Pericardial Angiosarcoma: Status Quo
Angiosarcoma originating from the heart, although exceptionally rare, is the most common cardiac primary malignant tumor.1 It typically presents in the right side of the heart and secondarily involves the pericardium. Primary pericardial angiosarcoma has a tendency to occur at middle age and appears more frequently in males.2 It has diverse clinical presentations and histological appearances, making early diagnosis challenging. Metastatic disease is very frequent by the time of diagnosis, mainly observed in lymph nodes, lungs, liver, central nervous system and bone.3-4 Earlier detection and targeted therapies may help improve the grave prognosis for this neoplasm.
Etiology
To date, no specific etiology and risk factors for the development of pericardial angiosarcoma are known. However, exposure to vinyl chloride, namely plastics, is believed to be associated with angiosarcoma.5 It has also been reported that mediastinal radiation makes a contribution to the development of this entity.6
Clinical Presentations
Aggressive pericardial angiosarcomas have an initial silent evolution. When present, symptoms and signs are generally associated with recurrent hemopericardium, pericarditis, invasion of adjacent structures and metastatic disease.7 Hence, the clinical picture is characterized by progressive dyspnea, pericarditic pain, chest pain, cough, general malaise and signs of caval obstruction. Such wide range of clinical manifestations may mimic many other diseases such that the diagnosis commonly comes unexpectedly during surgery or autopsy, eluding early detection of this tumor.8-9 Pericardial involvement can result in encasement and compression of vital structures, such as great vessels. In addition, malignancies are responsible for embolic events, myocardial infarction and arrhythmias.10 Rapidly, the clinical situation of patients may run a downhill course with intractable heart failure and death due to multiple organs failure.
Laboratory and Imaging Analysis
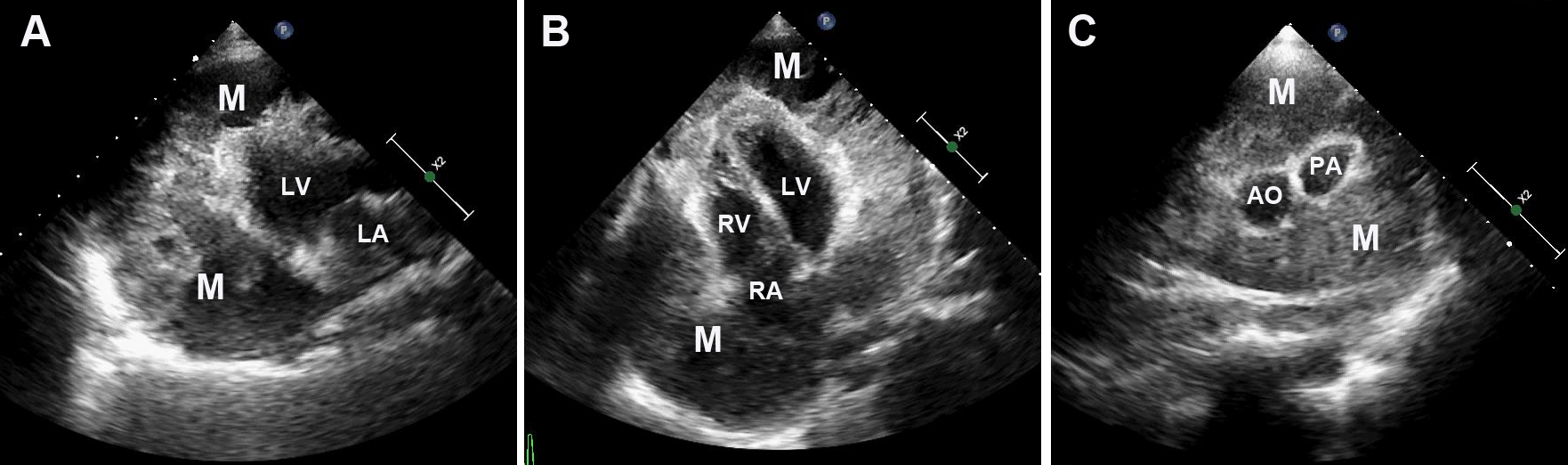
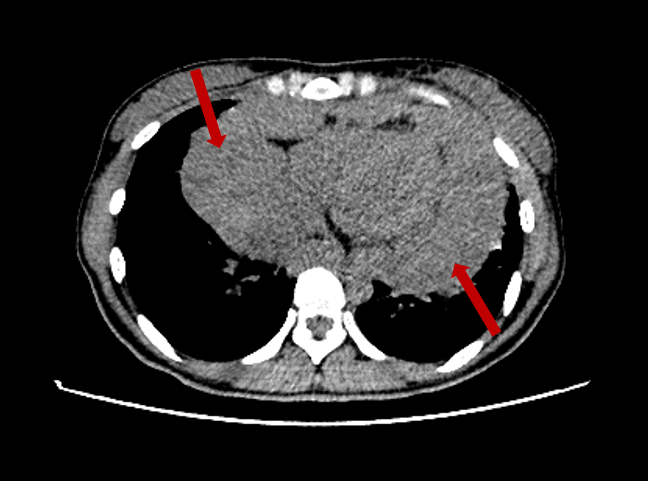
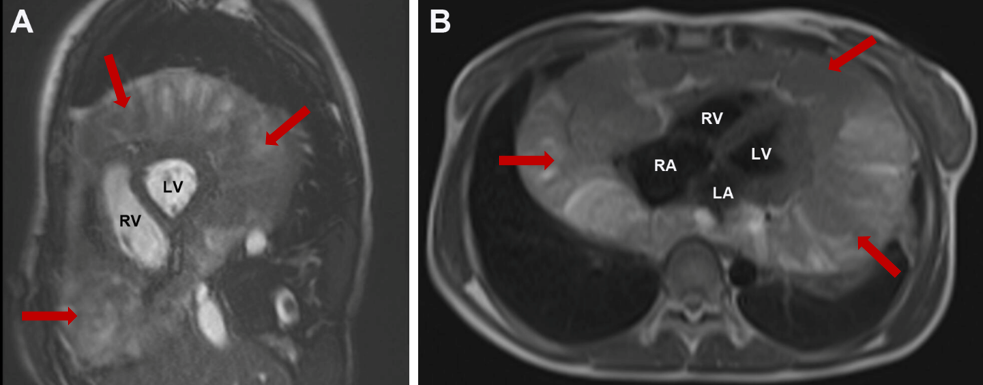
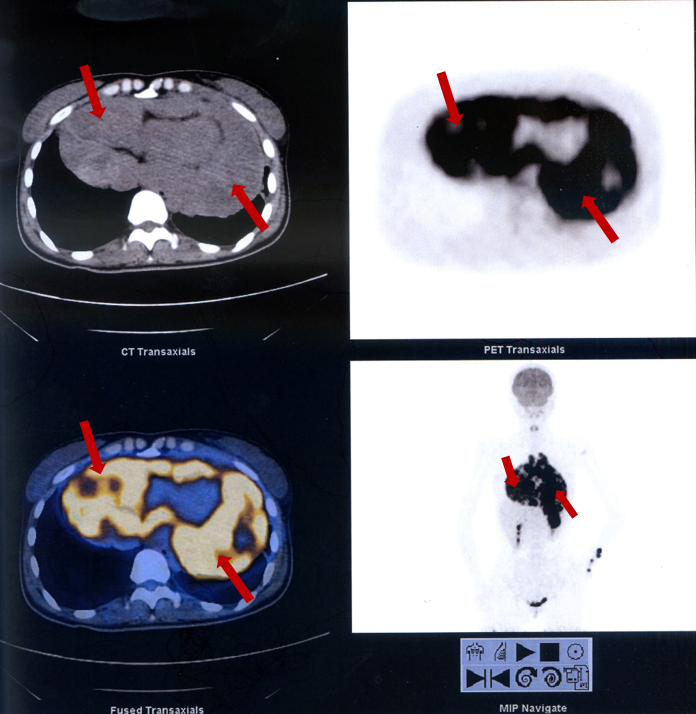
Although there are comprehensive clinical tests for diagnosing pericardial angiosarcomas, the value of these approaches is limited. Tumor markers, such as CA125, are usually elevated beyond normal limits. Pericardiocentesis yields heavily bloodstained fluid containing red and white blood cells. Repeated cytologic examinations of the pericardial effusion often fail to disclose malignant cells and there is no evidence of acid-fast bacilli, bacteria and viruses on smear or cultures. An electrocardiogram shows nonspecific ST-T wave changes and low voltage of the QRS complex. Chest radiography commonly delineates an enlarged cardiac silhouette (Figure 1). In most patients, transthoracic echocardiography discloses massive pericardial effusion, but it fails to depict an echogenic mass without a good acoustic window. In a few patients, transthoracic echocardiography shows the huge mass within the pericardium (Figure 2). While transesophageal echocardiography affords improved spatial resolution, it cannot detect distant structures from the heart or provide tissue characterization. Computed tomography plays a vital role in evaluating the location, size and extent of the tumor (Figure 3). Cardiac magnetic resonance (CMR) imaging confirms marked localized or diffuse thickening of the pericardium with hematic and solid components (Figure 4). Sometimes, it shows a"sunray"appearance on contrast-enhanced images.Tumor necrosis and hemorrhage can also be seen, as well as multiple foci of calcification, creating a"cauliflower"appearance.11 In some occasions, CMR has excellent diagnostic advantages to assess the exact location, characterizaton and staging of pericardial tumors, which is beneficial for management and posttreatment follow-up of patients. Nevertheless, a correlative study of CMR features and pathological appearances of pericardial angiosarcomas has not been performed to date. Positron emission tomography may be helpful in detecting metastasis from pericardial tumors12 (Figure 5).
Figure 1
Figure 2
Figure 3
Figure 4
Figure 5
Biopsy and Pathology
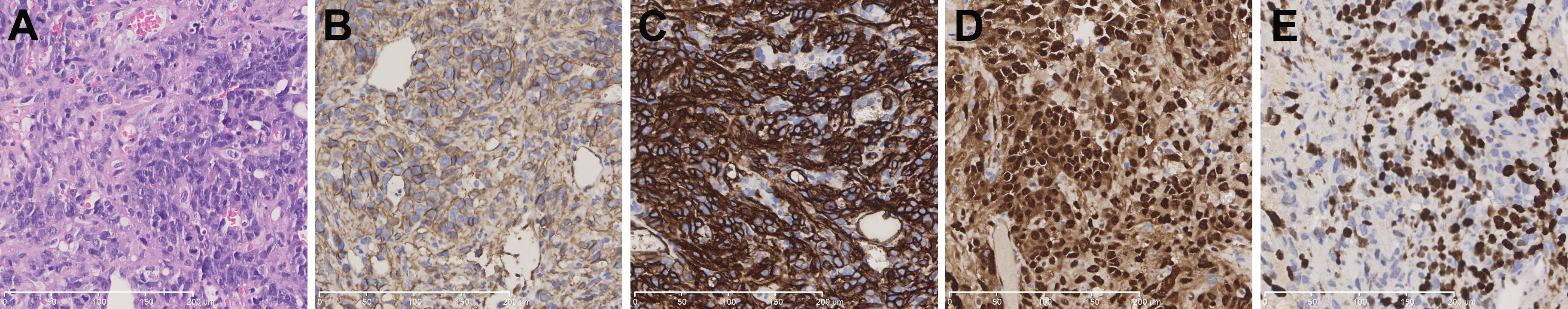
The definitive diagnosis of pericardial angiosarcoma is based on histopathological features. Therefore, mediastinoscopy, exploratory pericardiotomy or thoracotomy is performed with pericardial and lymph node biopsy. At operation, the heart is noted to be encased by hemorrhagic to solid tumor tissues, the texture of which resembles jelly or grapes. The parietal and visceral pericardium are not distinguishable implying that the pericardial sac is completely obliterated by the tumor. Occasionally, multiple gray to dusky red nodules can be seen in the lungs and pulmonary perihilar lymph nodes.13 If a pericardiectomy is undertaken for diagnosis, an extensive pericardial excision is recommended, since it will avoid sampling errors and may prevent subsequent development of constriction. Histologically, biopsies taken from the pericardium are characterized by the presence of anastomosing vascular channels lined by atypical, malignant endothelial cells showing frequent mitoses, which is consistent with angiosarcomas. Immunohistochemical staining pattern reveals that the tumor tissues express endothelial markers, such as CD31, CD34 , vimentin and factor VIII, supporting the diagnosis of angiosarcomas14-15 (Figure 6).
Figure 6
Diagnosis
The diagnosis of such angiosarcomas is often delayed, being made incidentally at operation or biopsy. Patients with pericardial angiosarcomas mostly manifest with pericardial effusions, which may be easily interpreted as various other cardiac abnormalities. For example, mesothelioma is the most common primary pericardial malignancy, the clinical features of which mimic pericardial angiosarcoma. However, from an immunohistochemical viewpoint, mesothelioma is positive for epithelial rather than endothelial markers.16 Other cardiac entities, including sarcomas, lymphoma, diffuse pericarditis and thrombus should be considered as well. Of note, culture of the pericardial fluid should precede biopsy. Eventually, for histological confirmation, percutaneous aspiration, biopsy or even surgical exploration is expected to be conducted. Malignant cells might infiltrate the incision canal or even the pleural cavity because of multiple pericardiocenteses, and this may result in delay of surgery.
Management
Due to the paucity of clinical data, there is no evidence-based management for such a rare angiosarcoma. Bloody pericardial effusion is initially suggestive of tuberculous pericarditis, but empirical antituberculosis or antibiotics therapy is futile. Subsequently, pericardiocentesis is always conducted, not only for diagnosis but also for relieving constriction. Generally, this tumor responds poorly to chemotherapy and radiation. Results of surgery alone have been disappointing because most patients present advanced disease at the time of diagnosis. Orthotopic cardiac transplantation has been carried out in some cases. Although survival has been prolonged, a high incidence of metastatic disease limits the utility.17 However, cardiac transplantation may be helpful for very carefully selected patients, of whom neoplasms are unresectable but locally aggressive involving only the heart without any metastases.
Presenting symptoms of this tumor frequently appear late, resulting in unresectable tumors in most cases. Consequently, available treatment options for this maligancy are only palliative. The length of survival for this group of neoplasms is dismal, ranging between 6-11 months after the onset of symptoms.11 Nowadays, with the introduction of multiple imaging techniques, pericardial angiosarcomas have become evident, even as preclinical findings. However, even though various advanced diagnostic imaging madalities have been applied, it still might miss the chance to detect this malignant tumor. Early diagnosis and complete excision are of great importance for a prolongation of survival. When the etiology of recurrent bloody pericardial effusion remains unknown, underlying malignancy should be suspected and early invasive diagnostic interventions, such as surgical exploration, should be considered for targeted therapy. In the future, clinical work will result in a improved prognosis and survival rate of these rare but lethal diseases.
References
- Burazor I, Aviel-Ronen S, Imazio M, et al. Primary malignancies of the heart and pericardium. Clin Cardiol 2014;37:582-8.
- Timóteo AT, Branco LM, Bravio I, et al. Primary angiosarcoma of the pericardium: case report and review of the literature. Kardiol Pol 2010;68:802-5.
- Burke A, Tavora F. The 2015 WHO Classification of Tumors of the Heart and Pericardium. J Thorac Oncol 2016;11:441-52.
- Rao JN, Gowda GD, Anand R. Angiosarcoma of the right atrium and right ventricle. J Card Surg 2017;32:807-8.
- Ma GT, Liu JZ, Miao Q, Cui QC. Angiosarcoma of the pericardium: a case report. Int J Clin Exp Pathol 2015;8:13568-70.
- Killion MJ, Brodovsky HS, Schwarting R. Pericardial angiosarcoma after mediastinal irradiation for seminoma. A case report and a review of the literature. Cancer 1996;78:912-7
- Li Y, Wang B, Zhang L, et al. Rare Case of Pericardial Angiosarcoma. Circ Heart Fail 2018;11:e005342.
- Zhrebker L, Cherni I, Gross LM, et al. Case report: whole exome sequencing of primary cardiac angiosarcoma highlights potential for targeted therapies. BMC Cancer 2017;17:17.
- Randhawa JS, Budd GT, Randhawa M, et al. Primary Cardiac Sarcoma: 25-Year Cleveland Clinic Experience. Am J Clin Oncol 2016;39:593-99.
- Maleszewski JJ, Anavekar NS. Neoplastic Pericardial Disease. Cardiol Clin 2017;35:589-600.
- Ong P, Greulich S, Schumm J, et al. Favorable course of pericardial angiosarcoma under paclitaxel followed by pazopanib treatment documented by cardiovascular magnetic resonance imaging. Circulation 2012;126:e279-81.
- Shi X, Li F. Primary Pericardial Angiosarcoma Shown on FDG PET/CT. Clin Nucl Med 2017;42:973-75.
- Dong Y, Zhu D, Dong L, Ren L. Primary cardiac angiosarcoma with pulmonary and lumbar metastases presenting as unexplained pericardial effusion in a 41 year-old man. Heart Lung Circ 2014;23:e145-6.
- Leduc C, Jenkins SM, Sukov WR, Rustin JG, Maleszewski JJ. Cardiac angiosarcoma: histopathologic, immunohistochemical, and cytogenetic analysis of 10 cases. Hum Pathol 2017;60:199-207.
- Wang JG, Wang B, Hu Y, et al. Clinicopathologic features and outcomes of primary cardiac tumors: a 16-year-experience with 212 patients at a Chinese medical center. Cardiovasc Pathol 2018;33:45-54.
- Yamamoto T, Ohtani K, Tanoue Y, Shiose A, Tsutsui H. Primary pericardial mesothelioma presenting as constrictive pericarditis. Eur Heart J Cardiovasc Imaging 2019;20:602.
- Cottini M, Pergolini A, Gentile P, Musumeci F. Primary Cardiac Angiosarcoma. J Card Surg 2016;31:63-4
Clinical Topics: Anticoagulation Management, Arrhythmias and Clinical EP, Cardiac Surgery, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Pericardial Disease, Implantable Devices, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Cardiac Surgery and Arrhythmias, Cardiac Surgery and Heart Failure, Acute Heart Failure, Heart Transplant, Interventions and Imaging, Computed Tomography, Echocardiography/Ultrasound, Nuclear Imaging
Keywords: Pericardial Effusion, Pericardiocentesis, Pericardiectomy, Hemangiosarcoma, Pericarditis, Tuberculous, Vimentin, Vinyl Chloride, Survival Rate, Echocardiography, Transesophageal, Mediastinoscopy, Pleural Cavity, Thoracotomy, Risk Factors, Selection Bias, Follow-Up Studies, Pericardium, Heart Neoplasms, Mesothelioma, Electrocardiography, Positron-Emission Tomography, Chest Pain, Biopsy, Arrhythmias, Cardiac, Factor VIII, Myocardial Infarction, Thrombosis, Heart Transplantation, Heart Failure, Leukocytes, Magnetic Resonance Spectroscopy, Early Diagnosis, Lymph Nodes, Dyspnea, Mitosis, Radiography, Endothelial Cells, Nervous System, Anti-Bacterial Agents, Tomography, Lymphoma
< Back to Listings