Preventive Cardiology – Children Are Not Little Adults
It Begins in Childhood
High cholesterol contributes to cardiovascular disease (CVD) across the lifespan. Retained lipoproteins (LPs), including apolipoprotein B (apoB), in the extracellular matrix of the coronary arterial wall elicit a maladaptive inflammatory response, resulting in atherosclerosis.1 Early atherosclerosis occurs by the second decade, as demonstrated by autopsy studies of young soldiers killed during the Korean and Vietnam wars.2,3 The Pathobiological Determinants of Atherosclerosis in Youth (PDAY) and a postmortem sub-Bogalusa cohort have not only identified prevalent fatty streaks and advanced atheromatous plaques in the aorta and coronary arteries of adolescents and young adults, but have linked their progression to premortum cardiovascular risk factors.4-7 Excess total cholesterol, particularly non HDL-cholesterol, elevated body mass index (BMI), and blood pressure levels show the strongest predictive associations with the early presence and progression of atherosclerosis. Early subclinical atherosclerotic lesions have also been demonstrated in vivo in children and adolescents with noninvasive ultrasound imaging of carotid artery intimal-medial thickness (CIMT).8,9 CIMT progresses with age. 'Vascular age' is accelerated with CVD risk factors that increase circulating apoB LPs, such as early onset diabetes mellitus, particularly type 2, and pediatric inflammatory conditions.10-12
Can We Reduce Risk?
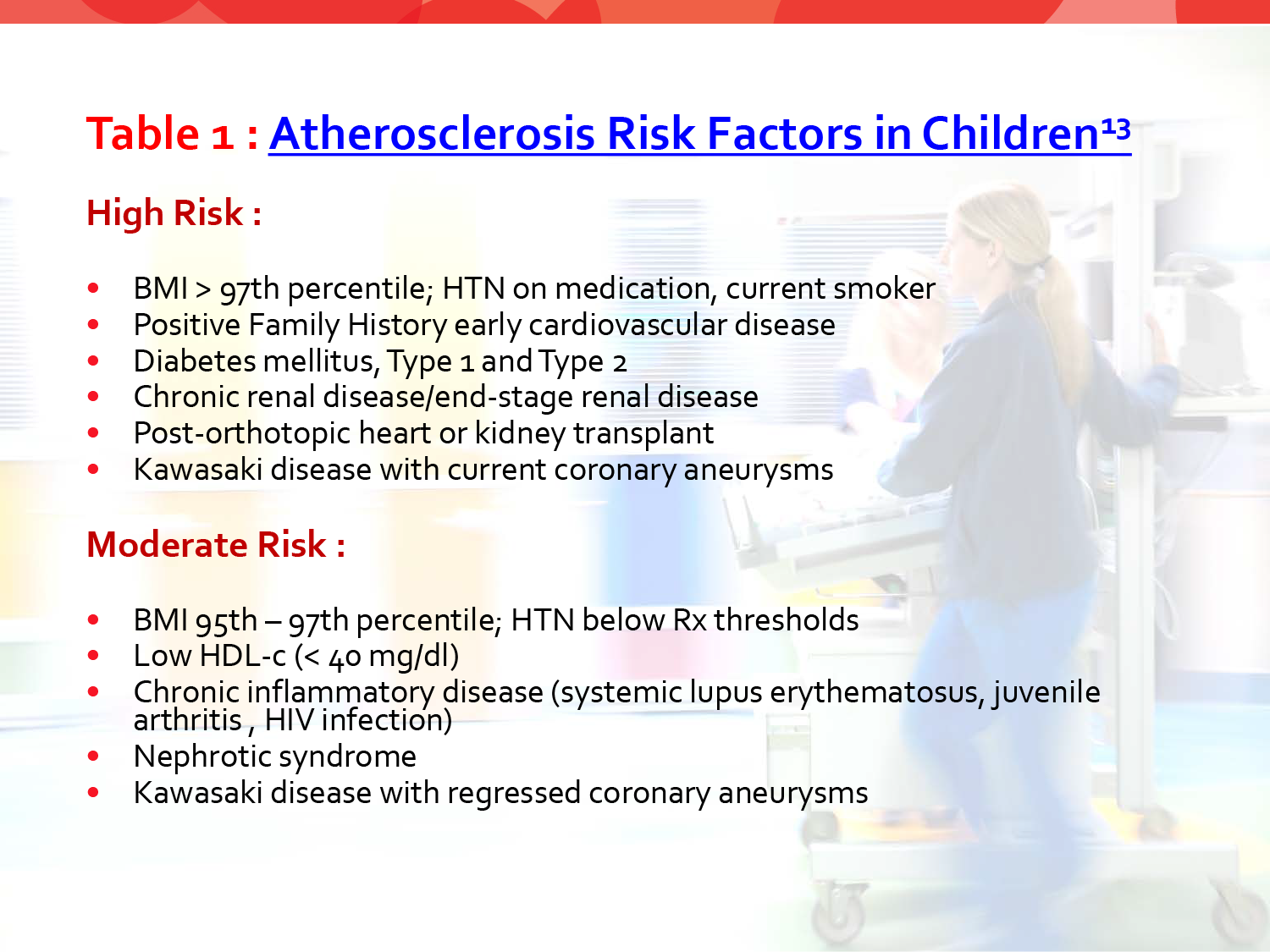
Early identification and risk reduction therapy during childhood and adolescence are important. The earliest stages of atherosclerosis (fatty streaks and raised atheroma) may be reversed by lowering apoB LPs. In the continued presence of inflammatory cardiovascular risk factors, smooth muscle cells migrate into the intima and form a fibrous cap, typically beginning in the third decade of life. Advanced plaques and eventual erosion of the cap lead to acute thrombotic vascular events. The complexity of advanced lesions, including accelerated LP retention in established lesions, renders them more irreversible with age. An extended interval between risk factor identification and disease expression is a unique opportunity for primary prevention. Universal screening is recommended between 9-11 and again between 17-18 years.13 Selective screening between 2-9 and between 11-17 years of age is recommended in the presence of: (1) a (+) Family history of early CVD (men younger than 55 years, women younger than 65 years), (2) a parent with known dyslipidemia, and (3) an established risk factor or a special risk condition in the child. Pediatric risk factors are classified as high or moderate and constitute conditions that contribute to an increased burden of apoB Lp (Table 1). Other potential risk factors include a history of cancer or congenital heart disease (especially coarctation of aorta and d-transposition of the great arteries), passive smoke exposure and an unknown family history.13
Adult versus Pediatrics Lipid Guidelines
Both adult and pediatric guidelines have faced controversy regarding overdiagnosis and overtreatment in the absence of known CVD. Adult and pediatric guidelines were applied to National Health and Nutrition Examination Survey (NHANES) participants aged 17-21 years from Jan 1999–Dec 2012. The mean total cholesterol and low-density lipoprotein (LDL) levels were lower but the triglyceride (TG) levels were higher in participants who were treated based on pediatric guidelines as compared to those who received therapy following the adult guidelines.14 Using pediatric guidelines resulted in statin treatment recommendations in more young people with lower LDL but higher prevalence for CVD risk. This is important to note as many patients between 17-21 years of age transition from a pediatric to an adult practice. Conflicting guidelines will lead to confusion in clinical practice as the underlying risk does not change.
The Current ACC/AHA Guidelines
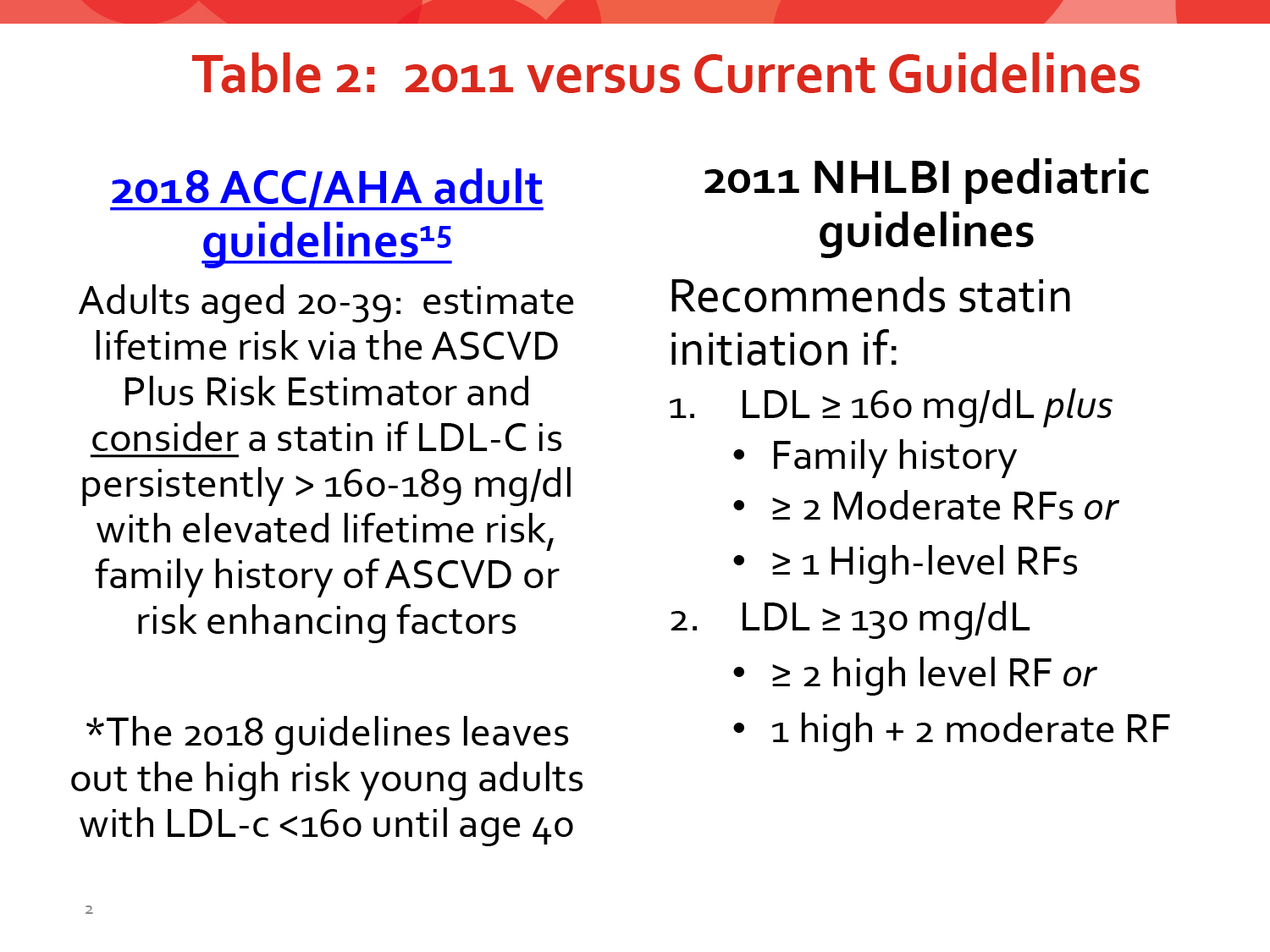
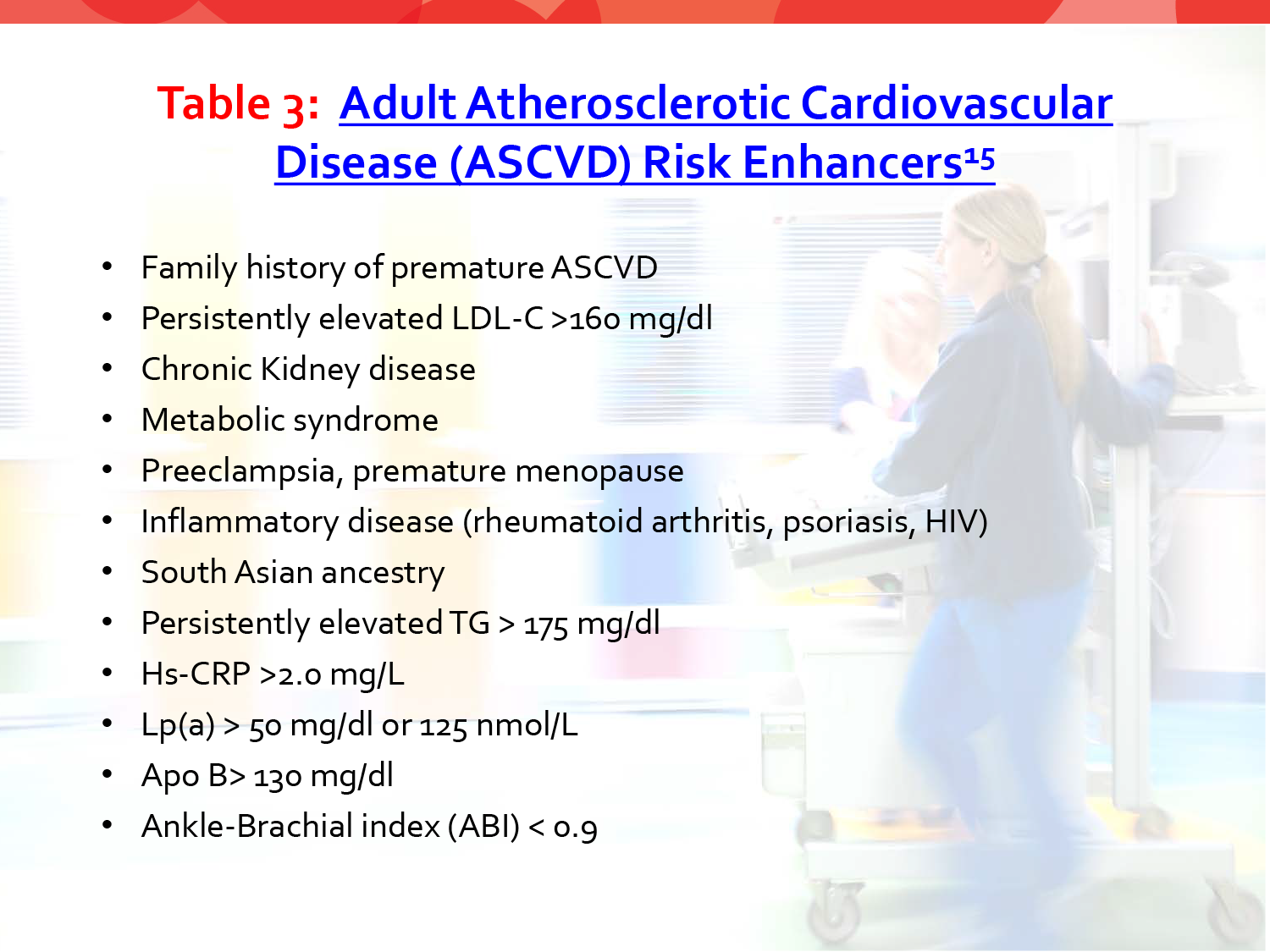
The ACC/AHA guidelines emphasize a heart healthy lifestyle across the lifespan. The differences in the new 2018 guidelines from the 2011 NHLBI guidelines are outlined in Table 2. Statin therapy is recommended without calculating 10-year atherosclerotic cardiovascular disease (ASCVD) risk in patients with severe hypercholesterolemia (LDL ≥190 mg/dl). There is a consensus for adjunct lipid-lowering treatment in youth when the LDL is >190 mg/dl. The 2011 Pediatric guidelines consider statin therapy for persistent LDL >130 with risk factors, and the 2018 Adult guidelines consider a statin for LDL >160 mg/dl with risk enhancing factors (see Table 3). The 2018 Adult guidelines do not recommend statin therapy for the young adult aged 20-39 years with LDL >160 mg/dl with the exception of patients with diabetes mellitus (DM) if the patient has had type 2 DM >10 years or type 1 DM >20 years.15
Closing Thoughts
Atherogenesis is a progressive disease that starts in childhood, especially in the presence of risk factors, and is most receptive to risk reduction in its earliest stages. A heart healthy lifestyle is recommended across the lifespan. The current adult guidelines are now in better alignment with the pediatric guidelines and best practices. Both prioritize treating individuals with risk enhancers. Given the gap in guidelines for young people aged 20-39, these patients should be engaged in shared decision making regarding therapy and must be encouraged to avoid modifiable risk factors such as poor nutrition, sedentary lifestyle, excess weight, and smoking.
References
- Tabas I, Williams KJ, Borén J. Subendothelial lipoprotein retention as the initiating process in atherosclerosis: update and therapeutic implications. Circulation 2007;116:1832-44.
- Virmani R, Robinowitz M, Geer JC, Breslin PP, Beyer JC, McAllister HA. Coronary artery atherosclerosis revisited in Korean war combat casualties. Arch Pathol Lab Med 1987;111:972-76.
- Mcnamara JJ, Molot MA, Stremple JF, Cutting RT. Coronary artery disease in combat casualties in Vietnam. JAMA 1971;216:1185-87.
- Newman WP 3rd, Freedman DS, Voors AW, et al. Relation of serum lipoprotein levels and systolic blood pressure to early atherosclerosis. The Bogalusa Heart Study. N Engl J Med 1986;314:138-44.
- Berenson GS, Srinivasan SR, Bao W, Newman WP 3rd, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med 1998;338:1650-56
- McGill HC, McMahan CA. Determinants of atherosclerosis in the young. Pathobiological Determinants of Atherosclerosis in Youth (PDAY) Research Group. Am J Cardiol 1998;82:30T-36T.
- Gidding SS, McMahan CA, McGill HC, et al. Prediction of coronary artery calcium in young adults using the pathobiological determinants of atherosclerosis in youth (PDAY) risk score: The CARDIA study. Arch Intern Med 2006;166:2341-47.
- Raitakari OT, Juonala M, Kahonen M, et al. Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: the Cardiovascular Risk in Young Finns Study. JAMA 2003;290:2277-83.
- Davis PH, Dawson JD, Riley WA, Lauer RM. Carotid intimal-medial thickness is related to cardiovascular risk factors measured from childhood through middle age the Muscatine Study. Circulation 2001;104:2815-19.
- Li S, Chen W, Srinivasan SR, et al. Childhood cardiovascular risk factors and carotid vascular changes in adulthood: The Bogalusa Heart Study. JAMA 2003;290:2271-76.
- Davis PH, Dawson JD, Riley WA, Lauer RM. Carotid intimal-medial thickness is related to cardiovascular risk factors measured from childhood through middle age. The Muscatine Study. Circulation 2001;104:2815-19.
- Mietus-Snyder M, Krauss RM. Lipid metabolism in children and adolescents: Impact on vascular biology. J Clin Lipidol 2008;2:127-37.
- Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents, National Heart, Lung, and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics 2011;128:S213-56.
- Gooding HC, Rodday AM, Wong JB, et al. Application of pediatric and adult guidelines for treatment of lipid levels among US adolescents transitioning to young adulthood. JAMA Pediatr 2015;169:569-74.
- Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the management of blood cholesterol: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019;73:3168-3209.
Keywords: Pediatrics, Child, Hypercholesterolemia, Hydroxymethylglutaryl-CoA Reductase Inhibitors, Risk Factors, Plaque, Atherosclerotic, Body Mass Index, Apolipoproteins B, National Heart, Lung, and Blood Institute (U.S.), Aortic Coarctation, Cardiovascular Diseases, Coronary Vessels, Blood Pressure, Atherosclerosis, Dyslipidemias, Lipoproteins, LDL, Carotid Arteries, Aorta, Diabetes Mellitus, Type 2, Risk Reduction Behavior, Smoking, Myocytes, Smooth Muscle, Extracellular Matrix, Ultrasonography, Neoplasms, Cholesterol, Primary Prevention, Triglycerides, Cohort Studies
< Back to Listings