State-of-the-Art Strategies for the Prevention of Ischemic Disease on Both Sides of the Atlantic
Rajeev Gupta and David Wood's important recent article in Lancet, "Primary Prevention of Ischemic heart disease: populations, individuals, and health professionals" opens by defining primordial prevention as "preventing the onset of disease before there is any evidence of the condition by addressing the underlying determinants in populations."1,2 Primary prevention addresses persons at high multifactorial risk of developing atherosclerotic vascular disease. Implicit is the reliance on the collective willpower of local and federal government to enact policy and legislation with these aims in mind.
The role of government is also covered extensively in the 2016 European Society of Cardiology (ESC) guidelines on primary prevention of atherosclerotic cardiovascular disease (ASCVD), but not dealt with in detail in the 2019 AHA/ACC prevention guidelines.3,4 The latter guidelines highlight social determinants of health but focus primarily on overall cardiovascular risk stratification, lifestyle and behavior, and risk factor modification in individuals and populations.
Gupta and Woods' article highlights many similarities and some differences in emphasis between the most recent primary prevention guidelines on each continent. We review here the main themes of Gupta and Woods' paper and discuss how the guidelines complement one another.
Primordial Prevention Targets
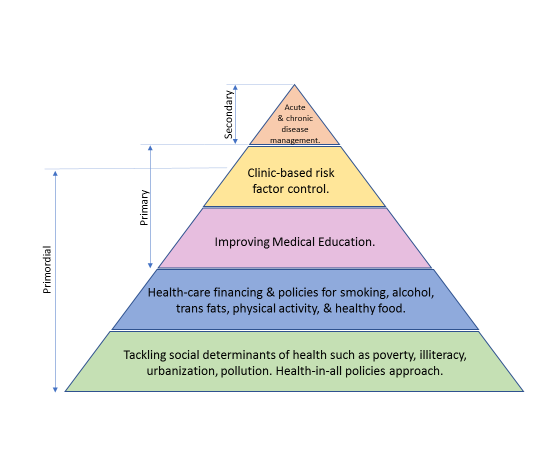
Gupta and Wood introduce an ischemic heart disease prevention pyramid (Figure 1) of which three out of five tiers focus on primordial prevention. The very foundation of their pyramid is built upon three pillars of primordial prevention, namely: 1) social determinants of health, 2) health policy and health financing, and 3) a focus on medical education.
Figure 1
The base of the cardiovascular prevention pyramid recognizes the fundamental importance of tackling social determinants such as pollution, mother and child nutrition, environmental policy, urban development goals that relate to safe neighborhoods and public areas that promote physical activity, poverty alleviation and livable wages, health literacy and education. The second tier relates primarily to health care policy and discusses the importance of universal health care coverage and health care financing, population-wide policy interventions that would address stress reduction, smoking and tobacco control, and promotion of healthy diets and exercise.
The 2019 ACC/AHA Primary Prevention Guidelines also include newly generated recommendations on the assessment of social determinants of health and gives a Class I indication that social determinants of health should inform optimal implementation of treatment recommendations for prevention. Table 1 is an adaptation of determinants to consider in the prevention of cardiovascular disease (CVD).
Table 1
| Governmental Restrictions and Mandates | Legislation on composition of foods to reduce energy density, salt and saturated fat, and sugar content of foods and beverages, and to limit portion sizes is recommended. Elimination of industrially produced trans fats. Facilitating an integrated and coherent policy and activities of the local governments, NGOs, food industry, schools, to promote a healthy diet and to prevent obesity. Legislation restricting marketing aimed at children of foods that are high in fats, sugar and/or salt, less healthy options, junk foods, drinks with alcohol and non-alcoholic beverages rich in sugar (e.g. on TV, internet, social media). |
| Labelling and Information | Mandatory and harmonized simplified front of pack nutrition labeling. |
| Economic Incentives | Pricing and subsidy strategies to promote healthier food and beverage choices. Taxes on foods and beverages rich in sugar and saturated fat, and on alcoholic drinks. |
| Schools | At all schools, a comprehensive policy is recommended to promote a healthy diet. Availability of fresh drinking water and healthy foods in schools and in vending machines. |
| Workplaces | At all companies, a coherent and comprehensive health policy and nutritional education are recommended to stimulate the health awareness of employees. |
Drs. Gupta and Wood define a cardiovascular disease risk factor as any attribute, characteristic, or exposure of an individual or group that increases the likelihood of developing disease. They point out that causality of risk factors is a matter of judgement and is based on the totality of experimental and observational evidence. The key strategy for risk factor control is primordial prevention.
Political Determinants of Health
Gupta and Wood discuss how politics influence social change and highlight the success of Scandinavian health-in-all policies approach that has led to the low burden of ischemic heart disease in these countries. This is in contrast to the dramatic rise in ischemic heart disease seen in Russia following the fall of the Soviet Union, when sociopolitical turmoil prevailed. This period was marked by increased unemployment, poverty, and socioeconomic stress. In general, democratic industrialization of countries has been associated with improved living conditions, employment, and income.
Primordial Prevention in the 2016 ESC Guidelines
The ESC guidelines emphasize the role that local and national authorities play in altering the context in which individuals make healthy decisions. The guidelines specifically endorse the Geoffrey Rose paradigm that "small shifts in the risk of disease (or risk factor) across a whole population consistently lead to greater reductions in disease burden than a large shift in high-risk individuals only."4
The ESC guidelines address population-level interventions in the areas of diet and nutrition, physical activity, smoking, alcohol, and fostering a healthy environment. They give specific recommendations to both government and public health agencies as well as NGOs (nongovernmental organization that addresses a social or political issue) in the form of restrictions and mandates, media and education, labelling and information, economic incentives, schools, workplaces, and community settings (Table 1). They advocate a call to action for authorities to create social environments that provide healthier defaults for individuals. Similarly, the 2019 ACC/AHA prevention guidelines also discuss these concepts in detail; for instance, the sections on diet and physical activity make specific recommendations for the entire population.
Diet as an Example
Gupta and Wood discuss in detail the current evidence behind the linear relationship between food patterns and cardiovascular disease. Both the 2016 ESC Guidelines and the 2019 AHA/ACC Guidelines specifically address diet on an individual and population level, but the ESC guidelines go one step further to advocate for the need for national and local strategies as well.
These strategies would aim to help populations through the concepts of 'nudging' (to push mildly) and changing the 'default' (make healthy decisions the easy ones). On a policy level these take the form of structural measures such as product reformulation, limitations on marketing and taxes on unhealthy foods, subsidizing the costs of healthier foods, and consumer-friendly nutrition labelling.
Common to both the ESC and ACC/AHA guidelines is an emphasis on the increased intake of vegetables, fruits, legumes, nuts, whole grains, and fish. Individuals should minimize their consumption of red meat, processed meats, trans fats, refined carbohydrates, and sugar sweetened beverages. Lowering sodium intake is also very effective for controlling blood pressure.5
Primary Prevention Targets and ACC/AHA Guidelines
Gupta and Wood spend considerable time dedicated to what remains central to both the ESC and AHA/ACC guidelines — namely the aggressive evaluation, risk stratification, and modification of risk factors that lead to cardiovascular disease both in individuals and populations. Recommendations in this regard vary little (Table 2) as they pertain to cholesterol, glucose control, obesity, physical activity and exercise, consumption of healthy foods, elimination of unhealthy foods, and smoking and alcohol cessation.
Table 2
| 2016 ESC Guidelines on Primary Prevention of CVD | 2019 ACC/AHA Guidelines on Primary Prevention of CVD | |
| Risk Score | Systematic Coronary Risk Evaluation (SCORE) system: based on large, representative European cohort datasets. Calculates 10-year risk of cardiovascular mortality. | Atherosclerotic Cardiovascular Disease (ASCVD) risk score: uses the pooled cohort equation. Calculates 10-year risk of major cardiovascular event: MI, stroke, cardiac arrest. Approximately three-fold higher than the corresponding SCORE risk score. |
| Smoking and Tobacco Use | No exposure to tobacco in any form and to avoid passive smoking. | All adults should be assessed at every visit for tobacco use and their tobacco use status recorded to facilitate tobacco cessation; to achieve tobacco abstinence, all adults who use tobacco should be firmly advised to quit; in tobacco users, a combination of behavioral interventions plus pharmacotherapy is recommended to maximize quitting, and tobacco abstinence is strongly advised. |
| Healthy Diet | A healthy diet is recommended as a cornerstone of cardiovascular prevention, with a focus on wholegrain products, vegetables, fruit, and oily fish; 30 g unsalted nuts, >200 g fruits, and >200 g vegetables are recommended per day |
A diet emphasizing intake of vegetables, fruits, legumes, nuts, whole grains, and fish is recommended. |
| Dietary Fats | Diet should be low in saturated fat; saturated fatty acids should account for <10% of total energy intake, through replacement with polyunsaturated fats; trans-unsaturated fatty acids should be avoided, with preferably no intake from processed food and <1% of total energy intake from natural origins | Replacement of saturated fat with monounsaturated and polyunsaturated fats is beneficial and trans fats should be avoided. |
| Dietary Sodium | <2000 mg / day | <1500 mg / day |
| Physical Activity | At least 150 min per week of moderate aerobic physical activity (30 min for 5 days per week) or 75 min a week of vigorous aerobic activity (15 min for 5 days per week) or a combination thereof; for additional benefit in healthy adults, a gradual increase in activity to 300 min a week of moderate intensity or 150 min a week of vigorous intensity, or an equivalent combination thereof; this is recommended in all low-risk individuals without any assessment |
Adults should be routinely counselled in health-care visits to optimize a physically active lifestyle; adults should engage in ≥150 min per week of accumulated moderate-intensity or ≥75 min per week of vigorous-intensity aerobic physical activity (or an equivalent combination of moderate and vigorous activity). |
| Obesity | It is recommended that individuals with healthy bodyweight maintain it; and that people who are overweight or obese achieve a healthy bodyweight. | In individuals who are overweight or obese, weight loss is recommended. Interventions, including calorie restriction are recommended for achieving and maintaining weight loss. BMI is recommended annually or more frequently, and it is reasonable to measure waist circumference. |
| Hypertension | Hypertension is defined by office blood pressure of ≥140/90 mm Hg, ambulatory blood pressure of ≥130/80 mm Hg, or home blood pressure of ≥135/85 mm Hg; important to screen every individual for hypertension (opportunistic screening) and diagnosis confirmed using out-of-office blood pressure measurement; blood pressure control targets of <130/80 mm Hg for hypertensive patients with co-existing CAD, CKD, diabetes, and stroke.9 | Defined by average blood pressure of ≥130/80 mm Hg, with blood pressure measured at multiple occasions; in adults with hypertension, including those requiring antihypertensive medications, non-pharmacological interventions are recommended to reduce blood pressure. In adults with an estimated 10-year risk of ≥10% and average systolic blood pressure of ≥130 mm Hg or average diastolic blood pressure of ≥80 mm Hg, use of blood pressure-lowering medications is recommended; in adults with confirmed hypertension and a 10-year event risk of ≥10%, CKD, or DM, a target of <130/80 mm Hg is recommended; in adults with an estimated 10-year atherosclerotic cardiovascular disease risk of <10% and SBP of ≥140 mm Hg or DBP of ≥90 mm Hg, initiation and use of blood pressure-lowering medication is recommended. |
| LDL Cholesterol | In very-high-risk patients the target is <1∙8 mmol/L, or a reduction of at least 50% if the baseline is between 1∙8 mmol/L and 3∙5 mmol/L; in high-risk patients the target is <2∙6 mmol/L or a reduction of at least 50% if the baseline is between 2∙6 mmol/L and 5∙1 mmol/L; in low-to-moderate-risk patients the target is <3∙0 mmol/L | In intermediate-risk (≥7∙5% to <20% 10-year risk) patients, statin therapy reduces risk of ischemic heart disease, and in the context of a risk discussion, a moderate-intensity statin should be recommended; in intermediate-risk patients, LDL-C concentrations should be reduced by ≥30%; for optimal risk reduction, especially in patients at high risk (≥20% 10-year risk), concentrations should be reduced by ≥50%; in adults aged 40–75 years with diabetes, regardless of estimated 10-year risk, moderate-intensity statin therapy is indicated; in patients aged 20–75 years with an LDL concentration of 190 mg/dL (≥4∙9 mmol/L) or higher, maximally tolerated statin therapy is recommended; in adults with diabetes who have multiple risk factors, it is reasonable to prescribe high-intensity statin therapy with the aim to reduce LDL concentrations by ≥50% |
| Diabetes | HbA1c <7%. Lifestyle changes including smoking cessation, healthy diet, aerobic physical activity, and strength training. |
A tailored nutrition plan focusing on a heart-healthy dietary pattern is recommended; adults should do at least 150 min per week of moderate-intensity physical activity or 75 min of vigorous-intensity physical activity; reasonable to initiate metformin as first-line therapy along with lifestyle therapies to improve glycemic control and reduce risk |
| Aspirin | Not recommended. | Should not be administered routinely. |
The US guidelines classify hypertension as ≥130/80 mmHg, while the European guidelines define hypertension as an office blood pressure average of ≥140/90 mmHg. The European guidelines do target values of <130/80 mmHg in most high-risk patients. Emphasis on the abovementioned healthy behaviors leads to reduction of conditions such as diabetes, hypertension, and hyperlipidemia.
Discussion
Drs. Gupta and Wood's emphasis on primordial prevention sharpens the focus on the role that local and federal governments play in primary prevention. Their manuscript highlights the importance of collective willpower in developing policy and legislation which curb behaviors that contribute heavily to the burden of ischemic heart disease. Table 3 highlights the distinction between primordial prevention and primary prevention noted by the authors. The left column of Table 3 lists the social and political determinants of health that shape public policy and the right column lists the individual and population-based risk factors that are common to both the ESC and AHA/ACC guidelines.
Table 3
| Primordial Prevention Targets | Primary Prevention Targets |
| Urban and Rural Infrastructure Illiteracy Maternal and Child Health Transportation Social Support Poverty and Wages Facilities for physical activity Health-care financing Universal Health Care Food, agriculture Work environment, unemployment, job stress |
Elimination of Unhealthy foods in the diet Promotion of Health foods in the diet Smoking and Smokeless Tobacco cessation Alcohol cessation Blood Pressure control Cholesterol control Family History identification Physical Activity Curbing high salt intake Blood glucose control Reduction in Psychosocial stress |
While promotion of the concepts of both a healthy diet and environments that are safe for exercise are discussed above, there are innumerable other examples of ways to curb ischemic heart disease through policy strategies that foster promotion of healthy environments in the community, at schools, and in work-places. It is additionally important to promote health literacy education in both medical schools and in the general population, as well as continued focus on the reduction of unhealthy behaviors such as smoking and consumption of refined carbohydrates, trans fats, and sugary beverages.
Primordial prevention is discussed in the main conclusions of the 2019 ACC/AHA primary prevention guidelines, stating "it should be noted that most ASCVD events are avoidable through prevention of risk factor development, i.e. primordial prevention, in addition to tight control of traditional cardiovascular risk factors" but the role of governmental policies to promote health is dealt with more fully in our recent AHA/ACC documents.2,6-8 The best takeaway from the Gupta and Wood article may be their concluding remark: "to prevent is better than to cure, and to wait until people develop ischemic heart disease is too late for too many."
References
- Gupta R, Wood DA. Primary prevention of ischemic heart disease: populations, individuals, and health professionals. Lancet 2019;394:685-96.
- Weintraub WS, Daniels SR, Burke LE, et al. Value of primordial and primary prevention for cardiovascular disease: a policy statement from the American Heart Association. Circulation 2011;124:967-90.
- Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019;140:e596-e646.
- Piepoli, MF, Hoes AW, Agewall S, et al. 2016 European guidelines on cardiovascular disease prevention in clinical practice. Atherosclerosis 2016;252:207-74.
- Sacks FM, Lichtenstein AH, Wu JHY, et al. Dietary fats and cardiovascular disease: a presidential advisory from the American Heart Association. Circulation 2017;136:e1-23.
- Havranek EP, Mujahid MS, Barr DA, et al. Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation 2015;132:873-98.
- Johnson RK, Appel LF, Brands M, et al. Dietary sugars intake and cardiovascular health: a scientific statement from the American Heart Association. Circulation 2009;120:1011-20.
- Riegel B, Moser DK, Buck HG, et al. Self-care for the prevention and management of cardiovascular disease and stroke: a scientific statement for healthcare professionals from the American Heart Association. J Am Heart Assoc 2017;6:e006997.
- Yang E, Sharma G, Ram V. American and European hypertension guidelines: finding common ground. Am J Cardiol 2019;123:1378-82.
Keywords: Dyslipidemias, Blood Pressure, Cardiovascular Diseases, Cholesterol, Coronary Artery Disease, Diabetes Mellitus, Diet, Education, Medical, Exercise, Food Labeling, Fabaceae, Goals, Health Literacy, Hyperlipidemias, Hypertension, Myocardial Ischemia, Obesity, Primary Prevention, Poverty, Public Health, Public Policy, Risk Factors, Smoking, Social Change, Sweetening Agents, Tobacco, Vascular Diseases, Sodium
< Back to Listings