Clinical Outcomes Using CCTA and FFRCT-Guided Management of Patients With Stable Chest Pain
Introduction
Coronary computed tomographic angiography (CCTA) is an established noninvasive test of coronary anatomy that can be used for the detection of coronary plaque and, in particular, the exclusion of obstructive coronary artery stenosis. The strength of this investigation mainly lies in its high negative predictive value of approximately 99%.1 As such, it is currently recommended for patients without known coronary artery disease (CAD)2 and is felt to be particularly useful in the low-intermediate pre-test probability group.3 Historically, CCTA has been considered to be limited by a relatively low positive predictive value and poor correlation with functional significance.1 However, recent clinical trials utilising CCTA in patients with chest pain have demonstrated its diagnostic value, including clinical outcome benefit.4,5
Ideally, the routine investigation of patients with chest pain would establish the presence or absence of atheromatous CAD (in which case they will benefit from disease-modifying medical treatment), as well as the presence or absence of myocardial ischaemia in those with CAD. Increasingly, evidence suggests that ischaemia provides the most robust target for revascularisation.
In recent years, it has become possible to complement the anatomical assessment provided by CCTA with functional data that represent ischaemia. A post-processing technique named fractional flow reserve (FFR) by coronary CTA, or FFRCT, has been developed by HeartFlow (Redwood City, California, USA) and uses computational fluid dynamics applied to a standard CCTA dataset to provide FFRCT data on all major epicardial vessels.
FFRCT has been successfully validated against invasive coronary angiography (ICA) and pressure wire assessment and shows considerable promise as a test for the diagnosis and management of patients presenting with chest pain. Ongoing randomised trials will provide essential evidence of the potential role for FFRCT in routine clinical practice.
Clinical Trials
Validation
It is now well-established that the selection of lesions for percutaneous coronary intervention (PCI) by FFR6-8 (and instantaneous wave-free ratio9,10) is superior in terms of cost, efficacy, and clinical outcome compared with an angiogram-directed strategy. Furthermore, an increasingly large body of observational data indicates that using FFR routinely at the diagnostic-angiogram stage has a profound effect upon the labelling of vessels as having "significant" disease (i.e., targets for revascularisation) and therefore on management of patients.11 Further, the 1,100 patient randomised RIPCORD 2 (In the Management of Coronary Artery Disease, Does Routine Pressure Wire Assessment at the Time of Coronary Angiography Affect Management Strategy, Hospital Costs and Outcomes?) trial has compared isolated angiographic assessment and management of stable patients and those with non-ST elevation myocardial infarction (MI) with angiogram plus routine FFR of all major epicardial vessels as the determinant of assessment and management, looking at both resource utilisation and clinical outcome, and will report later this year.12
On the back of this evidence, the ability to assess both coronary anatomy and physiological surrogates for ischaemia in one noninvasive test, FFRCT, offers a new diagnostic approach for patients presenting with chest pain.
The DISCOVER-FLOW (Diagnosis of Ischemia-Causing Stenoses Obtained Via Noninvasive Fractional Flow Reserve) and DEFACTO (Determination of Fractional Flow Reserve by Anatomic Computed Tomographic Angiography) studies compared the performance of the first iteration of FFRCT against invasive angiography and FFR in patients with suspected or known CAD and found accuracies of 84.6%13 and 73%,14 respectively. A second iteration of the FFRCT algorithm was tested against invasive angiography with FFR in 251 patients with suspected CAD in the NXT (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps) study. This reported that the diagnostic accuracy, sensitivity, specificity, positive predictive value, and negative predictive value for FFRCT on a per-patient basis was 81%, 86%, 79%, 65%, and 93%, respectively.15
Subsequently, a meta-analysis involving 609 patients and 1,050 vessels included in the 3 studies described above concluded that FFRCT improves the diagnostic accuracy of CCTA alone with an area under the curve of 0.89 at patient level and 0.88 at vessel level compared with 0.74 for CCTA at patient level.16
The potential impact on clinical decision-making was assessed in the FFRCT RIPCORD (Does Routine Pressure Wire Assessment Influence Management Strategy at Coronary Angiography for Diagnosis of Chest Pain?) study.17 A consensus assessment was made for each CCTA in 200 consecutive patients in the NXT trial, which aimed to identify "significant" lesions and, as a result, a management plan for each case. After this, the FFRCT data were revealed for each patient, and the number of significant lesions were analysed by consensus and the resultant management plan derived. In 36% of cases, the initial CCTA-based management plan was changed after FFRCT data were revealed.
Clinical Studies
PLATFORM (Prospective Longitudinal Trial of FFRCT: Outcome and Resource Impacts) was a prospective cohort study involving 584 patients with new onset chest pain and intermediate likelihood of CAD divided into planned invasive and noninvasive arms. It was designed as a non-randomised comparative study of usual care versus FFRCT. In the group of patients who were considered to have an indication for ICA, the primary endpoint of ICA showing no obstructive CAD was 73% in the routine0care group versus 12% in the FFRCT arm.18 Importantly, there were no adverse clinical events at 1 year in the patients in whom ICA was deferred based upon the FFRCT data, thus indicating that such deferral is safe.19
Although a CCTA strategy did not improve outcomes at 2 years in the initial PROMISE (Prospective Multicenter Imaging Study for Evaluation of Chest Pain trial),20 a substudy that retrospectively assessed FFRCT in 67% of the eligible patients demonstrated that the availability of these data led to a significantly better association with major adverse cardiac events (MACE) or revascularization compared with visual assessment by CCTA alone (hazard ratio 4.3; 95% confidence interval, 2.4-8.9 vs. hazard ratio 2.9; 95% confidence interval, 1.8-5.1; p = 0.033). Further, reserving an invasive strategy for patients with FFRCT < 0.8 decreased the rate of finding unobstructed coronaries at ICA by 44%, at the same time increasing the rate of revascularisation in those patients by 24%.
The ADVANCE registry (Assessing Diagnostic Value of Non-invasive FFRCT in Coronary Care) included 5,083 patients with symptoms suggestive of angina from 38 centres in Europe, North America, and Japan. Overall, there was a change in the management pathway in 66% of patients after FFRCT data were available compared with CCTA alone. Further, non-obstructive coronary disease was much less frequently found on ICA in patients with FFRCT > 0.8 when compared with FFRCT < 0.8 (14.4% vs. 43.8%). Finally, at 90 days follow-up, the rate of death or MI in those who had FFRCT > 0.8 was 0% compared with 0.3% in the group of those who had FFRCT < 0.8.
A recently published Danish single centre observational study included 3,674 patients with suspected CAD who had CCTA with FFRCT for stenoses between 30% and 90%. Patients with FFRCT > 0.8 had similar clinical outcomes to patients without obstructive disease on CCTA (<30%). By contrast, patients with FFRCT < 0.8 had significantly more MACE (9.6% vs 1.4%).21
In summary, these data consistently demonstrate that FFRCT significantly alters the assessment of the presence of "significant" coronary disease and therefore management of patients in over 25% of cases and that deferring invasive angiography in FFRCT-negative patients, even those with CAD on CCTA, appears to be safe.
Economic Impact
Analyses from existing studies have offered promising results in terms of the potential cost efficacy of a FFRCT strategy. Estimates based on data from the DISCOVER FLOW trial projected a 30% reduction in costs at 1 year when using CCTA/ FFRCT /ICA versus ICA/visual strategy ($7,674 vs. $10,702).22 The PLATFORM trial included a pre-specified economic evaluation that demonstrated reduced mean 1-year per patient costs with CCTA/FFRCT compared with invasive usual care ($8,127 vs. $12,145) in the group who would be committed to ICA.19 In the United Kingdom, a retrospective analysis of patients attending Rapid Access Chest Pain Clinics demonstrated that using FFRCT for lesions between 10% and 90% could save potentially £200 per patient.23
Regulatory Approval and Clinical Guidance
The US Food and Drug Administration (FDA) granted HeartFlow de novo clearance for FFRCT in November 2013 as a "post-processing software for the clinical quantitative and qualitative analysis of previously acquired Computed Tomography (CT)… for clinically stable symptomatic patients with coronary artery disease... to support the functional evaluation of coronary artery disease."24
In the United Kingdom, current National Institute for Clinical Excellence (NICE) Clinical Guidance 95 recommends CCTA as first-line investigation for chest pain in patients without known CAD. Further, after an independent appraisal, Medical Technologies Guidance MTG32 published in February 2017 recommends considering FFRCT as an option "for patients with stable, recent onset chest pain who are offered CCTA as part of the NICE pathway on chest pain." By implementing this method, the National Health Service England hopes to save £9 million by 2022, predominantly by avoiding invasive investigations and treatments.
Limitations of FFRCT
HeartFlow requires patient data transfer offsite to be post-processed by the company. This raises two limitations. First, it introduces a delay of approximately 24 hours to obtain a result. Second, confidentiality is ensured by "black-boxing" patients' details and then re-coupling the results on repatriation. This carries important information governance issues that are easily surmountable but are unfortunately dealt with at individual trust level, hence introducing delays into adoption.
Another limitation, which would be common to any CCTA-dependent platform, is that some CCTA raw data will be of insufficient quality to allow for FFRCT processing. For example, in the NXT and PLATFORM studies, 13% and 12% of CCTA data, respectively, were deemed unsuitable for FFRCT analysis mostly due to artefacts. This raises the possibility that real-world rejection rates are likely to be higher.
Future Trial Data
The FORECAST (Fractional Flow Reserve Derived From Computed Tomography Coronary Angiography in the Assessment and Management of Stable Chest Pain) trial is a 1,400 patient multicentre randomised trial currently recruiting in the United Kingdom that is assessing routine assessment and management of patients presenting with new onset stable chest pain versus a strategy of CCTA with FFRCT. The primary endpoint is resource utilisation, and prespecified endpoints include MACE and clinical events. Two further randomised trial of FFRCT are currently being organised in the United States.
Alternative Technologies
Although at present HeartFlow FFRCT is the only FDA- and NICE-approved method, there are several other vendors developing similar techniques.
Siemens cFFR (Siemens Healthineers; Erlangen, Germany) uses a similar but simpler method based on CCTA images. It uses only one-dimensional modelling, has lower spatial resolution, and requires manual coronary boundaries measurement. However, it uses desktop computer stations, thus allowing for faster results without the need for patient data transfer.
Canon Medical Systems Corporation (formerly Toshiba Medical, Ōtawara, Tochigi, Japan) has developed a four-dimensional FFR method involving four-dimensional computed tomography tracking. The image processing and fluid simulation are done onsite. However, it does require a 320-slice computed tomography scanner compared with only 64-slice computed tomography required by HeartFlow FFRCT.25
Summary
Groundbreaking and innovative bioengineering principles, coupled with clinical study evidence, yield a test that offers promise as a noninvasive assessment of coronary anatomy and physiology, and that may dramatically and safely reduce the requirement for invasive angiography and pressure wire measurement. Although already being used in the clinical arena, further data, particularly in the form of randomised clinical trials, are now required.
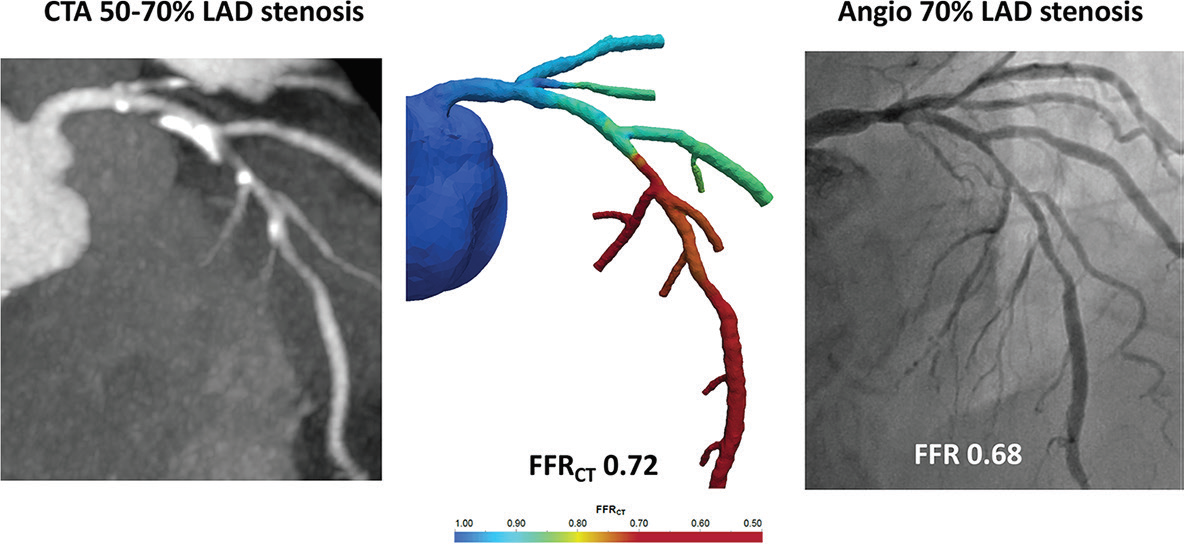
FFRCT Example
A 72-year-old man with typical chest pain and cardiovascular risk factors for diabetes mellitus, hypertension, hyperlipidaemia, and smoking underwent CCTA. This showed a moderate calcified plaque (50-70%) within the mid left anterior descending artery (LAD). The FFRCT value of the LAD was 0.72, and the patient was subsequently referred for angiography and PCI. Invasive FFR was concordant with the FFRCT value, and PCI was subsequently performed.
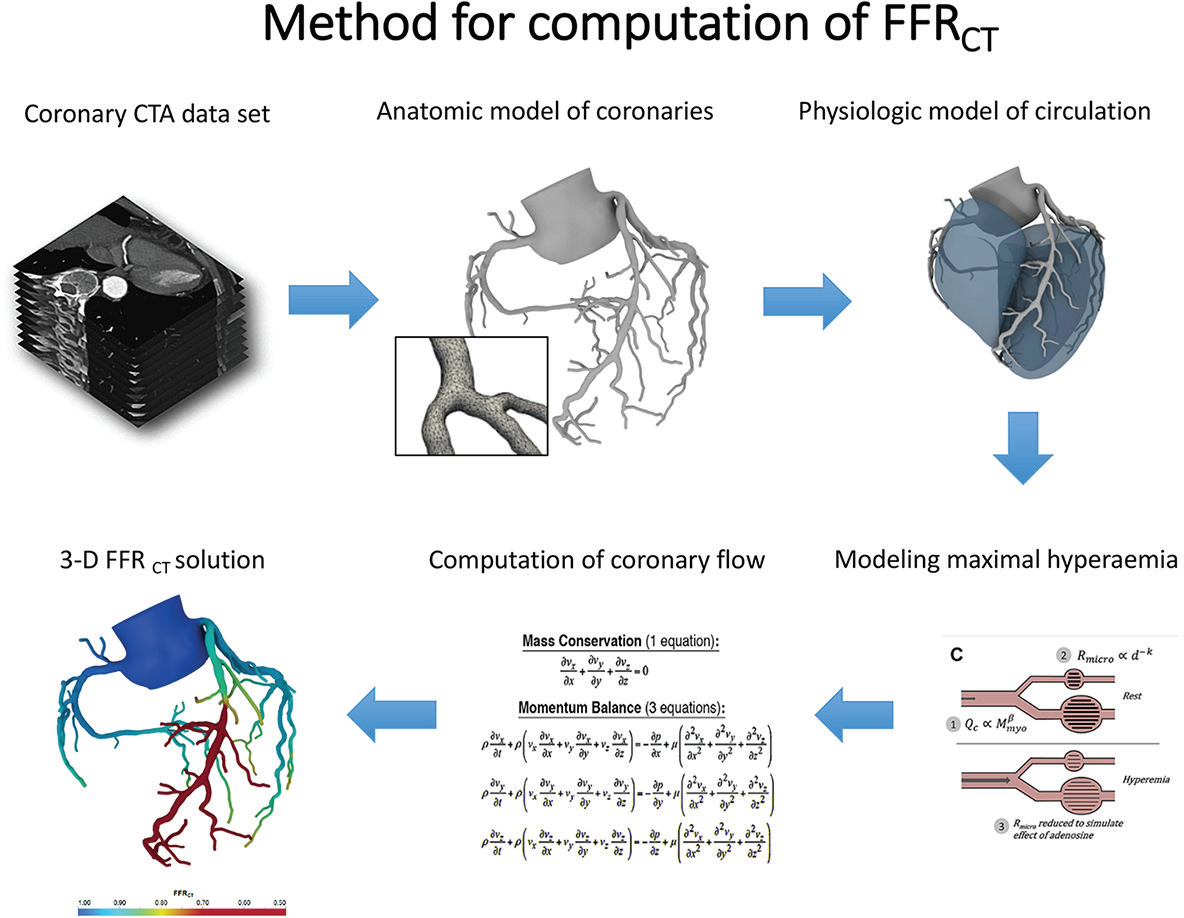
Method of Computation of FFRCT
- CCTA image data set, acquired using standard imaging protocol, without additional medications.
- Anatomic model of aortic root and coronary arteries, including second-order and third-order branchings. Construction of tetrahedral mesh resulting in millions of continuous discrete points for computation of coronary pressure and flow, including branch points.
- Physiologic model of coronary circulation with specified inflow and outflow boundary conditions. Resting coronary flow is based on myocardial mass.
- Modelling of maximal hyperaemia to reflect expected reduction in peripheral resistance resulting from adenosine administration.
- Numerical solution of Navier-Stokes equations that govern the fluid dynamics of blood flow. Fractional flow reserve is computed as coronary pressure divided by aortic pressure under simulated maximal hyperaemia.
- Three-dimensional solution of FFRCT throughout the coronary artery tree.
References
- Budoff MJ, Dowe D, Jollis JG, et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol 2008;52:1724-32.
- NICE Clinical Guideline CG 95: Chest pain of recent onset: assessment and diagnosis (NICE website). March 2010, last updated November 2016. Available at https://www.nice.org.uk/guidance/cg95. Accessed February 6, 2019.
- Taylor AJ, Cerqueira M, Hodgson JM, et al. ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 appropriate use criteria for cardiac computed tomography. A report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. J Am Coll Cardiol 2010;56:1864-94.
- SCOT-HEART investigators. CT coronary angiography in patients with suspected angina due to coronary heart disease (SCOT-HEART): an open-label, parallel-group, multicentre trial. Lancet 2015;385:2383-91.
- SCOT-HEART Investigators, Newby DE, Adamson PD, et al. Coronary CT Angiography and 5-Year Risk of Myocardial Infarction. N Engl J Med 2018;379:924-33.
- Bech GJ, De Bruyne B, Pijls NH, et al. Fractional flow reserve to determine the appropriateness of angioplasty in moderate coronary stenosis: a randomized trial. Circulation 2001;103:2928-34.
- Tonino PA, De Bruyne B, Pijls NH, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med 2009;360:213-24.
- De Bruyne B, Pijls NH, Kalesan B, et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med 2012;367:991-1001.
- Götberg M, Christiansen EH, Gudmundsdottir IJ, et al. Instantaneous Wave-free Ratio versus Fractional Flow Reserve to Guide PCI. N Engl J Med 2017;376:1813-23.
- Davies JE, Sen S, Dehbi HM, et al. Use of the Instantaneous Wave-free Ratio or Fractional Flow Reserve in PCI. N Engl J Med 2017;376:1824-34.
- Nagaraja V, Mamas M, Mahmoudi M, Rogers C, Curzen N. Change in angiogram-derived management strategy of patients with chest pain when some FFR data are available: How consistent is the effect? Cardiovasc Revasc Med 2017;18:320-7.
- Elguindy M, Stables R, Nicholas Z, Kemp I, Curzen N. Design and Rationale of the RIPCORD 2 Trial (Does Routine Pressure Wire Assessment Influence Management Strategy at Coronary Angiography for Diagnosis of Chest Pain?): A Randomized Controlled Trial to Compare Routine Pressure Wire Assessment With Conventional Angiography in the Management of Patients With Coronary Artery Disease. Circ Cardiovasc Qual Outcomes 2018;11:e004191.
- Koo BK, Erglis A, Doh JH, et al. Diagnosis of ischemia-causing coronary stenoses by noninvasive fractional flow reserve computed from coronary computed tomographic angiograms. Results from the prospective multicenter DISCOVER-FLOW (Diagnosis of Ischemia-Causing Stenoses Obtained Via Noninvasive Fractional Flow Reserve) study. J Am Coll Cardiol 2011;58:198-97.
- Min JK, Leipsic J, Pencina MJ, et al. Diagnostic accuracy of fractional flow reserve from anatomic CT angiography. JAMA 2012;308:1237-45.
- Nørgaard BL, Leipsic J, Gaur S, et al. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: the NXT trial (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps). J Am Coll Cardiol 2014;63:1145-55.
- Li S, Tang X, Peng L, Luo Y, Dong R, Liu J. The diagnostic performance of CT-derived fractional flow reserve for evaluation of myocardial ischaemia confirmed by invasive fractional flow reserve: a meta-analysis. Clin Radiol 2015;70:476-86.
- Curzen NP, Nolan J, Zaman AG, Nørgaard BL, Rajani R. Does the Routine Availability of CT-Derived FFR Influence Management of Patients With Stable Chest Pain Compared to CT Angiography Alone?: The FFRCT RIPCORD Study. JACC Cardiovasc Imaging 2016;9:1188-94.
- Douglas PS, Pontone G, Hlatky MA, et al. Clinical outcomes of fractional flow reserve by computed tomographic angiography-guided diagnostic strategies vs. usual care in patients with suspected coronary artery disease: the prospective longitudinal trial of FFR(CT): outcome and resource impacts study. Eur Heart J 2015;36:3359-67.
- Douglas PS, De Bruyne B, Pontone G, et al. 1-Year Outcomes of FFRCT-Guided Care in Patients With Suspected Coronary Disease: The PLATFORM Study. J Am Coll Cardiol 2016;68:435-45.
- Douglas PS, Hoffmann U, Patel MR, et al. Outcomes of anatomical versus functional testing for coronary artery disease. N Engl J Med 2015;372:1291-300.
- Nørgaard BL, Terkelsen CJ, Mathiassen ON, et al. Clinical Outcomes Using Coronary CT Angiography and FFRCT-Guided Management of Stable Chest Pain Patients. J Am Coll Cardiol 2018;Aug 25:25202.
- Hlatky MA, Saxena A, Koo BK, Erglis A, Zarins CK, Min JK. Projected costs and consequences of computed tomography-determined fractional flow reserve. Clin Cardiol 2013;36:743-8.
- Rajani R, Webb J, Marciniak A, Preston R. Comparative efficacy testing - fractional flow reserve by coronary computed tomography for the evaluation of patients with stable chest pain. Int J Cardiol 2015;183:173-7.
- HeartFlow FFRCT for estimating fractional flow reserve from coronary CT angiography (NICE website). February 2017. Available at https://www.nice.org.uk/guidance/mtg32. Accessed February 6, 2019.
- Asher A, Singhal A, Thornton G, Wragg A, Davies C. FFRCT derived from computed tomography angiography: the experience in the UK. Expert Rev Cardiovasc Ther 2018;16:919-29.
Keywords: Angina, Stable, Coronary Artery Disease, Coronary Angiography, Sequoia, Prospective Studies, Confidence Intervals, Constriction, Pathologic, Hospital Costs, Hydrodynamics, Myocardial Infarction, Coronary Stenosis, Angina Pectoris, Percutaneous Coronary Intervention, Myocardial Ischemia, Registries, Algorithms, Retrospective Studies, Fractional Flow Reserve, Myocardial
< Back to Listings