Thromboangiitis Obliterans (Buerger's Disease)
Buerger's disease or Thromboangiitis Obliterans (TAO) is a segmental non-atherosclerotic inflammatory condition that affects the small and medium sized arteries and veins of the extremities. It was first described in 1908 by Dr. Leo Buerger.1 TAO is more common in men, and is usually diagnosed before 50 years of age. TAO is closely linked to tobacco use, although limited research has suggested that moderate to severe periodontal disease may also be associated with the development of TAO.2
Phases of TAO
There are three phases described in patients with TAO:
- Acute phase: An initial inflammatory process forms an intraluminal hypercellular and inflammatory thrombus which occludes the affected vessel lumen.3 Generally, there is sparing of the vessel wall.4 Although local inflammation is central to this acute phase, inflammatory markers such as C-reactive protein (CRP) and erythrocyte sedimentation rates (ESR) are typically normal.5
- Subacute phase: The thrombus organizes in the setting of ongoing inflammation.
- Chronic phase: The inflammatory process subsides and non-inflammatory, fibrotic thrombus forms.4
In all phases, the internal elastic lamina is preserved - in contrast to atherosclerosis or vasculitis. 5
Clinical Manifestations
TAO usually presents in smokers less than 50 years of age with two or more extremities affected.4 The majority of patients present with ischemic ulceration affecting the upper and lower extremities.6,7 (Image 1). Patients may present with pain in the digits, associated with rubor or cyanosis, which can then progress to ulceration. Some patients present less acutely with complaints such as claudication or rest pain which can mimic peripheral artery disease (PAD). Even more subtlety, patients may present with superficial thrombophlebitis that is sometimes associated with tender erythematous subcutaneous nodules that follow a venous distribution.5 Lastly, TAO has presented with Raynaud's phenomenon (secondary).8
Image 1
Diagnosis
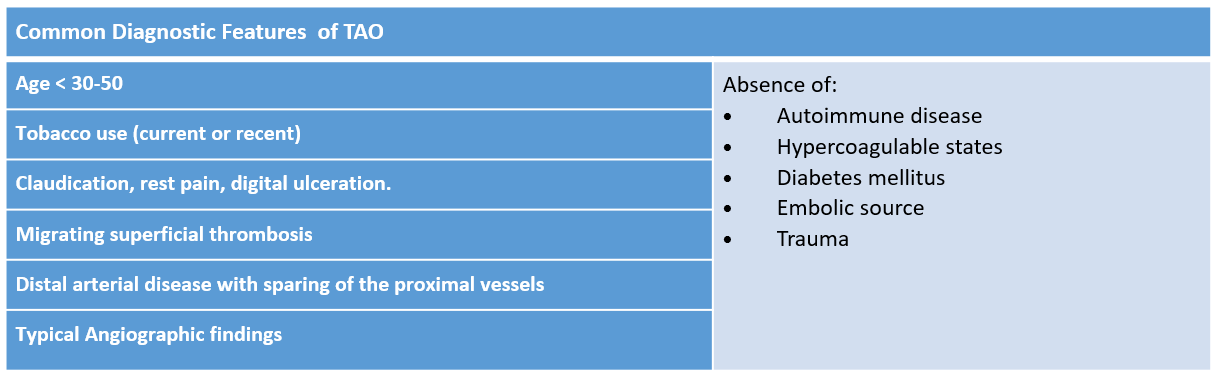
The diagnosis of TAO is based on history, physical examination and diagnostic imaging. It is a diagnosis of exclusion and requires the exclusion of a variety of conditions such as peripheral artery disease, hypercoagulable states, cardiac arrhythmia (with resultant emboli to the digits), vasculitis, and repetitive trauma, to name a few. Table 1 summarizes major elements of various proposed diagnostic criteria for TAO.9,10,11
Table 1
A thorough medical history should include any form of tobacco use (i.e. cigarettes, cigars, smokeless tobacco, electronic cigarettes), nicotine replacement therapy, and cannabis use. Exam should include a full and thorough pulse exam, auscultation for bruits, the Allen test, neurologic exam and visual inspection of the affected limbs.
Workup should aim to exclude the above differential diagnosis and include:
- Laboratory testing: Serologies for vasculitis and autoimmune syndromes (e.g. CREST syndrome, scleroderma), hypercoagulable states that may result in arterial clots (hyperhomocysteinemia, antiphospholipid antibodies), toxicology screen screening for nicotine and other vasoactive substances (cocaine, amphetamines), blood viscosity, serum and urine electrophoresis.
- An ankle brachial index (ABI) or wrist brachial index (WBI): While a decreased ABI/WBI is revealing, it may be normal in patients with TAO due to the distal nature of the occlusions. Obtaining digit pressures and calculating the digit-brachial index is useful to identify more distal disease. Pulse volume recordings (PVRs) are another tool for measuring arterial perfusion. PVRs obtained from the digits aids in identifying distal perfusion deficits. In unilateral presentations, ruling out arterial thoracic outlet syndrome can be useful.
- Transthoracic and transesophageal echocardiography: Intracardiac sources of embolism should be ruled out with echocardiography (cardioembolic).
- CT angiography: Performed to evaluate for aortic sources of embolism (atherosclerosis, and aneurysm/dissection with associated thrombus).
- Catheter-based angiography: Catheter-based angiography is preferred over magnetic resonance angiography (MRA)/computed tomography angiography (CTA) due to higher spatial resolution. Typically noted distally at the level of the wrists and ankles are small and medium vessel segmental occlusions with associated collateral formation (i.e. "corkscrew" collaterals) as is seen in Image 2.12 Such occlusions are seen in the absence of atherosclerosis or aneurysm formation.
- A biopsy is not typically needed. It may, however, offer a definitive diagnosis and should be reserved for atypical presentations, or to rule out TAO.
Image 2: Catheter Based Angiography
Treatment
Tobacco Cessation:
Complete cessation of all tobacco products is the mainstay of treatment. It is unclear whether nicotine replacement can exacerbate the disease, but most recommend complete avoidance. Non-nicotine containing agents to help aid smoking cessation such as Buproprion or Varenicline should be encouraged in patients with TAO.13 When symptoms persist despite nicotine abstinence, urine nicotine testing should be performed to verify abstinence as many patients continue to smoke despite the risk of amputation of the digits and more proximal extremities.13
Trigger Avoidance:
In additional to smoking cessation, patients should be educated on proper skin hygiene, daily foot checks, and proper footwear (to avoid trauma/rubbing). Avoiding cold exposures, as well as thermal, chemical or mechanical injury is important in preventing ulceration. Drugs that can cause peripheral vasoconstriction should be avoided.
Vasodilator therapy:
Vasodilator therapy with calcium channel blockers, nitrates, prostacyclin and phosphodiesterase inhibitors may theoretically alleviate symptoms of vasospasm. Of these, only Iloprost has been studied in patients with TAO. Intravenous Iloprost was compared to aspirin in 133 patients with TAO and critical limb ischemia. Of the patients treated with Iloprost, 58 of 68 (85%) showed improved ulcer healing and pain relief compared to only 11 of 65 (17%) of the patients in the aspirin group at 28 days.14 Unfortunately, Iloprost's benefits are limited to its intravenous form, as oral Iloprost was not effective in promoting ulcer healing.13 The prolonged infusion times of IV Iloprost make it challenging to administer in the outpatient setting and, thus, of limited use in the treatment of TAO, though repeat "daycare" treatments are potentially possible. Cilostazol, although not well studied in Buerger's, may have a role in reducing symptoms of digital ischemia.15
Interventional therapy:
Endovascular therapies are usually not indicated in TAO due to the distal nature of the disease. Intervention may be considered in patients with advanced, symptomatic disease if technically feasible. Kim, et al. demonstrated that revascularization can be performed with a high likelihood of technical success and is associated with an improved amputation-free survival at 3-year follow-up.16 Compared with autologous venous bypass, endovascular intervention yields similar rates of amputation-free survival at 3 years, but is associated with higher rates of re-intervention.17 Although there is limited data, sympathectomy has been shown to improve symptoms of TAO.18,19
Hyperbaric Oxygen Therapy:
Based on limited data, hyperbaric oxygen therapy (HBOT) may provide some benefit in TAO. A retrospective analysis of hyperbaric therapy compared HBOT to conventional treatment alone and showed that HBOT resulted in improved wound healing and pain control compared to conventional therapy. In this study, 21 of 47 patients in the hyperbaric group healed completely compared to 11 of 50 patients that received conventional therapy alone. At 10 months, there was less amputation observed in the HBOT group (2 of 47) compared to conventional therapy (13 of 50).20
Bosentan Therapy:
Bosentan therapy was described in a case series of eight patients who failed aggressive medical therapy with antiplatelet therapy, vasodilators and IV Alprostadil. Complete healing was observed in six patients. Given the absence of other compelling treatment options, Bosentan may be considered in severe, refractory cases of TAO.21
Autologous Bone-Marrow mononuclear cell implantation (BM-MNC):
Long term clinical benefits were observed in a small group of patients with that received BM-MNC. Twenty-five patients with PAD and 26 patients with TAO received BM-MNC and 46 critical limb ischemia (CLI) patients served as control. TAO patients had a higher amputation free survival rate (95%) at 4 years compared to those with PAD (48%) and control (0%). An improvement in transcutaneous oxygen pressures was noted at 3 years.22 A similar trend in amputation free survival was noted by Matoba et al.23
Summary
Despite being described over a century ago, TAO remains poorly understood and challenging to treat. Complete cessation of tobacco is still the mainstay of therapy for TAO as other therapies do not treat the root cause of the inflammatory response. Physicians must maintain a high clinical suspicion for TAO in young male smokers presenting with digital ulceration or symptoms related to lower extremity arterial insufficiency.
References
- Thromboangiitis obliterans: a study of the vascular lesions leading to presenile spontaneous gangrene by Leo Buerger, M.D.: published, 1908 in the American Journal of the Medical Sciences. Am J Med Sci 1973; 266:278-91.
- Iwai T, Inoue Y, Umeda M, et al. Oral bacteria in the occluded arteries of patients with Buerger disease. J Vasc Surg 2005;42:107–15.
- Sayin A, Bozkurt AK, Tüzün H, Vural FS, Erdog G, Ozer M. Surgical treatment of Buerger's disease: experience with 216 patients. Cardiovasc Surg 1993;1:377-80.
- Olin JW, Shih A. Thromboangiitis obliterans (Buerger's disease). Curr Opin Rheumatol 2006;18:18-24.
- Piazza G, Creager MA. Thromboangiitis obliterans. Circulation 2010;121:1858–61.
- Olin JW, Young JR, Graor RA, Ruschhaupt WF, Bartholomew JR. The changing clinical spectrum of thromboangiitis obliterans (Buerger's disease). Circulation 1990;82:IV3-8.
- Sasaki S, Sakuma M, Yasuda K. Current status of thromboangiitis obliterans (Buerger's disease) in Japan. Int J Cardiol 2000;75:S175-81.
- Piazza G, Olin JW. "Thrombangiitis Obliterans (Buerger Disease)". In: Creager MA, Beckman J, Loscalzo J eds., Vascular Medicine: A Companion to Braunwald's Heart Disease, 3rd edition.Elsevier;2018.
- Olin JW. Thromboangiitis obliterans (Buerger's disease). N Engl J Med 2000;343:864-69.
- Shionoya S. Diagnostic criteria of Buerger's disease. Int J Cardiol 1998;66:243-45.
- Papa MZ, Rabi I, Adar R. A point scoring system for the clinical diagnosis of Buerger's disease. Eur J Vasc Endovasc Surg 1996;11:335-39.
- Taniguchi T, Higuchi T, Tazaki J, Saito N, Kimura T. Successful percutaneous transcatheter angioplasty of radial artery in thromboangiitis obliterans (Buerger's Disease). JACC Cardiovasc Interv. 2017;10:e205-e206.
- Fiessinger JN, Schafer M. Trial of iloprost versus aspirin treatment for critical limb ischaemia of thromboangiitis obliterans. The TAO Study. Lancet 1990;335:555–57.
- Oral iloprost in the treatment of thromboangiitis obliterans (Buerger's disease): a double-blind, randomised, placebo-controlled trial. The European TAO Study Group. Eur J Vasc Endovasc Surg 1998;15:300-7.
- Dean SM, Satiani B. Three cases of digital ischemia successfully treated with cilostazol. Vasc Med 2001;6:245-48.
- Kim DH, Ko YG, Ahn CM, et al. Immediate and late outcomes of endovascular therapy for lower extremity arteries in Buerger disease. J Vasc Surg 2018;67:1769–77.
- Ye K, Shi H, Qin J, et al. Outcomes of endovascular recanalization versus autogenous venous bypass for thromboangiitis obliterans patients with critical limb ischemia due to tibioperoneal arterial occlusion. J Vasc Surg 2017;66:1133–42.
- Talwar S, Prasad P. Single-stage lumbar sympathectomy and omentopexy: a new surgical approach towards patients with Buerger's disease. Trop Doct 2001;31:73-75.
- De Giacomo T, Rendina EA, Venuta F, et al. Thoracoscopic sympathectomy for symptomatic arterial obstruction of the upper extremities. Ann Thorac Surg 2002;74:885-88.
- Hemsinli D, Altun G, Kaplan ST, Yildirim F, Cebi G. Hyperbaric oxygen treatment in thromboangiitis obliterans: a retrospective clinical audit. Diving Hyperb Med 2018;48:31–35.
- Narváez J, García-Gómez C, Álvarez L, et al. Efficacy of bosentan in patients with refractory thromboangiitis obliterans (Buerger disease): A case series and review of the literature. Medicine (Baltimore) 2016;95:e5511.
- Idei N, Soga J, Hata T, et al. Autologous bone-marrow mononuclear cell implantation reduces long-term major amputation risk in patients with critical limb ischemia: a comparison of atherosclerotic peripheral arterial disease and Buerger disease. Circ Cardiovasc Interv 2011;4:15-25.
- Matoba S, Tatsumi T, Murohara T, et al. Long-term clinical outcome after intramuscular implantation of bone marrow mononuclear cells (Therapeutic Angiogenesis by Cell Transplantation [TACT] trial) in patients with chronic limb ischemia. Am Heart J 2008;156:1010-08.
Clinical Topics: Arrhythmias and Clinical EP, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Vascular Medicine, Implantable Devices, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Heart Failure and Cardiac Biomarkers, Interventions and Imaging, Interventions and Vascular Medicine, Angiography, Echocardiography/Ultrasound, Magnetic Resonance Imaging, Nuclear Imaging
Keywords: Thromboangiitis Obliterans, Angiography, Coronary Angiography, C-Reactive Protein, Peripheral Arterial Disease, Ankle Brachial Index, Troleandomycin, Gangrene, Echocardiography, Transesophageal, Magnetic Resonance Angiography, CREST Syndrome, Blood Viscosity, Hyperhomocysteinemia, Blood Sedimentation, Inflammation, Antibodies, Antiphospholipid, Thoracic Outlet Syndrome, Aneurysm, Arrhythmias, Cardiac, Tobacco Use, Pain, Physical Examination, Biopsy, Cyanosis, Auscultation, Thrombophlebitis, Amphetamines, Periodontal Diseases, Electrophoresis
< Back to Listings