Perfusion CMR for the Assessment of Ischemic Heart Disease
Introduction
Perfusion imaging with cardiovascular magnetic resonance (perfusion CMR) is a rapid, noninvasive test that is free of ionizing radiation. Over the last decade, it has been shown to be highly accurate, provide strong prognostic data, and reduce the number of unnecessary invasive angiographies in patients with stable chest pain. Perfusion CMR is attractive for a wide variety of patients early in the work-up of their symptoms. If positive, it provides strong guidance toward revascularization. If negative, it frequently provides important information on the underlying pathophysiology (e.g., microvascular disease or inflammation), which helps explain the symptoms and guide further medical therapy.
Evidence
Diagnostic accuracy of perfusion CMR has been evaluated in numerous studies with a total of more than 4,000 patients against invasive angiography with or without additional fractional flow reserve (FFR) as the reference standard. Meta-analyses show sensitivities of 89% (88-91%), specificities of 76% (73-78%), and accuracies of 86% versus invasive angiography,1 with slightly better numbers for higher field strengths (3 Tesla vs. 1.5 Tesla) or stricter angiographic criteria (70% stenosis vs. 50% stenosis).2 Similarly, data are slightly better when using FFR as the reference standard (89%/87%/88%).3 Diagnostic accuracy remains similar for men and women as well as for multivessel disease. The two largest studies comparing diagnostic accuracy of perfusion CMR to single photon emission tomography (SPECT) are MR-IMPACT II (Magnetic Resonance Imaging for Myocardial Perfusion Assessment in Coronary Artery Disease Trial) (multi-centre, ungated SPECT)4 and CE-MARC (Clinical Evaluation of Magnetic Resonance Imaging in Coronary Heart Disease) (single centre, gated SPECT)5 both of which demonstrated superior diagnostic accuracy of perfusion CMR versus SPECT, a finding that is further strengthened by meta-analyses.2,3
Similarly, a strong prognostic power of perfusion CMR has been demonstrated in large cohorts of patients, summarized in Lipinski et al.6 In this meta-analysis of 11,636 patients with an average follow-up time of 32 months, the event rates for cardiovascular death or myocardial infarction were 0.3 ± 0.3% and 0.4 ± 0.3% in case of a negative CMR study (0.8 ± 0.7% for the combined end-point of cardiovascular death or myocardial infarction). In case of a positive stress CMR, event rates were 2.8 ± 1.6%, 2.6 ± 2%, and 4.9 ± 3.1% (p < 0.0001 for all), resulting in hazard ratios of 7.7, 6.96, and 6.5. Similar to SPECT, a cut-off value of approximately ≥10% ischemic myocardium seems to optimally define patients who profit from revascularization.7 The presence of a previous myocardial infarction or diffuse fibrosis/edema8 is an additional strong prognostic factor.
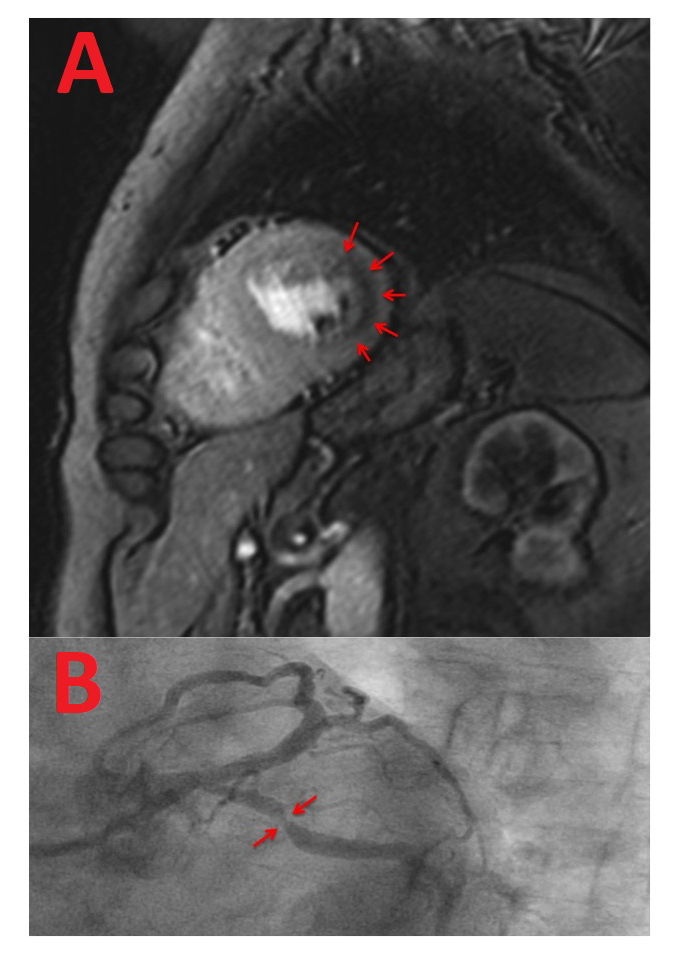
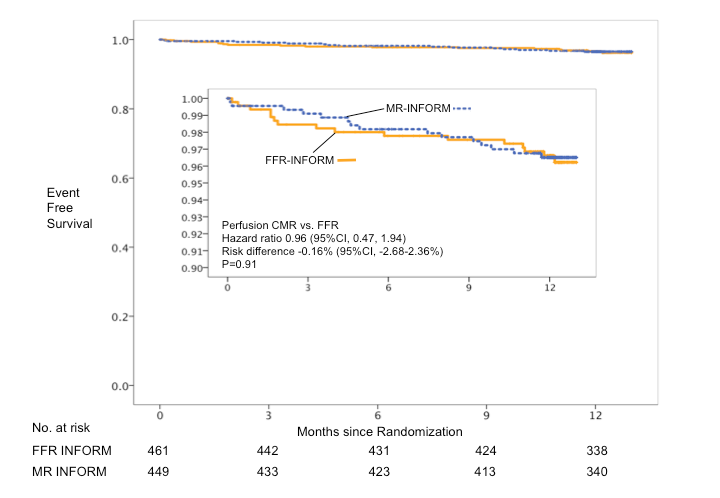
Recently, the results from the MR-INFORM trial (Stress Perfusion Imaging to Guide the Management of Patients With Stable Coronary Artery Disease), an international, randomized controlled clinical-effectiveness trial, were published.9 The trial demonstrated in 918 patients with stable chest pain and intermediate to high pre-test likelihood for coronary artery disease (CAD) that perfusion CMR can guide further management as effectively as invasive angiography supported by FFR (Figure 1). Patients with stable chest pain and ≥2 risk factors or positive exercise electrocardiogram (ECG) were randomized into a noninvasive arm guided by stress perfusion CMR or an invasive arm guided by angiography and FFR. All patients received guideline-directed medical therapy. In the CMR-informed arm, only 40.5% required an invasive angiography despite an intermediate to high pre-test likelihood (74% according to a modified Diamond and Forrester score), and fewer patients than in the FFR-informed arm were revascularised (35.7% CMR guided vs. 45.0% invasively guided; p = 0.005). The occurrence of angina pectoris (50.8% vs. 56.2%; p = 0.21) or major cardiac events (death, myocardial infarction, and target vessel revascularization) (3.56% vs. 3.72%; hazard ratio -2.68-2.36; p = ns) was identical by perfusion CMR or invasively guided therapy (Figure 2). These data demonstrate that perfusion CMR is as safe and effective as invasive coronary angiography supported by FFR to guide the management of patients with stable chest pain.
Although the data on cost-effectiveness from the MR-INFORM trial are still outstanding, calculations based on CE-MARC data10 and Euro-CMR data11 and compared with computed tomography angiography12 demonstrate cost savings for the majority of pathways using perfusion CMR.
Figure 1: Perfusion CMR During Adenosine Stress of a Patient in the MR-INFORM Trial
Figure 2: Kaplan-Meier Curves of Event-Free Survival of the MR-INFORM Trial
CMR in Patients With Chest Pain but no Significant CAD
CMR has been proven highly valuable in assessing the etiology of cardiovascular diseases due to its ability to assess function, regional fibrosis, edema due to inflammation, and microvascular flow. As such, CMR is now recommended after negative coronary angiography in patients with suspected troponin-positive acute coronary syndrome.13 In these patients, originally defined as myocardial infarction with nonobstructive coronary arteries, CMR has been reported to define an underlying etiology of the troponin rise in 87% of patients,14 demonstrating myocarditis, takotsubo cardiomyopathy, or acute myocardial infarction as the most frequent causes. Importantly, CMR can also recognize causes for chest pain in patients with low pre-test likelihood, such as pericarditis, myocarditis, or microvascular disease, which are missed if invasive coronary angiography or computed tomography coronary angiography are used to rule out coronary disease.
Guidelines Recommendations
Guidelines differentiate their recommendations into the diagnosis and the therapy of CAD. In the European Society of Cardiology guidelines, perfusion CMR is a Class IA indication to prove myocardial ischemia before revascularization, as well as for the work-up of symptomatic patients with intermediate (15-85%) pre-test probability.15,16 American College of Cardiology appropriate use criteria from 2014 regard perfusion CMR as appropriate in patients with intermediate pre-test probability and nondiagnostic exercise ECG as well as in patients with high pre-test probability independent of the interpretability of the exercise ECG.17 These guidelines are currently updated.
Summary
The evidence presented demonstrates the strong position of perfusion CMR in the work-up of patients with stable chest pain. Given the novel evidence, clinical practice may change toward examining a broader spectrum of patients with perfusion CMR. In patients with low to intermediate pre-test likelihood, a negative perfusion CMR conveys a good prognosis and frequently allows for the identification of the underlying non-coronary cause of the patients' symptoms. In patients with intermediate to high pre-test likelihood for CAD, the current invasive strategy can be safely replaced by a short, noninvasive imaging test.
References
- Jaarsma C, Leiner T, Bekkers SC, et al. Diagnostic performance of noninvasive myocardial perfusion imaging using single-photon emission computed tomography, cardiac magnetic resonance, and positron emission tomography imaging for the detection of obstructive coronary artery disease: a meta-analysis. J Am Coll Cardiol 2012;59:1719-28.
- Kiaos A, Tziatzios I, Hadjimiltiades S, Karvounis C, Karamitsos TD. Diagnostic performance of stress perfusion cardiac magnetic resonance for the detection of coronary artery disease: A systematic review and meta-analysis. Int J Cardiol 2018;252:229-33.
- Takx RA, Blomberg BA, El Aidi H, et al. Diagnostic accuracy of stress myocardial perfusion imaging compared to invasive coronary angiography with fractional flow reserve meta-analysis. Circ Cardiovasc Imaging 2015;8:e002666.
- Schwitter J, Wacker CM, van Rossum AC, et al. MR-IMPACT: comparison of perfusion-cardiac magnetic resonance with single-photon emission computed tomography for the detection of coronary artery disease in a multicentre, multivendor, randomized trial. Eur Heart J 2008;29:480-9.
- Greenwood JP, Maredia N, Younger JF, et al. Cardiovascular magnetic resonance and single-photon emission computed tomography for diagnosis of coronary heart disease (CE-MARC): a prospective trial. Lancet 2012;379:453-60.
- Lipinski MJ, McVey CM, Berger JS, Kramer CM, Salerno M. Prognostic value of stress cardiac magnetic resonance imaging in patients with known or suspected coronary artery disease: a systematic review and meta-analysis. J Am Coll Cardiol 2013;62:826-38.
- Shaw LJ, Berman DS, Picard MH, et al. Comparative definitions for moderate-severe ischemia in stress nuclear, echocardiography, and magnetic resonance imaging. JACC Cardiovasc Imaging 2014;7:593-604.
- Puntmann VO, Carr-White G, Jabbour A, et al. Native T1 and ECV of Noninfarcted Myocardium and Outcome in Patients With Coronary Artery Disease. J Am Coll Cardiol 2018;71:766-78.
- Nagel E, Greenwood JP, McCann GP, et al. Magnetic Resonance Perfusion or Fractional Flow Reserve in Coronary Disease. N Engl J Med 2019;380:2418-28.
- Walker S, Girardin F, McKenna C, et al. Cost-effectiveness of cardiovascular magnetic resonance in the diagnosis of coronary heart disease: an economic evaluation using data from the CE-MARC study. Heart 2013;99:873-81.
- Moschetti K, Petersen SE, Pilz G, et al. Cost-minimization analysis of three decision strategies for cardiac revascularization: results of the "suspected CAD" cohort of the european cardiovascular magnetic resonance registry. J Cardiovasc Magn Reson 2016;18:3.
- Pontone G, Andreini D, Guaricci AI, et al. The STRATEGY Study (Stress Cardiac Magnetic Resonance Versus Computed Tomography Coronary Angiography for the Management of Symptomatic Revascularized Patients): Resources and Outcomes Impact. Circ Cardiovasc Imaging 2016;9:e005171.
- Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2018;39:119-77.
- Pathik B, Raman B, Mohd Amin NH, et al. Troponin-positive chest pain with unobstructed coronary arteries: incremental diagnostic value of cardiovascular magnetic resonance imaging. Eur Heart J Cardiovasc Imaging 2016;17:1146-52.
- Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J 2019;40:87-165.
- Task Force Members, Montalescot G, Sechtem U, et al. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J 2013;34:2949-3003.
- Wolk MJ, Bailey SR, Doherty JU, et al. ACCF/AHA/ASE/ASNC/HFSA/HRS/SCAI/SCCT/SCMR/STS 2013 multimodality appropriate use criteria for the detection and risk assessment of stable ischemic heart disease: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons. J Am Coll Cardiol 2014;63:380-406.
Keywords: Coronary Angiography, Coronary Artery Disease, Troponin, Adenosine, Takotsubo Cardiomyopathy, Acute Coronary Syndrome, Myocarditis, Risk Factors, Constriction, Pathologic, Cost Savings, Cost-Benefit Analysis, Research Personnel, Follow-Up Studies, Angina Pectoris, Myocardial Infarction, Electrocardiography, Tomography, Emission-Computed, Single-Photon, Perfusion Imaging, Magnetic Resonance Imaging, Magnetic Resonance Spectroscopy, Pericarditis, Inflammation, Edema, Treatment Outcome, Myocardium, Angina, Stable
< Back to Listings