Comparison of the ACC/AHA and ESC/ESH Hypertension Guidelines
Introduction
Hypertension is the leading cause of death, premature morbidity, and disability-adjusted life years worldwide and a primary risk factor for coronary artery disease (CAD), cerebrovascular disease (CeVD), heart failure (HF), chronic kidney disease (CKD), and dementia.1,2
Given the importance of hypertension management to reduce cardiovascular (CV) morbidity and mortality, clinical guidelines have been established to provide a framework to guide clinicians in the diagnosis and treatment of this condition. While professional medical societies have developed many hypertension guidelines, two well-established documents from North America and Europe are the 2017 American College of Cardiology (ACC)/American Heart Association (AHA) and 2018 European Society of Cardiology (ESC)/European Society of Hypertension (ESH) guidelines.3,4 Although there are key differences between these guidelines, it is important to acknowledge that there is also much overlap. In this review, we will discuss the common features and explore some of the major differences between the guidelines.
Principal Areas of Agreement Between American and European Guidelines
- Emphasis on accuracy of BP measurements: Both guidelines recommend office blood pressure (BP) measurement on repeated visits and ambulatory blood pressure monitoring (ABPM) or home blood pressure monitoring (HBPM) to confirm the diagnosis of hypertension (Class I). ABPM uses a device worn on the patient's arm to record BP at 15- or 30-minute intervals for 24 to 48 hours during routine daily activities and sleep. HBPM is a self-monitoring tool where patients use commercially available instruments to measure and record their BPs. There is consensus that ABPM and HBPM provide a greater number of BP measurements than conventional office BPs and reflect conditions that are more representative of daily life. Additionally, both are useful tools for the diagnosis of "white coat" and masked hypertension. For adults who present with elevated office BPs but normal readings at home, ABPM or HBPM should be used to confirm diagnosis of white coat hypertension. Masked hypertension refers to untreated patients with normal office BPs but signs of end-organ damage. It is associated with an increased risk of CV morbidity and mortality and should be diagnosed using ABPM or HBPM.
- Cardiovascular-risk calculator to determine BP treatment thresholds: ESC guidelines utilize the Systematic Coronary Risk Evaluation (SCORE) system to estimate CV risk for patients with hypertension at the time of initial diagnosis prior to initiation of pharmacotherapy or whenever changes occur to BP readings.4 Since 2003, the European CV prevention guidelines have recommended the SCORE risk estimate because it is based on large, representative European cohorts and estimates the 10-year risk of a first fatal atherosclerotic cardiovascular disease event in relation to age, sex, smoking habits, total cholesterol level, and systolic BP (SBP). It also allows for country-specific risk calibration in European countries based on CV disease risk levels and has been externally validated. The ACC/AHA guidelines recommend use of the Atherosclerotic Cardiovascular Disease Risk (ASCVD) calculator using the Pooled Cohort Equation (PEC) for determination of BP targets. Both guidelines recognize that treatment decisions based on aligning thresholds with CV risk offer a more rational and evidence-based approach. If the CV risk is low, both recommend initial emphasis on lifestyle modifications prior to initiation of pharmacotherapy. While the Europeans identify hyperuricemia and elevated heart rate as CV disease risk factors, American guidelines do not recognize them due to limited evidence that treatment improves clinical outcomes.
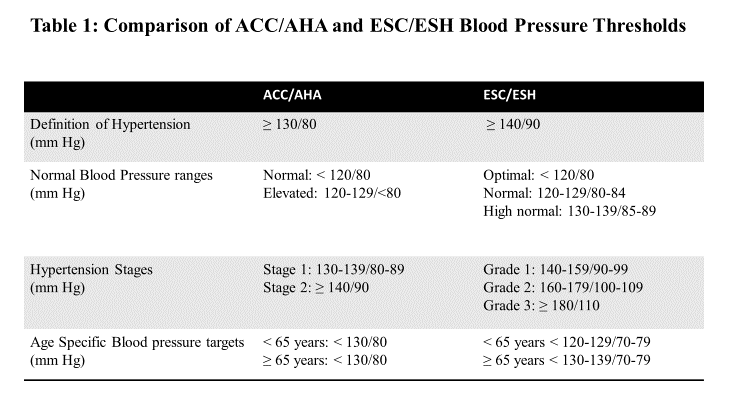
- BP treatment targets: When comparing the guidelines, the definition of normal (as used in the ACC/AHA guidelines) or optimal BP (as used in the ESC/ESH guidelines) is the same for systolic BP (<120 mm Hg) and diastolic BP (DBP) (<80 mm Hg) (Table 1).
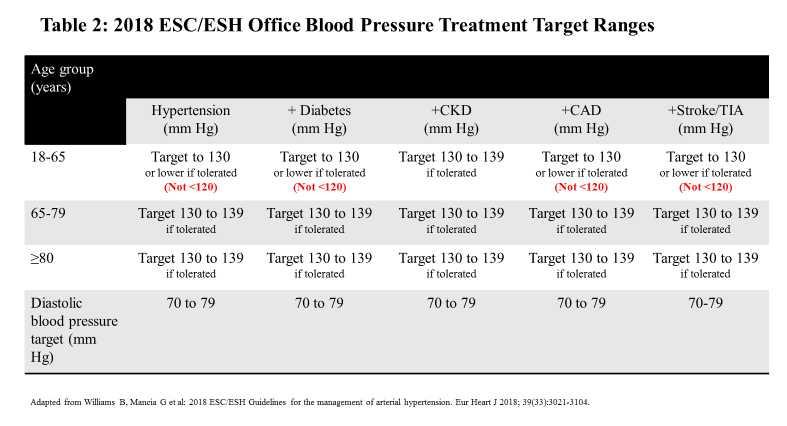
The ACC/AHA guidelines replace "prehypertension" with "elevated blood pressure" for BP levels 120-129/80-89 mm Hg while the ESC/ESH defines this category as "normal blood pressure". The American cut-off for the definition of hypertension has been lowered to ≥130/80 mm Hg with BP range 130-139/80-89 mm Hg now classified as stage 1 hypertension.3 While lowering the BP threshold levels for diagnosis and treatment of hypertension has created controversy in the American public and among other major medical societies, there is strong evidence for increased CV risk for systolic BP levels between 130-139 mm Hg and diastolic BP levels between 80-89 mm Hg.3 Moreover, as clinical trial data have demonstrated additional benefits of aggressive BP lowering to <130 mm Hg, the BP target recommended in the 2017 ACC/AHA guidelines has been revised to <130/80 mm Hg (<130 mm Hg systolic BP only in ambulatory, community living older adults ≥65 years). In contrast, the 2018 ESC/ESH guidelines do not lower the hypertension threshold definition (>140/90 mm Hg) but they do acknowledge that 130-139/80-89 mm Hg is high normal BP. A deeper dive into the European recommendations reveals similar BP treatment targets (<130/80 mm Hg) for hypertensive patients with co-existing CAD, CKD, diabetes, and CeVD (Table 2).
- Lifestyle modification recommendations: Both guidelines recommend lifestyle modifications as primary interventions to prevent and treat hypertension. The ACC/AHA and ESC/ESH hypertension guidelines stress the importance of weight optimization, heart healthy diet (e.g. DASH), sodium restriction, physical activity with a structured exercise program, abstinence from or moderation of alcohol consumption and smoking cessation as strategies to optimize BP (Class 1, evidence level A).3,4 Both stress that effective lifestyle changes may be sufficient to delay or prevent the need for drug therapy in patients with stage 1 hypertension (ACC/AHA guidelines) or high normal BP (ESC/ESH guidelines). For patients with stage 2/grade 1 hypertension, pharmacotherapy should be initiated without delay, but lifestyle and behavioral interventions should be concurrently emphasized. Weight reduction is recommended to target a healthy BMI (19-25 kg/m2) and to avoid obesity (BMI >30 kg/m2). Hypertensive patients are advised to eat a balanced diet containing vegetables, legumes, fresh fruits, low-fat dairy products, whole grains, fish and poultry, and unsaturated fatty acids (especially olive oil) while minimizing consumption of red meat and saturated fat. Moderate intensity exercise is encouraged, especially dynamic aerobic exercises such as walking, jogging, cycling, or swimming for 30 minutes daily at least 5 times a week.
- Pharmacotherapy for BP management: American and European hypertension guidelines recommend initial BP treatment based on four major classes of pharmacotherapies including ACE inhibitors (ACEi), angiotensin receptor blockers (ARBs), calcium channel blockers (CCBs), and thiazide/thiazide‐like diuretics. Beta‐blockers are recommended in select patients, such as those with heart failure with reduced ejection fraction (HF-rEF) or myocardial infarction. Combination therapy is recommended by both guidelines for stage 2 hypertension, average SBP/DBP >20/10 mm Hg above BP target. For hypertensive blacks, the ESC/ESH guidelines also give a Class I recommendation to the use of combination drug therapy, preferably with a diuretic or CCB with a renin-angiotensin system (RAS) blocker.
Primary Differences Between American and European Guidelines
- Classification of BP status and definition of hypertension: Despite their similarities, the two guidelines take a different position in several key areas. The most apparent is in the classification of hypertension. In the European guidelines, hypertension is defined as a BP ≥140/90 mm Hg (Table 1) while the Americans choose a lower threshold of BP ≥130/80 mm Hg. American guidelines classify Stage 1 hypertension as SBP ≥130‐139 mm Hg or DBP ≥80‐89 mm Hg while the Europeans define this as high normal BP (130-139/85-89 mm Hg). ACC/AHA defines Stage 2 hypertension as BP ≥140/90 mm Hg while the Europeans continue to classify this as Stage 1 (140-159/90-99 mm Hg) (Table 1).
- BP targets in older adults (age ≥65): Unlike the 2017 ACC/AHA recommendation for similar BP targets across all age groups (except age ≥65 years where the ACC/AHA guidelines recommend target of SBP <130 mmHg), the ESC/ESH guidelines have taken a more restrained stance on BP thresholds for older adults. The 2013 ESC/ESH guidelines endorsed a BP target of <150/90 mm Hg for adults ≥65 years old. The 2018 committee recognized the importance of more aggressive BP control for all populations, including older cohorts, and supported lowering the threshold to <140/80 mm Hg for this group. Consistent with the ACC/AHA recommendations, there is acknowledgment of the difference between biological versus chronological age and the importance of assessing other factors, such as frailty and tolerability of treatment, to guide BP management in this population. The ESC/ESH guideline authors point out that while the SPRINT trial included a high proportion of patients over >75 years who had varying degrees of frailty, they were still independently living.5 The HYVET trial targeted individuals >80 years and similarly included active, older adults.6 The cautious approach taken by the Europeans may reflect some of the concerns raised by those who felt that the aggressive ACC/AHA targets were not sufficiently supported by meta-analyses of the randomized controlled trials.7
- Drug treatment strategies: There is consensus on pharmacologic hypertension management between American and European guidelines. Antihypertensive therapy recommendations for specific disease states including CAD, CKD, and HF-rEF are nearly identical. The Europeans still include beta-blockers among the first line options for hypertension management while American guidelines specify their primary use only for patients with ischemic heart disease or HF-rEF. While ACC/AHA recommends a single pill combination (SPC) for Stage 2 hypertension, the ESC/ESH encourages SPCs for all grades of hypertension given greater ease of use and potential for improved patient adherence.
- BP targets in specific populations: With few exceptions, the ACC/AHA guidelines have a uniform BP treatment target of <130/80 mm Hg. The European guidelines provide some rationalization for their BP threshold recommendations for specific populations, including different ethnicities, diabetics, pregnant women, and CKD patients. Given the heterogeneity of ethnic groups in Europe, blacks in particular, and the lack of a sufficient registry to accurately assess CV outcomes in some minority groups, the European guidelines calculate CV risk in blacks utilizing American cohorts. They do acknowledge this as a major deficiency in their guidelines and an opportunity for research. A unique aspect of the European SCORE risk estimate is the use of correction factors to reflect CV risk differences among 1st generation immigrants to Europe. American guidelines do recognize differences in CV risk among Asian and Hispanic sub-groups, but no multiplier exists to refine the risk calculator in these populations. Of note, the European guidelines have identified hypertensive patients of South Asian origin as the highest risk group. This group was also recently recognized as a risk enhancer in the updated 2018 ACC/AHA blood cholesterol guidelines though was not part of the 2017 ACC/AHA hypertension guidelines.8 For diabetic patients, the Europeans recommend a BP threshold of >140/90 mm Hg for initiation of anti-hypertensive therapy while treatment is recommended for BP ≥130/80 mm Hg in the American guideline.9 However, both endorse a target BP <130/80 mm Hg. While the Europeans recommend combination antihypertensive therapy with a RAS blocker + CCB or thiazide diuretic, no specific drug combinations are proposed in the American guidelines. For patients with CKD, the European guidelines contend that there is insufficient evidence to support treatment targets lower than 130/80 mm Hg. For hypertension and pregnancy, the Europeans provide clear definitions and classifications as well as comprehensive recommendations for laboratory testing, risk stratification, and pharmacotherapy. For example, in the ESC/ESH guidelines, hypertension in pregnancy is defined as mild (140-159/90-109 mm Hg) or severe (≥160/110 mm Hg).
Conclusion
After careful review of the two guidelines, we find more agreement with the Europeans than major differences. Both strongly recommend lower BP targets for high-risk patients and place a similar emphasis on proper BP measurement and technique, laboratory and diagnostic testing, lifestyle and behavioral changes, and pharmacological management. Even though the Europeans have not changed the hypertension definition thresholds, they acknowledge that lower BP (e.g. <130/80 mm Hg) reduces CV morbidity and mortality. While the aggressive American BP goals may be difficult to achieve, the medical community must make a concerted effort to embrace these recommendations.10,11
References
- Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2224-60.
- Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomized trials in the context of expectations from prospective epidemiological studies. BMJ 2009;338:b1665.
- Whelton PK, Carey RM, Aronow WS, et al. 2017ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018;71:1269-1324.
- Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J 2018;39:3021-3104.
- Williamson JD, Supiano MA, Applegate WB, et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA 2016;315:2673–82.
- Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med 2008;358:1887-98.
- Qaseem A, Wilt TJ, Rich R, et al. Pharmacologic treatment of hypertension in adults aged 60 Years or older to higher versus lower blood pressure targets: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med 2017;166:430-37.
- Grundy SM, Stone NJ, Bailey AL; et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019;73:3168-3209.
- American Diabetes Association. Cardiovascular disease and risk management: standards of medical care in diabetes-2018. Diabetes Care 2018;41:S86–S104.
- Ram CVS. Latest guidelines for hypertension: adopt and adapt. J Am Soc Hypertens 2018;12:67-68.
- Yang E, Sharma G, Ram V. American and European hypertension guidelines: finding common ground. Am J Cardiol 2019;123:1378-82.
Clinical Topics: Cardiovascular Care Team, Diabetes and Cardiometabolic Disease, Dyslipidemia, Heart Failure and Cardiomyopathies, Prevention, Vascular Medicine, Atherosclerotic Disease (CAD/PAD), Lipid Metabolism, Nonstatins, Acute Heart Failure, Exercise, Hypertension, Smoking, Sleep Apnea
Keywords: Primary Prevention, Secondary Prevention, Adrenergic beta-Antagonists, American Heart Association, Angiotensin-Converting Enzyme Inhibitors, Blood Pressure, Blood Pressure Monitoring, Ambulatory, Body Mass Index, Angiotensin Receptor Antagonists, Calcium Channel Blockers, Cardiovascular Diseases, Antihypertensive Agents, Cerebrovascular Disorders, Cholesterol, Cohort Studies, Coronary Artery Disease, Dementia, Diabetes Mellitus, Cause of Death, Diuretics, Drug Therapy, Combination, Drug Combinations, Ethnic Groups, Fabaceae, Fatty Acids, Unsaturated, Exercise Therapy, Goals, Heart Failure, Hispanic Americans, Heart Rate, Hypertension, Hyperuricemia, Life Style, Masked Hypertension, Minority Groups, Myocardial Infarction, Patient Compliance, Obesity, Pregnancy, Prehypertension, Quality-Adjusted Life Years, Rationalization, Registries, Renal Insufficiency, Chronic, Renin-Angiotensin System, Risk Factors, Smoking, Smoking Cessation, Societies, Medical, Sodium, Sodium Chloride Symporter Inhibitors, Stroke Volume, Thiazides, Weight Loss, White Coat Hypertension
< Back to Listings