The Nuts and Bolts of an Inpatient Cardio-Oncology Consult Team
Introduction
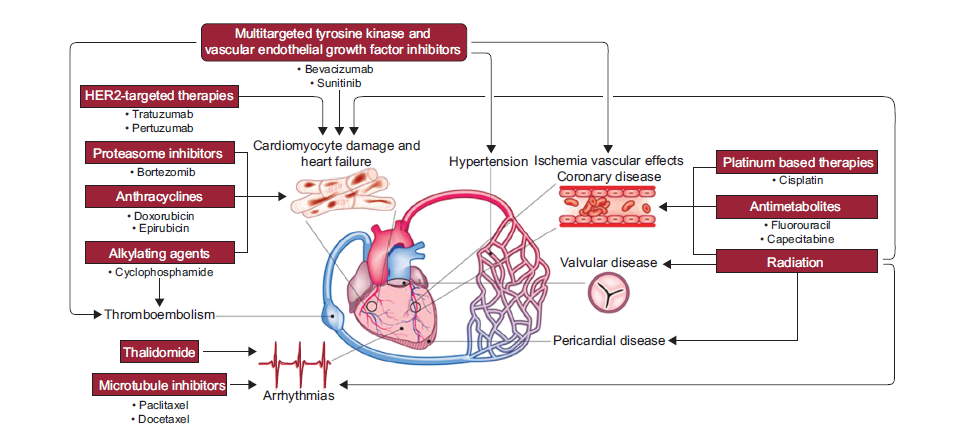
Cancer is a global burden. By the year 2030, 23.6 million new cancer cases are expected to be added annually to the global burden.1 Traditional cancer treatments such as anthracycline-based chemotherapies, monoclonal antibody-based therapies (e.g., trastuzumab), and radiation can have cardiac toxicities.2 In the last decade, novel cancer therapies or their combinations have improved cancer survivorship.3 These cancer therapies are associated with cardiovascular complications (Figure 1).3-5 Additionally, patients with cancer and survivors of cancer are often elderly and have new or preexisting cardiovascular comorbidities. Patients with pre-existing cardiovascular disease have an increased risk of cardiovascular toxicity.6 Cardiovascular complications of cancer therapy have a profound negative effect on the survival and quality of life of patients with cancer.7,8
Figure 1: Cardiovascular Toxicities of Cancer Therapies
Cancer therapies can affect the whole cardiovascular system, but these cardiotoxic effects are generally reported as changes in left ventricular (LV) ejection fraction.4,10 The most common cardiovascular adverse effects are LV dysfunction and heart failure (HF). Other adverse effects include hypertension, acute coronary syndromes, thromboembolic events, rhythm disturbances, and valvular and/or pericardial disease.10 Hence, prediction, early recognition, and timely management of cardiovascular complications in patients with cancer are gaining importance.11 This need gave birth to the concept of interdisciplinary cardiology-oncology (cardio-oncology) care delivered through teams of cardiologists, oncologists, and hematologists.3,5,12
Rationale, Goal, and Benefits of Multidisciplinary Cardio-Oncology Care
Rationale
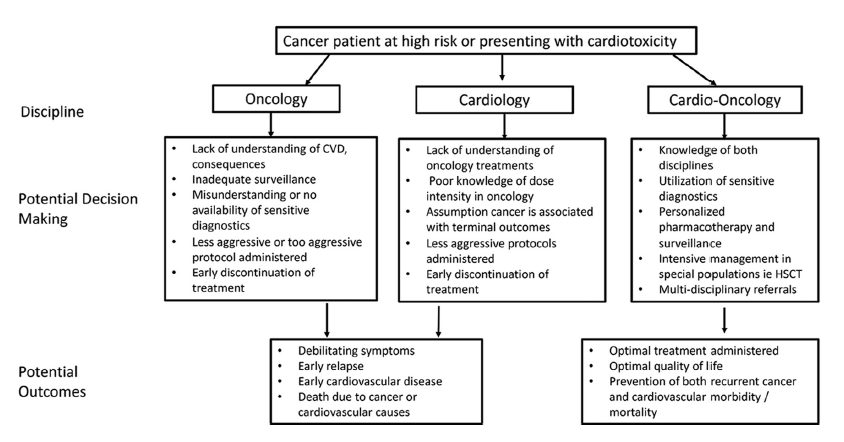
A cardiologist is not trained in cancer care and dosing strategies of cancer therapies, and an oncologist is not trained in cardiovascular care protocols. Hence, a cardiologist who is trained in basic oncology care and is familiar with cancer drug toxicities is the ideal cardio-oncology specialist (Figure 2).13
Figure 2: Rationale of Cardio-Oncology Care
Goal
The main goal of a cardio-oncology service is to improve treatment decision-making and patient outcomes through effective communication and coordination between the health care team members and patients.14
Benefits
The multidisciplinary team improves patient care in the following ways:14
- Optimizes acute and long-term cardiovascular health of patients with cancer
- Prevents cardiovascular complications if possible
- Ensures early diagnosis and timely management of cardiovascular complications
- Reduces the need to interrupt cancer therapy
- Improves survival and quality of life of patients with cancer
Implementation of the Inpatient Cardio-Oncology Team
Organizational Structure
The organizational structure of an inpatient cardio-oncology team would depend on the size of the hospital, burden of patients with cancer, and facilities available. To set up a cardio-oncology team, certain organizational, structural (such as an intensive care unit [ICU] and requisite infrastructure of cardiac-specific procedures), laboratory, and radiology facilities are required (Table 1). The inpatient cardio-oncology team should ideally have the following components:14,15
- A lead cardiologist and lead oncologist with their respective teams to work collaboratively on all aspects of cardio-oncology care
- Hematologists, cardiologists, cardiac surgeons, cardiac sub-specialists (electrophysiology, imaging, intervention, and HF), radiation oncologists, medical oncologists, surgical oncologists, and trainee students
- A lead administrator and team to help with budgetary and operational planning
- A common communication platform, such as electronic health record, and technicians and staff maintaining it
- Cardio-oncology nurse coordinator
- Cardio-oncology expert to train other doctors and staff on a new team (trainer to train)
- Radiology technicians
- Clinical psychologist
- Clinical support staff, such as medical assistants, dieticians, nurses (trained in cardiology and oncology care), nurse practitioners, and physician assistants
- Patient and patient's family and community support
Table 1: Nuts and Bolts of Inpatient Cardio-Oncology Team in Hospitals
| Requirements | District Hospitals | Tertiary Hospitals | Super-Specialty Hospitals |
| Burden of Patients With Cancer | <10 patients/week | >10 patients/week | >20 patients/week |
| Hospital Structure |
|
|
|
| Multidisciplinary Teams | |||
| Organization |
|
|
Apart from features mentioned under tertiary hospitals, has specialized centers for
|
| Round-the-Clock Facility | 24/7 services recommended | Available only in emergency/acute cases | Available only in emergency/acute cases |
| Cancer Survivorship Programs | Not available | Available | Available |
| Structured Training Programs | Not available | Available for healthcare professionals | Available both for patients and healthcare professionals |
| Technical Resources | |||
| Cardiac Imaging |
|
|
|
| Cardiac Biomarkers | Available | Available | Apart from standard biomarkers, new biomarkers, and genetic testing facility |
| Procedures | Cardiac catheterization, devices, and surgeries; electrophysiology services (if not available or for complex cases, refer to bigger regional facilities) | Cardiac catheterization, devices, and surgeries; electrophysiology services | Cardiac catheterization, devices, and surgeries; electrophysiology services; cardiac transplant facility |
| Data Review |
|
|
|
**The drawbacks of cardiac magnetic resonance, cardiac CT, and positron emission tomography CT are cost and availability.23
Reproduced with permission from Lancellotti et al.14,20
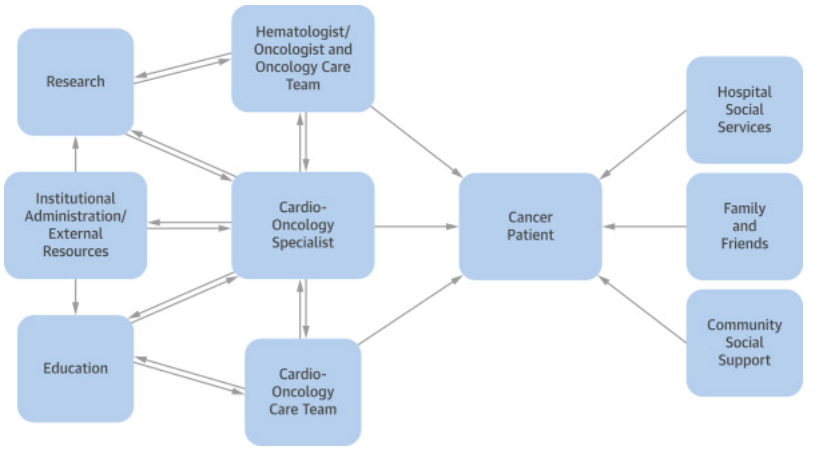
The cardio-oncology care model will work only if there is proper communication among the players and if there is effective feedback, training, and research at every level to improve cancer and cardiovascular care (Figure 3). This will also ensure patients' safety through timely detection and management of cardiovascular toxicities.16
Figure 3: Inpatient Cardio-Oncology Care Model
Roles, Responsibilities, and Rationale of an Inpatient Cardio-Oncology Team
Patient
The lead cardiologist in the team is the main cardio-oncology specialist and is expected to have expertise in diagnosing and predicting cardiac abnormalities, including HF on the basis of physical exam, clinical signs and symptoms, and high-resolution imaging.11,16,17 The oncologist and the cardiologist address the main cancer disease and associated cardiovascular complications, respectively, but other players are equally necessary for holistic management of the patient and for successful implementation of the cardio-oncology care protocol.11,16
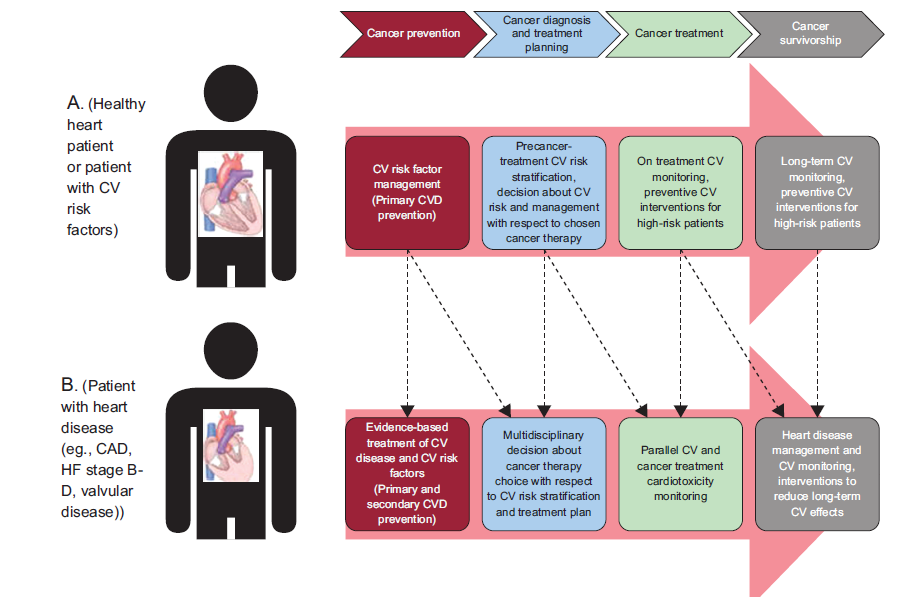
Each hospital should have a proper cardio-oncology protocol made in consultation with the lead cardiologist and oncologist to handle all cardiovascular complexities before, during, and after cancer therapy.15 These protocols should cover areas such as expected cardiovascular side effects of cancer therapy, notification of the cardio-oncology team, diagnosis and treatment of cardiovascular complications, and protocols for supportive treatments like stenting, psychotherapy, and physical therapy. This will provide a continuum of cardio-oncology care right from diagnosis of cancer to therapy and through survivorship (Figure 4).18
Figure 4: Continuum of Care Through a Cardio-Oncology Unit
At the time of a patient's admission, each team member should meet with the patient to identify care needs and review and plan treatment strategies. The team should then meet to integrate their treatment strategies, and this should be reviewed by the cardio-oncology specialist before starting the treatment. The patient's physical, mental, and social conditions should be considered while formulating treatment strategies to ensure treatment adherence.17
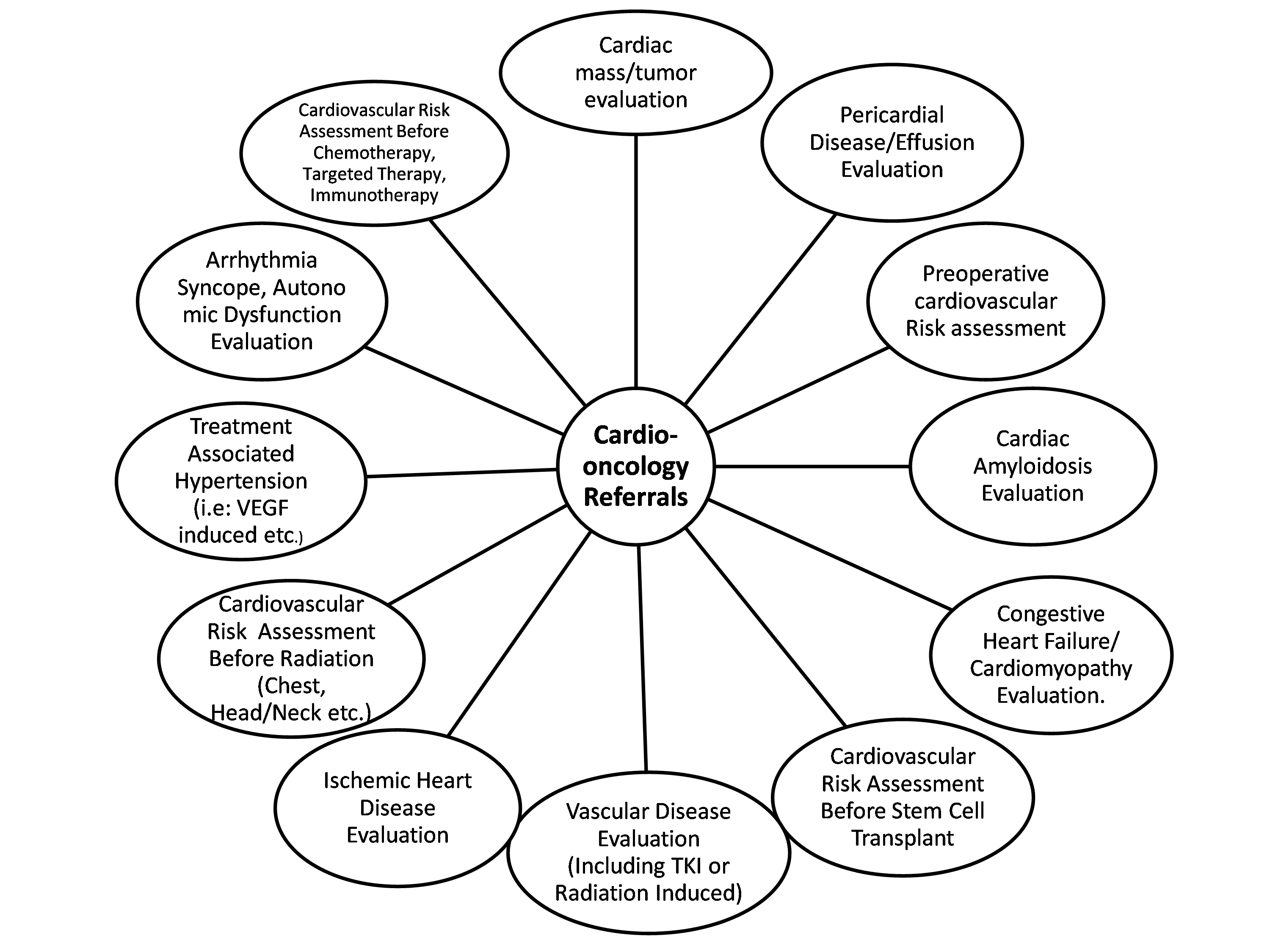
Before starting any cancer therapy, hematopoietic stem cell transplant, radiotherapy, or any cancer-related surgery, cardiovascular risk assessment should be performed through detailed history, physical examination, electrocardiogram, and echocardiogram. This protocol for appropriate cardiovascular evaluation should be followed up during and after the therapy, procedure, or surgery as required (Figure 5).12,15,17,19-21
Figure 5: Referrals to a Cardiologist15
Every inpatient should receive regular cardio-oncology consults along with round-the-clock monitoring for any cardiovascular toxicity. Cardiovascular testing should be done for all patients to assess the risk. Standard echocardiography and cardiac biomarkers should be performed for all. Advanced cardiac testing like newer biomarkers, genetic testing, cardiac magnetic resonance, CT, and positron emission tomography CT should be built into the protocol for complex cases.12,15,17,19-21 Seamless maneuvering of the patient for cardiac imaging tests, laboratory samples, doctor visits, and medication timing and monitoring is made possible through the coordination among the clinical support staff, nurses, and doctors who are involved in patient care.22
The outpatient cardio-oncology clinic follow-up should be arranged prior to discharge and before the patient is formally handed over to the cardio-oncology team there. Also, every patient should be assigned a cardio-oncology nurse coordinator prior to discharge to oversee patient education and adherence to treatment. Regular meetings with nurse coordinator will also help in early identification of potential cardiovascular complications post-therapy.12,15,17,19-21
Supporting Care
Where possible, every patient should be enrolled in a cancer survivorship program with special cardio-oncology nurse coordinator and special educators and into a cancer survivor support group to help foster positive rehabilitation. Each patient should also be assigned to a psychologist to evaluate the patient's stress, anxiety, and depression level before, during, and after treatment. Patients with cancer would need proper diet to recover from the brunt of chemotherapy, and a dietician plays an important role in that.12,15,17,19,21
Physicians, Nurses, and Staff
A cardio-oncology trainer should conduct regular staff training in cardiology and oncology to keep the staff informed about the latest treatments, potential cardiovascular toxicities, early identification, and emergency first aid. All new cardiologists and oncologists should be regularly involved in training.13,15
Challenges and Opportunities
The cardio-oncology care model is a relatively new field. Clinicians often face the dilemma whether give preference to the cancer status of the patient or to the cardiovascular toxicity. There are many unanswered questions, such as how long to provide cardioprotection, whether biomarkers should be integrated into the cardioprotection protocol, and, if yes, which biomarkers to use and at what stage in the patient's journey.23
Lack of awareness about this integrated practice, its availability in very few centers, lack of proper protocols for decision-making, and lack of resources to set up such a team are some of the key challenges in implementing the cardio-oncology program.24 Additionally, it is difficult to get skilled medical experts and supporting staff. If such a program gets implemented, the cost is high and often not covered by patients' insurance.24,25 However, in the United States, the insurance sector is becoming sensitive toward cardio-oncology care reimbursement with programs like the Quality Payment Program. Physicians should be careful, however, about how they are documenting cardio-oncology care so that their patients can be properly reimbursed.25 Recognizing the need for cardio-oncology, many funding agencies are coming forward to support these programs, such as pharmaceutical industry and philanthropic initiatives. National cardiology societies and the National Institutes of Health are providing research funding to improve the care model.24
Although several hospitals are recognizing the growing need of an inpatient cardio-oncology team, there is lack of direct evidence that these teams are more successful than usual care in reducing LV dysfunction in an oncology setting.13 Therefore, convincing hospital management to set up this specialized unit is a challenge.
However, a 5-year study from United Kingdom showed that 93.8% of the patients with cancer with LV systolic dysfunction who were treated in a cardio-oncology unit showed significant improvement in LV ejection fraction at a median follow-up of 360 days (45% pre vs. 53% post; p < 0.001) and New York Heart Association class III-IV (22% pre vs. 10% post; p = 0.01).26
Additionally, the TITAN Study (Multidisciplinary Team Intervention in Cardio-Oncology) is likely to shed light on the advantages of a cardio-oncology unit.27 All hospitals with a cardio-oncology unit should collect data to help understand the advantages of this integrated program and to identify gaps in program implementations. This will help tremendously in improving cardio-oncology care in an ongoing manner.
Future Directions
Dedicated and continuous efforts should be made to coordinate medical education and training and to promote clinical research in cardio-oncology.14 All cardio-oncology program protocols should have appropriate quality control checkpoints to standardize patient monitoring during cancer therapies.14,21 Apart from fostering community education to make patients aware of the cardiotoxic effects of their chemotherapy, cardio-oncology programs should to be publicized in primary health centers and all hospitals providing oncology care. Oncologists, nurses, patients, and their attendants should be trained to recognize signs and symptoms of cardiotoxicity.15 Because cardio-oncology care is a growing field, there is need for proper fellowship programs to train cardiologists in cancer-cardiovascular care.15
References
- Cancer Statistics (National Institute of Cancer website). 2018. Available at: https://www.cancer.gov/about-cancer/understanding/statistics. Accessed September 7, 2019.
- Lenneman CG, Sawyer DB. Cardio-Oncology: An Update on Cardiotoxicity of Cancer-Related Treatment. Circ Res 2016;118:1008-20.
- DeSantis CE, Lin CC, Mariotto AB, et al. Cancer treatment and survivorship statistics, 2014. CA Cancer J Clin 2014;64:252-71.
- Moslehi JJ. Cardiovascular Toxic Effects of Targeted Cancer Therapies. N Engl J Med 2016;375:1457-67.
- Truong J, Yan AT, Cramarossa G, Chan KK. Chemotherapy-induced cardiotoxicity: detection, prevention, and management. Can J Cardiol 2014;30:869-78.
- Cardinale D, Biasillo G, Cipolla CM. Curing Cancer, Saving the Heart: A Challenge That Cardioncology Should Not Miss. Curr Cardiol Rep 2016;18:51.
- Oliveira GH, Mukerji S, Hernandez AV, et al. Incidence, predictors, and impact on survival of left ventricular systolic dysfunction and recovery in advanced cancer patients. Am J Cardiol 2014;113:1893-8.
- Wang SY, Long JB, Hurria A, et al. Cardiovascular events, early discontinuation of trastuzumab, and their impact on survival. Breast Cancer Res Treat 2014;146:411-9.
- Plana JC, Galderisi M, Barac A, et al. Expert consensus for multimodality imaging evaluation of adult patients during and after cancer therapy: a report from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 2014;27:911-39.
- Guha A, Armanious M, Fradley MG. Update on cardio-oncology: Novel cancer therapeutics and associated cardiotoxicities. Trends Cardiovasc Med 2019;29:29-39.
- Lenihan DJ, Hartlage G, DeCara J, et al. Cardio-Oncology Training: A Proposal From the International Cardioncology Society and Canadian Cardiac Oncology Network for a New Multidisciplinary Specialty. J Card Fail 2016;22:465-71.
- Barros-Gomes S, Herrmann J, Mulvagh SL, Lerman A, Lin G, Villarraga HR. Rationale for setting up a cardio-oncology unit: our experience at Mayo Clinic. Cardiooncology 2016;2:5.
- Pituskin E, Paterson I, Cox-Kennett N, Rothe D, Perri M, Becher H. The Role of Cardio-Oncology in the Interprofessional Care of Adult Patients Receiving Cancer Therapy. Semin Oncol Nurs 2017;33:384-92.
- Lancellotti P, Suter TM, López-Fernández T, et al. Cardio-Oncology Services: rationale, organization, and implementation. Eur Heart J 2019;40:1756-63.
- Fradley MG, Brown AC, Shields B, et al. Developing a Comprehensive Cardio-Oncology Program at a Cancer Institute: The Moffitt Cancer Center Experience. Oncol Rev 2017;11:340.
- Okwuosa TM, Barac A. Burgeoning Cardio-Oncology Programs: Challenges and Opportunities for Early Career Cardiologists/Faculty Directors. J Am Coll Cardiol 2015;66:1193-7.
- Parent S, Pituskin E, Paterson DI. The Cardio-oncology Program: A Multidisciplinary Approach to the Care of Cancer Patients With Cardiovascular Disease. Can J Cardiol 2016;32:847-51.
- Barac A, Murtagh G, Carver JR, et al. Cardiovascular Health of Patients With Cancer and Cancer Survivors: A Roadmap to the Next Level. J Am Coll Cardiol 2015;65:2739-46.
- Herrmann J, Loprinzi C, Ruddy K. Building a Cardio-Onco-Hematology Program. Curr Oncol Rep 2018;20:81.
- Asteggiano R, Suter TM, Bax JJ. Cardio-oncology: principles and organisational issues. e-Journal of Cardiology Practice 2019;16.
- Michel L, Rassaf T. Cardio-oncology: need for novel structures. Eur J Med Res 2019;24:1.
- Nhola LF, Villarraga HR. Rationale for Cardio-Oncology Units. Rev Esp Cardiol (Engl Ed) 2017;70:583-9.
- Ghosh AK, Walker JM. Cardio-Oncology - A new subspecialty with collaboration at its heart. Indian Heart J 2017;69:556-62.
- Okwuosa TM, Prabhu N, Patel H, et al. The Cardiologist and the Cancer Patient: Challenges to Cardio-Oncology (or Onco-Cardiology) and Call to Action. J Am Coll Cardiol 2018;72:228-32.
- Arnold AM, Biga C, Mariani D. How to Code and Bill for Cardio-Oncology (American College of Cardiology website). May 7, 2018. Available at: https://www.acc.org/latest-in-cardiology/articles/2018/05/07/08/34/how-to-code-and-bill-for-cardio-oncology. Accessed October 12, 2019.
- Pareek N, Cevallos J, Moliner P, et al. Activity and outcomes of a cardio-oncology service in the United Kingdom-a five-year experience. Eur J Heart Fail 2018;20:1721-31.
- Pituskin E, Haykowsky M, McNeely M, Mackey J, Chua N, Paterson I. Rationale and design of the multidisciplinary team IntervenTion in cArdio-oNcology study (TITAN). BMC Cancer 2016;16:733.
Keywords: Cardio-oncology, Acute Coronary Syndrome, Anthracyclines, Antineoplastic Combined Chemotherapy Protocols, Anxiety, Cardiotoxicity, Cardiovascular Diseases, Cardiovascular System, Continuity of Patient Care, Cytarabine, Comorbidity, Depression, Diet, Drug Industry, Early Diagnosis, Decision Making, Echocardiography, Electrocardiography, Education, Medical, Electronic Health Records, Electrophysiology, Etoposide, Fellowships and Scholarships, First Aid, Genetic Testing, Follow-Up Studies, Goals, Heart Failure, Hematopoietic Stem Cell Transplantation, Hypertension, Inpatients, Intensive Care Units, Magnetic Resonance Spectroscopy, Methotrexate, National Institutes of Health (U.S.), Monitoring, Physiologic, Nurse Practitioners, Nutritionists, Outpatients, Patient Care, Patient Care Team, Physical Examination, Physician Assistants, Positron-Emission Tomography, Psychotherapy, Quality Control, Quality of Life, Referral and Consultation, Risk Factors, Self-Help Groups, Stroke Volume, Surgeons, Survivors, Tomography, X-Ray Computed
< Back to Listings