Length of Stay After PCI
Case 1
A 65-year-old male patient was referred for elective outpatient coronary angiography. He had been experiencing anginal symptoms for several months despite maximally tolerated doses of metoprolol, isosorbide mononitrate, and ranolazine. A pharmacological myocardial perfusion stress test revealed a moderate-sized, highly reversible inferior-lateral wall defect. Comorbidities included hypertension, hyperlipidemia, asthma, and osteoarthritis.
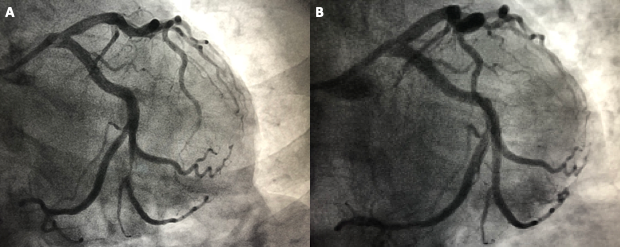
A 6 French, right radial diagnostic approach was selected. Coronary angiography demonstrated a left dominant system with a left posterior lateral lesion that correlated with the stress test findings (Figure 1). Using an XB 3.5 guide catheter over a work horse wire, the lesion was predilated with a 2.75 x 12 mm semi-compliant balloon, and then stented with a 3.0 x 18 mm zotarolimus-eluting stent at slightly above nominal pressure. Final angiography demonstrated Thrombolysis in Myocardial Infarction (TIMI) 3 flow, no dissections, no perforations, and 0% residual stenosis. A radial hemostasis band was used and ultimately removed after 2 hours. The patient had no symptoms during or after the procedure. He was observed in the procedural holding area for 6 hours then discharged home to the care of his spouse.
Figure 1
Case 2
An 81-year-old male patient was referred for planned chronic total occlusion (CTO) intervention to an ostial occlusion of the right coronary artery (RCA). The patient had been suffering from intense anginal symptoms that were not responsive to maximally tolerated doses of amlodipine and carvedilol. Transthoracic echocardiography (TTE) demonstrated a hypokinetic inferior wall with a mildly depressed left ventricular ejection fraction. Initially when he presented with classic symptoms and risk factors that included hypertension, hyperlipidemia, stage III chronic kidney disease, and history of tobacco use, the patient was referred directly for coronary angiography. Coronary angiography, as mentioned, demonstrated an ostial occlusion of the RCA. Given the hypokinesis on TTE, a pharmacologic nuclear stress test was ordered before proceeding with percutaneous coronary intervention (PCI) that demonstrated a large, fully reversible inferior wall defect with normal uptake on rest imaging.
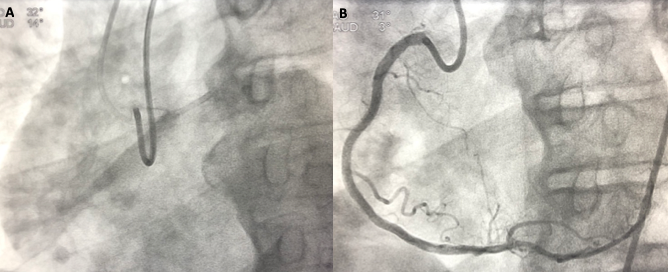
Using a bilateral 7 French femoral approach, an XB 3.5 guide was engaged in the left main, and an AL 1 guide was engaged in the RCA. Antegrade injections demonstrated no antegrade flow (Figure 2) but robust collaterals from the left system. Ultimately, an antegrade wire escalation technique was successfully completed and followed by deployment of overlapping 3.5 x 38 mm and 4.0 x 24 mm everolimus-eluting stents after vessel prep with atherectomy. Total contrast used was <100cc. Final angiography demonstrated TIMI 3 flow, no dissections, no perforations, and 0% residual stenosis. Suture-based closure devices were used for the femoral puncture sites, with no bleeding after deployment. The patient was transferred to the procedural holding area for observation and post-procedure hydration. He experienced no post-procedure complications but was monitored overnight and discharged the next day.
Figure 2
Length of Stay Following PCI
PCI has progressed rapidly over the past decade. From routine 8 French femoral access procedures, catheterization laboratories now often use 5 and 6 French radial access for most procedures. Stent platforms/polymers have improved significantly and are now considered thrombo-protective. Additional procedural improvements have reduced complications. These reductions in complications have facilitated the ability to discharge patients earlier, even on the same day of PCI.
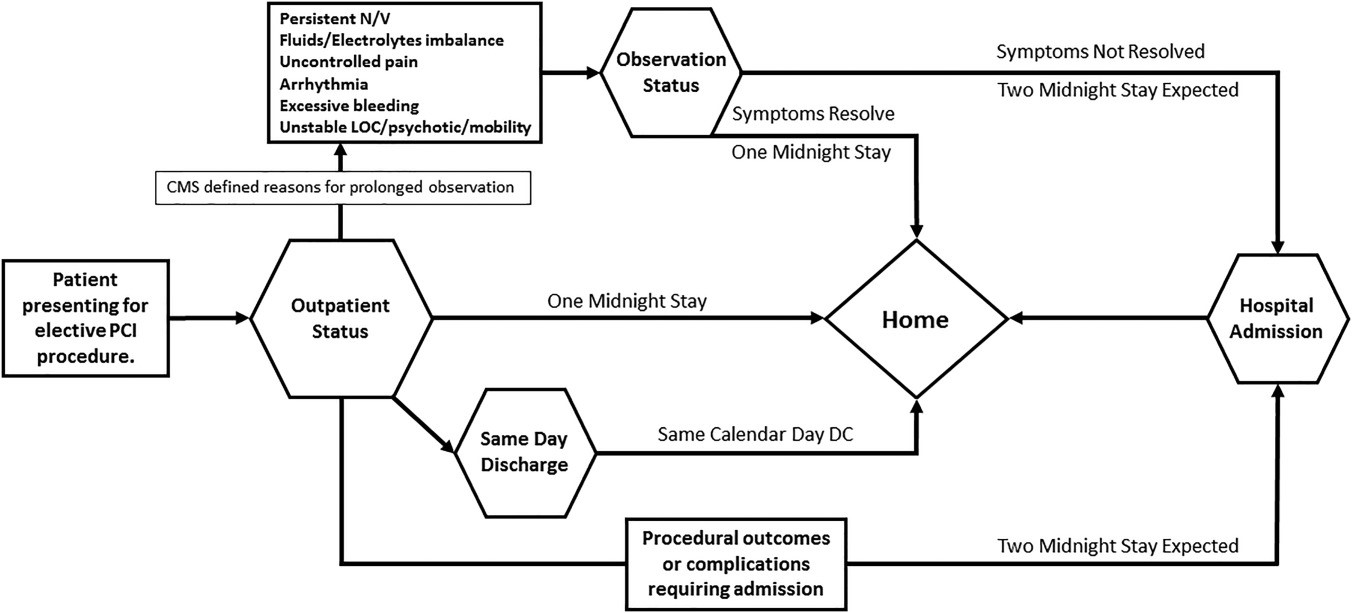
The two cases presented demonstrate opposite ends of the PCI spectrum. In Case 1, a short stent was placed in a type A lesion using a 6 French radial guide. Case 2 used bilateral femoral access with a 7 French sheath, rotational atherectomy, CTO intervention with multiple overlapping stents. Length of stay was accordingly different. Operators in Case 1 monitored the patient post-PCI for 6 hours and then discharged home on the same day. Operators in Case 2 monitored the patient overnight, despite ideal hemostasis, no complications and no symptoms. The question must be asked: Did Case 2 (CTO intervention) need to be kept overnight? Specifically, are there avoidable events 6-24 hours after a procedure that care be identified by in-hospital monitoring (Figure 3)?1
Figure 3
Complications and Their Timing
The justification for prolonged monitoring post-PCI is to avoid complications not apparent during short-term monitoring that may be identified during an intermediate period, enabling rapid management to reduce adverse events. However, the reality is that complications are decreasing, and longer monitoring may not be necessary.
Post-PCI complications carry a significant degree of harm. Thus, physicians tend toward a conservative approach, often continuing post-PCI hospitalization longer than potentially necessary. The CHAMPION PHOENIX (Cangrelor vs. Standard Therapy to Achieve Optimal Management of Platelet Inhibition) trial was an all-comers, acute coronary syndrome (ACS) and elective PCI patient trial comparing cangrelor plus clopidogrel versus clopidogrel alone.2 Events were intensely monitored given that the impact of cangrelor is during the procedure and in the immediate peri-procedural period. A significant and under-reported finding outside of the primary study is that nearly all events (combined endpoint of death, myocardial infarction, and stent thrombosis or ischemia-driven revascularization) occurred within 6 hours of the procedure regardless of treatment strategy. Events were essentially flat over 42 hours post-PCI, with equivalent event rates during hours 6-24 and 24-48.
The STRIDE (Same-Day Transradial Intervention and Discharge Evaluation) and DISCHARGE studies demonstrated nearly identical findings.3-4 In STRIDE and DISCHARGE, all events were before 6 hours or after 24 hours. As mentioned previously, event rates for modern drug-eluting stents are very low. In the recently published 1,243 patient BIONYX (Bioresorbable Polymer ORSIRO Versus Durable Polymer RESOLUTE ONYX Stents) PCI trial with the commercially available Resolute Onyx drug-eluting stent (Medtronic; Minneapolis, MN), the total number of stent thromboses was 1.5 Thus, understanding current timing and incidence of post-PCI complications allows more informed decisions about resource utilization and timing of discharge.
Influence of Medical Therapy
In addition to procedural technique and equipment, better understanding of optimal medical therapy has improved due to availability of P2Y12 inhibitors. Bleeding rates have declined due to the increased use of heparin or bivalirudin monotherapy with decreased utilization of glycoprotein IIb/IIIa inhibitors (GPI).6-7 GPI therapy is associated with increased rates of thrombocytopenia and/or bleeding, thus are not being used or supplanted with cangrelor.8 The introduction of prasugrel and ticagrelor has provided oral P2Y12 inhibition with a rapid onset and high potency and a generally limited increased bleeding risk. In the PLATO (Platelet Inhibition and Patient Outcomes) trial, TIMI-defined non-coronary artery bypass grafting bleeding rate with ticagrelor increased only 0.6% with a nearly 1% reduction in stent thrombosis and a 1.4% reduction in all-cause death.9 Appropriate pharmacotherapy is important for reducing ischemic complications such as stent thrombosis while achieving lower bleeding rates.
ACS PCI
Patients with ACS fall into two categories: unstable angina (UA)/non-ST-segment elevation myocardial infarction (NSTEMI) and ST-segment elevation myocardial infarction (STEMI). Data from the STEMI population in the CathPCI registry demonstrated that length of stay ≤3 days was associated with similar or better outcomes than with longer stays.10 Longer hospital stays often reflect shock or other high-risk clinical conditions, and short stays (i.e., 2-3 days) are safe for usual STEMI given that mechanical and non-mechanical complications most often occur within the first 48 hours.11
Patients with UA/NSTEMI have been included in all of the previously discussed data, thus direct comparisons are appropriate. Clinical risk stratification is important given the nature of ACS versus elective PCI. That these patients are typically admitted to the hospital influences the decision of discharge timing as well. Elective PCI patients usually do not require a TTE or trending of troponins for prognosis. UA/NSTEMI can precipitate heart failure, prolonging hospitalization, which is uncommon in elective PCI patients. Therefore, selected, elective PCI patients can undergo same-day discharge, patients with STEMI require longer length of stay, and patients with UA/NSTEMI are more nuanced and require an extensive clinical assessment.
Non-Clinical Factors
Elective PCI is billed as an outpatient procedure regardless of overnight observation or same-day discharge, so from a resource perspective, same-day discharge can be more cost efficient. Patients with ACS are considered inpatients regardless of the number of nights if physician documentation supports inpatient status. Thus, discharge decisions are less influenced by length-of-stay requirements because length of stay does not typically increase reimbursement for ACS patients; longer hospital stays increase costs, reducing reimbursement.
Medicolegal concerns always are a specter in any decision-making process. However, with appropriate documentation supporting a same-day discharge versus overnight stays, legal concerns can be reduced. Additionally, with increasing favorable clinical experience surrounding same-day discharge, litigation concerns should diminish.
Conclusions
Ultimately, the decision regarding discharge is based on each individual patients' clinical scenario. A recently published consensus document on length of stay outlines much of the data presented above and presents a template and flow chart for determining the optimal discharge decision (Figure 3, Table 1).1 Stable elective PCI cases can be typically monitored for 6 hours then sent home with no significant risk of complications beyond those that could occur over 24 hours and beyond. Modern drug-eluting stent platforms, improved anticoagulation, and potent P2Y12 inhibitors provide a framework for safe same-day discharge. Radial access with reduced bleeding complications should also factor into decision-making.
When applying these criteria to our two case presentations, we have uncomplicated single-vessel PCI in stable patients with no post-procedure symptoms. Despite the massively differing complexity, nothing was gained by in-house overnight hospitalization for the CTO patient. Practically speaking, the patient who remained in the hospital did not sleep well and ate poorly, and the hospital utilized a bed for no clinical benefit. Despite the perception that one case should be more closely monitored than another, applying the data and clinical decision-making tools suggests otherwise.
Patients with ACS are all different and require a more comprehensive workup. Patients with STEMI require a longer length of stay, and this applies to patients with UA/NSTEMI to some degree as well. However, patients with UA/NSTEMI are included in the clinical data presented above, which supports expedited discharge after the completion of the clinical work-up. Reimbursement concerns should not influence a longer length of stay if needed given Centers for Medicare & Medicaid Services reimbursement patterns. Expediated discharge should also be a program goal and involve the entire team to ensure follow-up calls and visits and appropriate discharge instructions and prescriptions.
The totality of the current evidence suggests that a stable patient undergoing an uncomplicated PCI can be sent home after 6 hours of monitoring. Patients with UA/NSTEMI can also be evaluated for expedited discharge. Patients with STEMI continue to require a longer length of stay. However, after an uncomplicated 3 days post-PCI, there is no benefit in remaining in-house.
Table 1: Determining Discharge Status
|
Expedited Discharge Requirements |
Factors Against Expedited Discharge |
Patient Factors |
|
|
Procedure Factors |
|
|
Program |
|
|
References
- Seto AH, Shroff A, Abu-Fadel M, et al. Length of stay following percutaneous coronary intervention: An expert consensus document update from the society for cardiovascular angiography and interventions. Catheter Cardiovasc Interv 2018;92:717-31.
- Bhatt DL, Stone GW, Mahaffey KW, et al. Effect of platelet inhibition with cangrelor during PCI on ischemic events. N Engl J Med 2013;368:1303-13.
- Jabara R, Gadesam R, Pendyala L, et al. Ambulatory discharge after transradial coronary intervention: Preliminary US single-center experience (Same-day TransRadial Intervention and Discharge Evaluation, the STRIDE Study). Am Heart J 2008;156:1141-6.
- Small A, Klinke P, Della Siega A, et al. Day procedure intervention is safe and complication free in higher risk patients undergoing transradial angioplasty and stenting. The discharge study. Catheter Cardiovasc Interv 2007;70:907-12.
- von Birgelen C, Zocca P, Buiten RA, et al. Thin composite wire strut, durable polymer-coated (Resolute Onyx) versus ultrathin cobalt-chromium strut, bioresorbable polymer-coated (Orsiro) drug-eluting stents in allcomers with coronary artery disease (BIONYX): an international, single-blind, randomised non-inferiority trial. Lancet 2018;392:1235-45.
- Shahzad A, Kemp I, Mars C, et al. Unfractionated heparin versus bivalirudin in primary percutaneous coronary intervention (HEAT-PPCI): an open-label, single centre, randomised controlled trial. Lancet 2014;384:1849-58.
- Stone GW, Witzenbichler B, Guagliumi G, et al. Bivalirudin during primary PCI in acute myocardial infarction. N Engl J Med 2008;358:2218-30.
- Groves EM, Bhatt DL, Steg PG, et al. Incidence, Predictors, and Outcomes of Acquired Thrombocytopenia After Percutaneous Coronary Intervention: A Pooled, Patient-Level Analysis of the CHAMPION Trials (Cangrelor Versus Standard Therapy to Achieve Optimal Management of Platelet Inhibition). Circ Cardiovasc Interv 2018;11:e005635.
- Wallentin L, Becker RC, Budaj A, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 2009;361:1045-57.
- Swaminathan RV, Rao SV, McCoy LA, et al. Hospital length of stay and clinical outcomes in older STEMI patients after primary PCI: a report from the National Cardiovascular Data Registry. J Am Coll Cardiol 2015;65:1161-71.
- Melberg T, Jørgensen M, Ørn S, Solli T, Edland U, Dickstein K. Safety and health status following early discharge in patients with acute myocardial infarction treated with primary PCI: a randomized trial. Eur J Prev Cardiol 2015;22:1427-34.
Clinical Topics: Acute Coronary Syndromes, Anticoagulation Management, Cardiac Surgery, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Anticoagulation Management and ACS, Aortic Surgery, Cardiac Surgery and Heart Failure, Acute Heart Failure, Interventions and ACS, Interventions and Imaging, Angiography, Nuclear Imaging
Keywords: Percutaneous Coronary Intervention, Length of Stay, Myocardial Infarction, Acute Coronary Syndrome, Troponin, Atherectomy, Coronary, Heparin, Drug-Eluting Stents, Follow-Up Studies, Absorbable Implants, Blood Platelets, Medicaid, Outpatients, Hirudins, Ticlopidine, Peptide Fragments, Angina, Unstable, Adenosine, Registries, Thrombocytopenia, Hemostasis, Thrombosis, Prognosis, Medicare, Heart Failure, Arteries, Coronary Angiography
< Back to Listings