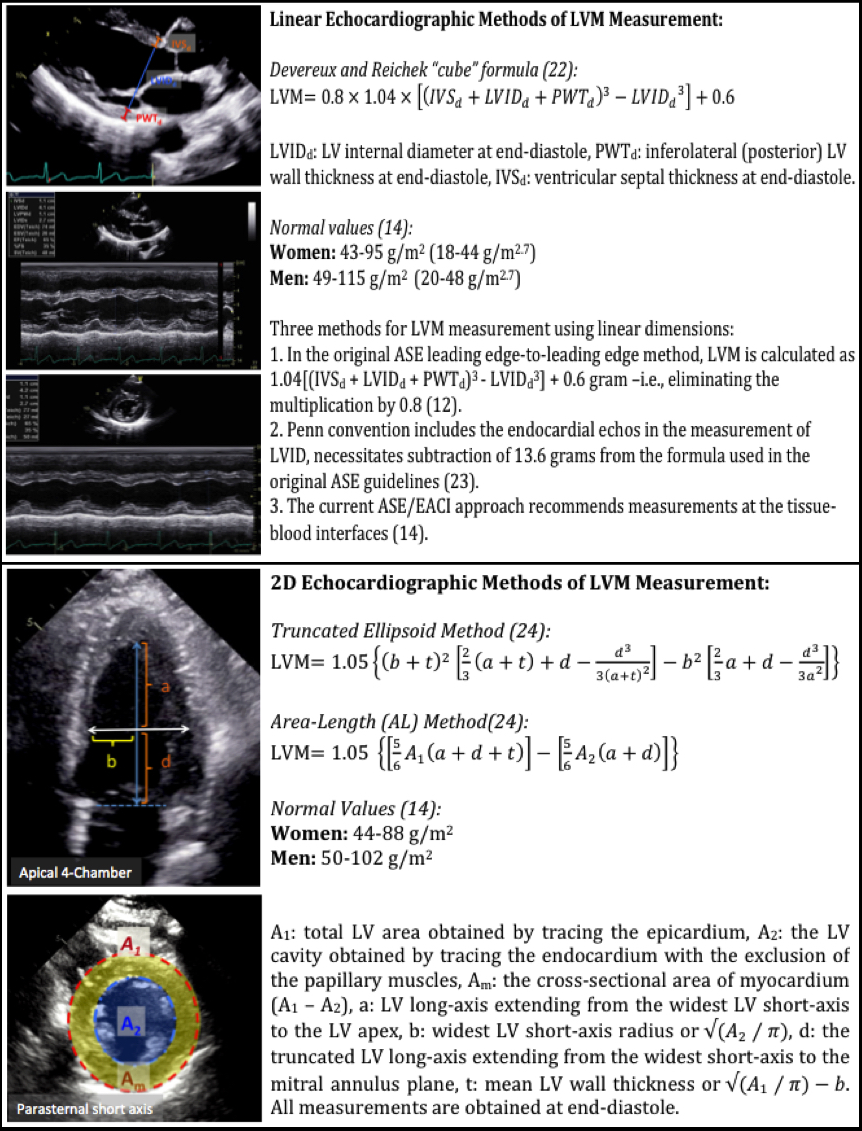
The first and most commonly used echocardiography method of LVM estimation is the linear method, which uses end-diastolic linear measurements of the interventricular septum (IVSd), LV inferolateral wall thickness, and LV internal diameter derived from 2D-guided M-mode or direct 2D echocardiography. This method utilizes the Devereux and Reichek "cube" formula, which assumes a prolate ellipsoid shape of the LV with a ratio of 1:2 minor- to major-axis (Figure 1).22 The cube formula includes a 20% correction based on overestimation of LVM in prior validation studies.14
It is essential to acquire LV images at end-diastole with the ultrasound beam directed perpendicular to the LV long axis approximately at the level of the mitral valve leaflet tips from either a parasternal long-axis or short-axis view.12 Additionally, the values for LV thickness obtained by direct 2D might be smaller than those obtained by M-mode; therefore, normal values for LVM might be not interchangeable.14 The current ASE and European Association of Cardiovascular Imaging Chamber Quantification Guidelines recommend the use of the LV tissue-blood interface for LVM measurement and propose normal values derived from this approach (Figure 1).12,14,23 Because of its simplicity, easy acquisition, and lower measured variability, the ASE and the European Association of Cardiovascular Imaging recommended that the linear method (2D-guided M-mode or direct 2D) be implemented as the best screening technique for LVH. Additionally, most of the data about the prognostic value of LVM are based on this method. However, any error in linear measurements can result in significant inaccuracies because all measurements are cubed in the LVM formula. This formula is also not accurate in asymmetric LVH, dilated cardiomyopathy, and other conditions with regional differences in LV wall thickness.14
Figure 1: Linear and 2D Echocardiographic Methods of LVM Measurement
The most commonly used 2D echocardiography methods for LVM estimation are the area-length and truncated ellipsoid methods.14 In both, the area is measured at the midpapillary level in the parasternal short-axis view and at end-diastole (Figure 1).24 Postmortem data have demonstrated that both 2D echocardiography methods (area-length and truncated ellipsoid) and 2D-guided M-mode measurements of LVM were comparable, with modest correlations with autopsy-derived LVM (r = 0.66-0.72 for 2D echocardiography and r = 0.78 for 2D-guided M-mode).25 They also demonstrated that both area-length- and truncated ellipsoid-derived LVM were comparable in their correlation with autopsy LVM, and the inclusion of papillary muscles in the area measurements tended to overestimate LVM.25
A limitation of the 2D methods is that they rely on geometrical assumptions that are not applicable when there are major LV distortions or when the LV is foreshortened.12 Moreover, in comparison to the M-mode, the 2D methods require better echocardiography windows to identify endocardial and epicardial borders.24 Normal reference values for LVM indices using 2D echocardiography are listed in Figure 1.14
The last echocardiography method for measuring LVM is the utilization of real-time 3-D imaging. Real-time 3D echocardiography relies on direct measurement of the LV without geometric assumptions; therefore, it can theoretically provide a more accurate estimation of LVM than linear M-mode or 2D methods. Additionally, real-time 3D estimation of LVM has shown better agreement with CMR measurements than 2D direct and M-mode echocardiography measurements.26-27 Real-time 3D assessment of LVM demonstrated excellent correlation with CMR data with a Pearson's correlation coefficient (r) of 0.99, in comparison to the 2D method versus CMR, which had an r of 0.84.26 Similarly, the interobserver and intraobserver variability of real-time 3D measurements were 7% and 8%, respectively, which were significantly better than the interobserver and intraobserver variability of the 2D method (37% and 19%, respectively).27 In addition, LVM values by real-time 3D reportedly were similar to CMR values with only a minimal bias of 4 grams.27 Therefore, the real-time 3D technique improves the accuracy and reproducibility of echocardiography estimation of LVM but is highly dependent on the equipment used and the quality of the images obtained.14 ASE and European Association of Cardiovascular Imaging Chamber Quantification Guidelines did not provide normal reference values for real-time-3D-derived LVM because of limited published data.14
Classification of LV Remodeling Patterns
Traditionally, LV has been classified into four mutually exclusive patterns according to LV geometry assessed by RWT and the presence or absence of LVH defined by an LVM index >115 g/m2 for men or >95 g/m2 for women (Figure 2).1 This traditional classification, which has been adopted by the ASE and the European Association of Cardiovascular Imaging, has disadvantages related to the use of linear measurements to reflect a 3D LV structure. In addition, the traditional approach does not identify isolated changes in LV size or LV thickness because RWT is a ratio.
Figure 2: Left Ventricular Geometric Patterns: Classification Systems
In an attempt to develop a classification that is more inclusive of different physiologic and pathologic remodeling phenotypes, Gaasch and Zile suggested including LV end-diastolic volume as an additional marker to identify LV dilatation (Figure 2).28 This classification provided incremental prognostic value regarding CVD outcomes in the Cardiovascular Health Study cohort.29
In another attempt to address the limitations associated with the traditional remodeling classification, Khouri et al. suggested a four-tiered classification of LVH (Figure 2).30 The four-tiered classification was evaluated in the Dallas Heart Study over a mean follow-up of 9 years and successfully stratified LVH into subgroups with differential prognosis. Dilated LVH and mixed thick and dilated LVH carried the worst prognosis for heart failure or CV death, and indeterminate hypertrophy had comparable rates to those without LVH.31
References
- Koren MJ, Devereux RB, Casale PN, et al. Relation of left ventricular mass and geometry to morbidity and mortality in uncomplicated essential hypertension. Ann Intern Med 1991;114:345-52.
- Drazner MH, Rame JE, Marino EK et al. Increased left ventricular mass is a risk factor for the development of a depressed left ventricular ejection fraction within five years: the Cardiovascular Health Study. J Am Coll Cardiol 2004;43:2207-15.
- Verma A, Meris A, Skali H, et al. Prognostic implications of left ventricular mass and geometry following myocardial infarction: the VALIANT (VALsartan In Acute myocardial iNfarcTion) Echocardiographic Study. JACC Cardiovasc Imaging 2008;1:582-91.
- Levy D, Garrison RJ, Savage DD, et al. Left ventricular mass and incidence of coronary heart disease in an elderly cohort. The Framingham Heart Study. Ann Intern Med 1989;110:101-7.
- Gardin JM, McClelland R, Kitzman D, et al. M-mode echocardiographic predictors of six- to seven-year incidence of coronary heart disease, stroke, congestive heart failure, and mortality in an elderly cohort (the Cardiovascular Health Study). Am J Cardiol 2001;87:1051-7.
- Verdecchia P, Carini G, Circo A, et al. Left ventricular mass and cardiovascular morbidity in essential hypertension: the MAVI study. J Am Coll Cardiol 2001;38:1829-35.
- Gidding SS, Carnethon MR, Daniels S, et al. Low cardiovascular risk is associated with favorable left ventricular mass, left ventricular relative wall thickness, and left atrial size: the CARDIA study. J Am Soc Echocardiogr 2010;23:816-22.
- Devereux RB, Alderman MH. Role of preclinical cardiovascular disease in the evolution from risk factor exposure to development of morbid events. Circulation 1993;88:1444-55.
- Verdecchia P, Schillaci G, Borgioni C, et al. Prognostic significance of serial changes in left ventricular mass in essential hypertension. Circulation 1998;97:48-54.
- Hatani T, Kitai T, Murai R, et al. Associations of residual left ventricular and left atrial remodeling with clinical outcomes in patients after aortic valve replacement for severe aortic stenosis. J Cardiol 2015 Oct 30. [Epub ahead of print].
- Gardin JM, Wagenknecht LE, Anton-Culver H, et al. Relationship of cardiovascular risk factors to echocardiographic left ventricular mass in healthy young black and white adult men and women. The CARDIA study. Coronary Artery Risk Development in Young Adults. Circulation 1995;92:380-7.
- Marwick TH, Gillebert TC, Aurigemma G, et al. Recommendations on the Use of Echocardiography in Adult Hypertension: A Report from the European Association of Cardiovascular Imaging (EACVI) and the American Society of Echocardiography (ASE). J Am Soc Echocardiogr 2015;28:727-54.
- Poppe KK, Doughty RN, Gardin JM, et al.; on behalf of the Echocardiographic Normal Ranges Meta-Analysis of the Left Heart Collaboration. Ethnic-Specific Normative Reference Values for Echocardiographic LA and LV Size, LV Mass, and Systolic Function: The EchoNoRMAL Study. JACC Cardiovasc Imaging 2015;8:656-65.
- Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 2015;28:1-39.e14.
- Chirinos JA, Segers P, De Buyzere ML, et al. Left ventricular mass: allometric scaling, normative values, effect of obesity, and prognostic performance. Hypertension 2010;56:91-8.
- Gardin JM, Arnold A, Gottdiener JS, et al. Left ventricular mass in the elderly. The Cardiovascular Health Study. Hypertension 1997;29:1095-103.
- Ferrara LA, Vaccaro O, Cardoni O, et al. Indexation criteria of ventricular mass and predictive role of blood pressure and body composition. Am J Hypertens 2005;18:1282-7.
- Cuspidi C, Giudici V, Negri F, et al. Improving cardiovascular risk stratification in essential hypertensive patients by indexing left ventricular mass to height(2.7). J Hypertens 2009;27:2465-71.
- de Simone G, Daniels SR, Devereux RB, et al. Left ventricular mass and body size in normotensive children and adults: assessment of allometric relations and impact of overweight. J Am Coll Cardiol 1992;20:1251-60.
- de Simone G, Devereux RB, Maggioni AP, et al. Different normalizations for body size and population attributable risk of left ventricular hypertrophy: the MAVI study. Am J Hypertens 2005;18:1288-93.
- de Simone G, Kizer JR, Chinali M, et al. Normalization for body size and population-attributable risk of left ventricular hypertrophy: the Strong Heart Study. Am J Hypertens 2005;18:191-6.
- Devereux RB, Reichek N. Echocardiographic determination of left ventricular mass in man. Anatomic validation of the method. Circulation 1977;55:613-8.
- Deague JA, Wilson CM, Grigg LE, et al. Discrepancies between echocardiographic measurements of left ventricular mass in a healthy adult population. Clin Sci (Lond) 1999;97:377-83.
- Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 2005;18:1440-63.
- Park SH, Shub C, Nobrega TP, et al. Two-dimensional echocardiographic calculation of left ventricular mass as recommended by the American Society of Echocardiography: correlation with autopsy and M-mode echocardiography. J Am Soc Echocardiogr 1996;9:119-28.
- Chuang ML, Beaudin RA, Riley MF, et al. Three-dimensional echocardiographic measurement of left ventricular mass: comparison with magnetic resonance imaging and two-dimensional echocardiographic determinations in man. Int J Card Imaging 2000;16:347-57.
- Mor-Avi V, Sugeng L, Weinert L, et al. Fast measurement of left ventricular mass with real-time three-dimensional echocardiography: comparison with magnetic resonance imaging. Circulation 2004;110:1814-8.
- Gaasch WH, Zile MR. Left ventricular structural remodeling in health and disease: with special emphasis on volume, mass, and geometry. J Am Coll Cardiol 2011;58:1733-40.
- Zile MR, Gaasch WH, Patel K, et al. Adverse left ventricular remodeling in community-dwelling older adults predicts incident heart failure and mortality. JACC Heart Fail 2014;2:512-22.
- Khouri MG, Peshock RM, Ayers CR, et al. A 4-tiered classification of left ventricular hypertrophy based on left ventricular geometry: the Dallas heart study. Circ Cardiovasc Imaging 2010;3:164-71.
- Garg S, de Lemos JA, Ayers C, et al. Association of a 4-Tiered Classification of LV Hypertrophy With Adverse CV Outcomes in the General Population. JACC Cardiovasc Imaging 2015;8:1034-41.
Keywords: African Americans, Antihypertensive Agents, Aortic Valve, Aortic Valve Stenosis, Athletes, Autopsy, Blood Pressure, Body Size, Body Surface Area, Cardiomyopathy, Dilated, Cohort Studies, Coronary Disease, Diastole, Dilatation, Echocardiography, Echocardiography, Three-Dimensional, Hypertension, Hypertrophy, Left Ventricular, Magnetic Resonance Spectroscopy, Mitral Valve, Mortality, Premature, Obesity, Observer Variation, Papillary Muscles, Phenotype, Phosmet, Prevalence, Prognosis, Reference Values, Reproducibility of Results, Risk Factors, Ventricular Remodeling
< Back to Listings