Antithrombotic Strategy in Patients With AF and Recent ACS or PCI: Primary Results of the AUGUSTUS Trial
Introduction
The optimal antithrombotic strategy for patients with atrial fibrillation (AF) with acute coronary syndrome (ACS) and/or recent percutaneous coronary intervention (PCI) can be challenging. Although dual antiplatelet therapy (DAPT) is indicated for secondary prevention of coronary events and to protect against stent thrombosis, it is not indicated for stroke prevention in patient with AF.1-3 Conversely, oral anticoagulation (OAC) with either warfarin or a direct oral anticoagulant (DOAC) is indicated for stroke prevention in patients with AF but provides limited protection against future coronary ischemic events or stent thrombosis (although there are emerging data demonstrating some benefit with DOACs).1,3,4 Furthermore, the combination of antiplatelet and anticoagulant therapies (i.e., triple therapy) has been associated with significantly increased risk of bleeding and with less clear benefit with respect to ischemic events.5-7
Prior Studies
The WOEST study (What is the Optimal Antiplatelet and Anticoagulant Therapy in Patients with Oral Anticoagulation and Coronary Stenting) randomized patients undergoing PCI on OAC to aspirin plus clopidogrel versus clopidogrel alone and found that clopidogrel alone resulted in lower rates of both bleeding and ischemic events.8 However, it was a small study that randomized 573 total patients with broad indication for OAC use.
PIONEER-AF PCI (An Open-Label, Randomized, Controlled, Multicenter Study Exploring Two Treatment Strategies of Rivaroxaban and a Dose-Adjusted Oral Vitamin K Antagonist Treatment Strategy in Subjects With Atrial Fibrillation Who Undergo Percutaneous Coronary Intervention) randomized 2,100 patients to 3 strategies that included 2 rivaroxaban-based strategies and 1 traditional vitamin K antagonist (VKA) based triple therapy strategy and found lower rates of bleeding in the two rivaroxaban-based strategies compared with the VKA-based strategy.9 Likewise, the REDUAL PCI trial (Randomized Evaluation of Dual Antithrombotic Therapy With Dabigatran vs. Triple Therapy With Warfarin in Patients With Nonvalvular Atrial Fibrillation Undergoing Percutaneous Coronary Intervention) randomized 2,725 patients to 2 different doses of dabigatran with P2Y12 inhibitor versus a warfarin-based triple therapy strategy and found lower rates of bleeding with the dabigatran-based strategies.10
Whereas both of these studies demonstrated the safety of DOAC-based strategies, they were not designed to assess whether the observed bleeding reduction was due to the DOAC or simply the discontinuation of aspirin. Additionally, PIONEER-AF PCI studied doses of rivaroxaban that were not demonstrated to reduce stroke in patients with AF.
AUGUSTUS Study Design
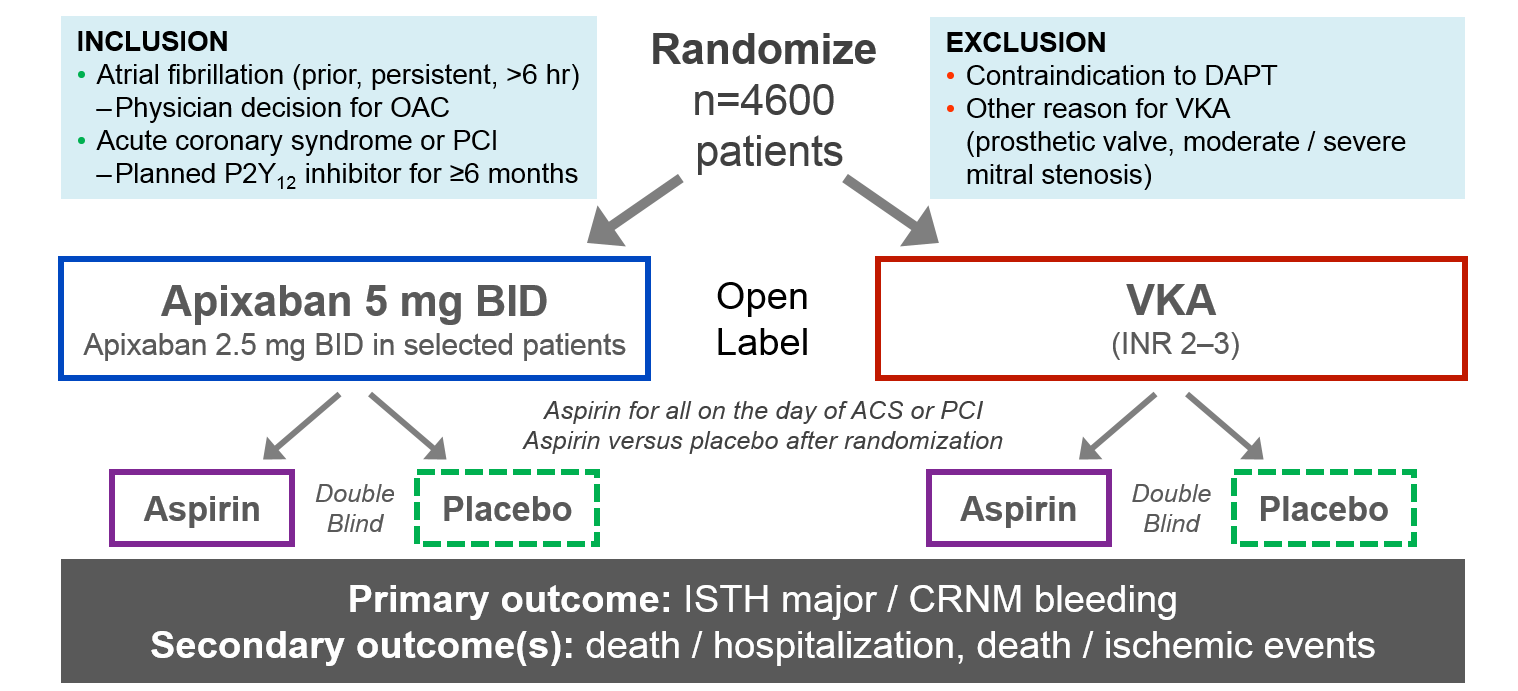
AUGUSTUS (Antithrombotic Therapy After Acute Coronary Syndrome or PCI in Atrial Fibrillation) is a 2 x 2 factorial randomized clinical trial that sought to determine the optimal antithrombotic strategy among patient with AF and recent ACS and/or PCI.11 Patients were assigned to either open-label warfarin or apixaban and double-blind aspirin or aspirin placebo on planned P2Y12 inhibitor. The trial was designed to test two independent hypotheses:
- Apixaban would be at least noninferior, and possibly superior, to warfarin with respect to International Society on Thrombosis and Haemostasis (ISTH) major/clinically relevant nonmajor (CRNM) bleeding.
- Single antiplatelet therapy with a P2Y12 inhibitor would be superior to DAPT (P2Y12 inhibitor plus aspirin) with respect to ISTH major/CRNM bleeding.
The primary outcome for each study factor was ISTH major/CRNM bleeding. The secondary outcome included death or hospitalization, death or ischemic events (stroke, myocardial infarction, stent thrombosis, urgent revascularization), and the individual components of the secondary outcomes. The study follow-up period was 6 months.
Figure 1: Study Flow
Primary Results of AUGUSTUS
The study randomized 4,614 patients from 494 sites across 33 countries.12 The median age of all patients was 70.6 years, and about one-third of patients were women. Patient characteristics were well-balanced across study arms. The mean CHADS-VASc score was 3.9, and the mean HAS-BLED score was 2.9, indicating a high risk of ischemic stroke as well as bleeding. Only half of all patients had been on prior OAC, and 92.6% of patients were on clopidogrel, with the remainder on other P2Y12 agents.
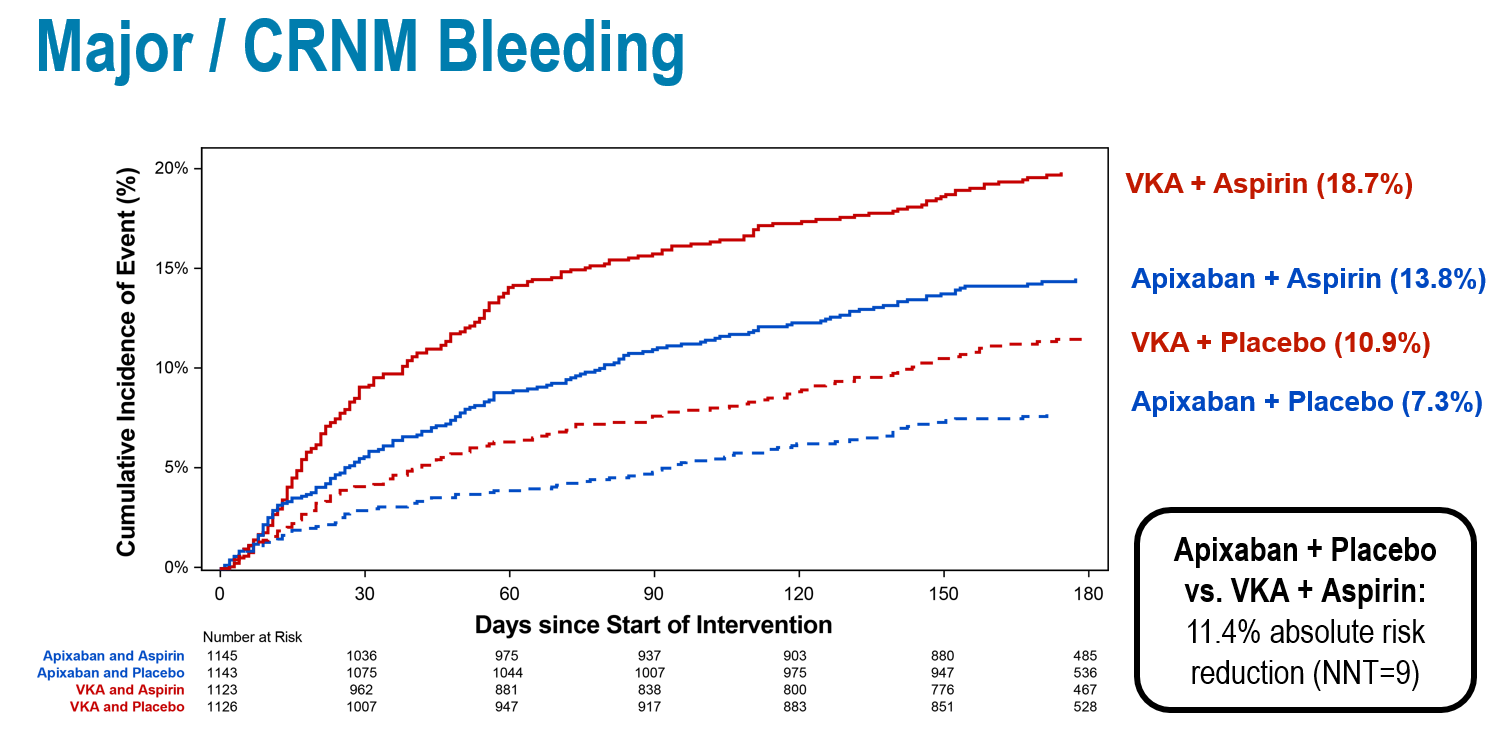
At 6 months, 10.5% of patients receiving apixaban and 14.7% receiving warfarin had an ISTH major/CRNM bleeding event (hazard ratio [HR] 0.69; 95% confidence interval [CI], 0.58-0.81), meeting the prespecified endpoints for both noninferiority and superiority. Among patients receiving aspirin, 16.1% had a bleeding event compared with 9.0% receiving aspirin placebo (HR 1.89; 95% CI, 1.59-2.24; p < 0.001). The number needed to treat (NNT) with apixaban compared with warfarin over 6 months to prevent 1 episode of bleeding was 24, whereas the number needed to harm with treatment using aspirin versus placebo was 14.
Apixaban was found to be superior to warfarin with respect to death/rehospitalization (23.5% vs. 27.4%) (HR 0.83; 95% CI, 0.74-0.96; p = 0.002; NNT = 26), driven primarily by differences in rates of rehospitalization. However, no such difference was observed in the antiplatelet-regimen comparison (26.2% with aspirin vs. 24.7% with aspirin placebo) (HR 1.08; 95% CI, 0.96-1.21).
With respect to death or ischemic events, there were no significant differences between apixaban/warfarin (6.7% vs 7.1%) (HR 0.93; 95% CI, 0.75-1.16) or aspirin/placebo (6.5% vs 7.3%) (HR 0.89; 95% CI, 0.71-1.11), though apixaban treatment resulted in fewer strokes (0.6% vs 1.1%) (HR 0.50; 95% CI, 0.26-0.97). Although the individual endpoints are exploratory and hypothesis generating, this provides additional reassurance about the importance of choosing the indicated dose of apixaban that has previously demonstrated stroke prevention.
Figure 2: Primary Outcome
Clinical Implications
AUGUSTUS is the first study to evaluate the independent effects of anticoagulant and antiplatelet therapy on patients with AF and recent ACS and/or PCI. The study found that apixaban resulted in lower bleeding compared with warfarin, and aspirin resulted in higher bleeding than placebo. Apixaban also resulted in lower rates of death/rehospitalization compared with warfarin, driven primarily by rehospitalization. For most patients, a regimen of aspirin on background clopidogrel offered balance between the ischemic and bleeding risks in this high-risk population.
Although not statistically significant, the study did demonstrate higher numerical counts of myocardial infarction, urgent revascularization, and stent thrombosis among patients assigned to placebo compared with patients assigned to aspirin. There are still questions to be answered about timing, predictors, and prognosis of stent thrombosis as well as the risk-benefit ratio between stent thrombosis and bleeding at different time points after the ACS/PCI event. This likely warrants further study.
However, AUGUSTUS clarifies the specific risks associated with the various treatment strategies and demonstrates that the risk of ischemic events is relatively low, even among patients assigned to aspirin. This suggests that a strategy of apixaban and clopidogrel without aspirin is safest for most patients, without significant differences in ischemic events compared with regimens that included a VKA, aspirin, or both.
Thus, one reasonable approach may be to use aspirin during the initial treatment of the ACS/PCI event and during the course of hospitalization. Aspirin can then be safely discontinued around the time of discharge and the OAC and P2Y12 inhibitor maintained for at least 6 months.
Summary
In patients with AF and recent ACS and/or PCI who are treated on background P2Y12 inhibitor, an antithrombotic strategy of apixaban without concomitant aspirin use resulted in less bleeding and fewer hospitalizations with no statistically significant increase in ischemic events compared with a regimen of VKA and/or aspirin.
References
- Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC Guideline for the Management of Patients with Non-ST-Elevation Acute Coronary Syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014;64:e139-e228.
- January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 2014;64:e1-76.
- O'Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013;61:e78-e140.
- Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA Guideline Focused Update on Duration of Dual Antiplatelet Therapy in Patients With Coronary Artery Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2016;68:1082-115.
- Hansen ML, Sørensen R, Clausen MT, et al. Risk of bleeding with single, dual, or triple therapy with warfarin, aspirin, and clopidogrel in patients with atrial fibrillation. Arch Intern Med 2010;170:1433-41.
- Lopes RD, Rao M, Simon DN, et al. Triple vs Dual Antithrombotic Therapy in Patients with Atrial Fibrillation and Coronary Artery Disease. Am J Med 2016;129:592-599.e1.
- Sørensen R, Hansen ML, Abildstrom SZ, et al. Risk of bleeding in patients with acute myocardial infarction treated with different combinations of aspirin, clopidogrel, and vitamin K antagonists in Denmark: a retrospective analysis of nationwide registry data. Lancet 2009;374:1967-74.
- Dewilde WJ, Oirbans T, Verheugt FW, et al. Use of clopidogrel with or without aspirin in patients taking oral anticoagulant therapy and undergoing percutaneous coronary intervention: an open-label, randomised, controlled trial. Lancet 2013;381:1107-15.
- Gibson CM, Mehran R, Bode C, et al. Prevention of Bleeding in Patients with Atrial Fibrillation Undergoing PCI. N Engl J Med 2016;375:2423-34.
- Cannon CP, Bhatt DL, Oldgren J, et al. Dual Antithrombotic Therapy with Dabigatran after PCI in Atrial Fibrillation. N Engl J Med 2017;377:1513-24.
- Lopes RD, Vora AN, Liaw D, et al. An open-Label, 2 × 2 factorial, randomized controlled trial to evaluate the safety of apixaban vs. vitamin K antagonist and aspirin vs. placebo in patients with atrial fibrillation and acute coronary syndrome and/or percutaneous coronary intervention: Rationale and design of the AUGUSTUS trial. Am Heart J 2018;200:17-23.
- Lopes RD, Heizer G, Aronson R, et al. Antithrombotic Therapy after Acute Coronary Syndrome or PCI in Atrial Fibrillation. N Engl J Med 2019;380:1509-24.
Clinical Topics: Acute Coronary Syndromes, Anticoagulation Management, Arrhythmias and Clinical EP, Invasive Cardiovascular Angiography and Intervention, Prevention, Anticoagulation Management and ACS, Anticoagulation Management and Atrial Fibrillation, Implantable Devices, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Interventions and ACS
Keywords: ACC Annual Scientific Session, ACC19, Arrhythmias, Cardiac, Warfarin, Anticoagulants, Atrial Fibrillation, Aspirin, Fibrinolytic Agents, Acute Coronary Syndrome, Secondary Prevention, Double-Blind Method, Vitamin K 1, Stroke, Brain Ischemia, Pyridones, Pyrazoles, Ticlopidine, Hemorrhage, Thrombosis, Myocardial Infarction, Percutaneous Coronary Intervention, Hemostasis, Stents
< Back to Listings