PCI vs. CABG in Patients With Three-Vessel or LM CAD: Who Finally Won the Battle of the Titans?
The SYNTAXES study (Synergy Between Percutaneous Coronary Intervention With TAXUS and Cardiac Surgery Extended Survival) is the 10-year follow-up of the original SYNTAX trial. It is the study with the longest follow-up comparing coronary artery bypass grafting (CABG) and percutaneous coronary intervention (PCI) with drug-eluting stents (DES) in the treatment of three-vessel or left main (LM) coronary artery disease (CAD).
The SYNTAX trial was initially published in 2009,1 and it remains the landmark study for decision-making and risk stratification of complex CAD. Both the initial trial with 1-year follow-up and the numerous sub-studies within the 5-year follow-up have been published with a primary outcome of a composite of major adverse cardiac and cerebrovascular events.2-4 In all of these studies, CABG demonstrated fewer major adverse cardiac and cerebrovascular events compared with PCI. Arguably most importantly, the SYNTAX study introduced the heart team concept and the SYNTAX score to allow assimilation and grading of the patients' coronary disease burden.
In 2018, 5-year data from the SYNTAX trial and other similar randomised studies (11 randomised trials involving 11,518 patients) comparing PCI with CABG for complex CAD were assembled and meta-analyzed.5 All-cause mortality was significantly higher with PCI compared with CABG. Due to the large number of individual data, subgroup analysis was feasible. It showed that in non-diabetic patients with multivessel disease and low (≤22) SYNTAX score, PCI was as safe and effective as CABG. Similarly, patients with non-complex LM disease had similar survival with PCI and CABG. In diabetic patients, a trend for better outcome with CABG compared with PCI was observed as the SYNTAX score increased. Conclusions from this meta-analysis were adopted from the European Society of Cardiology Revascularization Guidelines, and recommendations were made accordingly.6
These changes in recommendations led to a debate between cardiologists and cardiac surgeons7-9 that was highlighted in the accompanying editorial of the SYNTAXES trial.10 The main reason for debate was the lack of long-term follow-up in comparative PCI/CABG trials. Publication of the SYNTAXES trial attempts to fill this gap, providing long-term follow-up data on mortality of patients in the SYNTAX trial with a median follow-up duration of 11.2 years.
The primary outcome of SYNTAXES was all-cause death at 10 years in patients previously assigned to PCI with DES versus CABG. The secondary outcome was all-cause death at maximum available follow-up. According to the authors, the primary outcome in SYNTAXES occurred in 27% of the PCI patients and in 24% of the CABG patients (hazard ratio [HR] 1.17; 95% confidence interval [CI], 0.97-1.41; p = 0.092), concluding that there is no significant difference between the 2 treatments.11 Furthermore, these results were consistent across the 2 different lustrums (0-5 and 5-10 years). However, superiority of CABG compared with PCI was observed for the secondary endpoint, with PCI increasing the risk of death by 18% compared with CABG.
A more detailed investigation showed that patients with three-vessel disease had a survival advantage with CABG versus PCI at 10 years (21% vs. 28% died, respectively; HR 1.41; 95% CI, 1.10-1.80; p = 0.006). In three-vessel disease, high SYNTAX score (>33) was the principal differentiator. Contrary to previous reports in SYNTAX or similar studies in diabetics,12 diabetes was not a differentiator of prognosis. No difference between the 2 groups was evident in patients with LM disease (26% vs. 28%, respectively; HR 0.90; 95% CI, 0.68-1.20; p = 0.47).
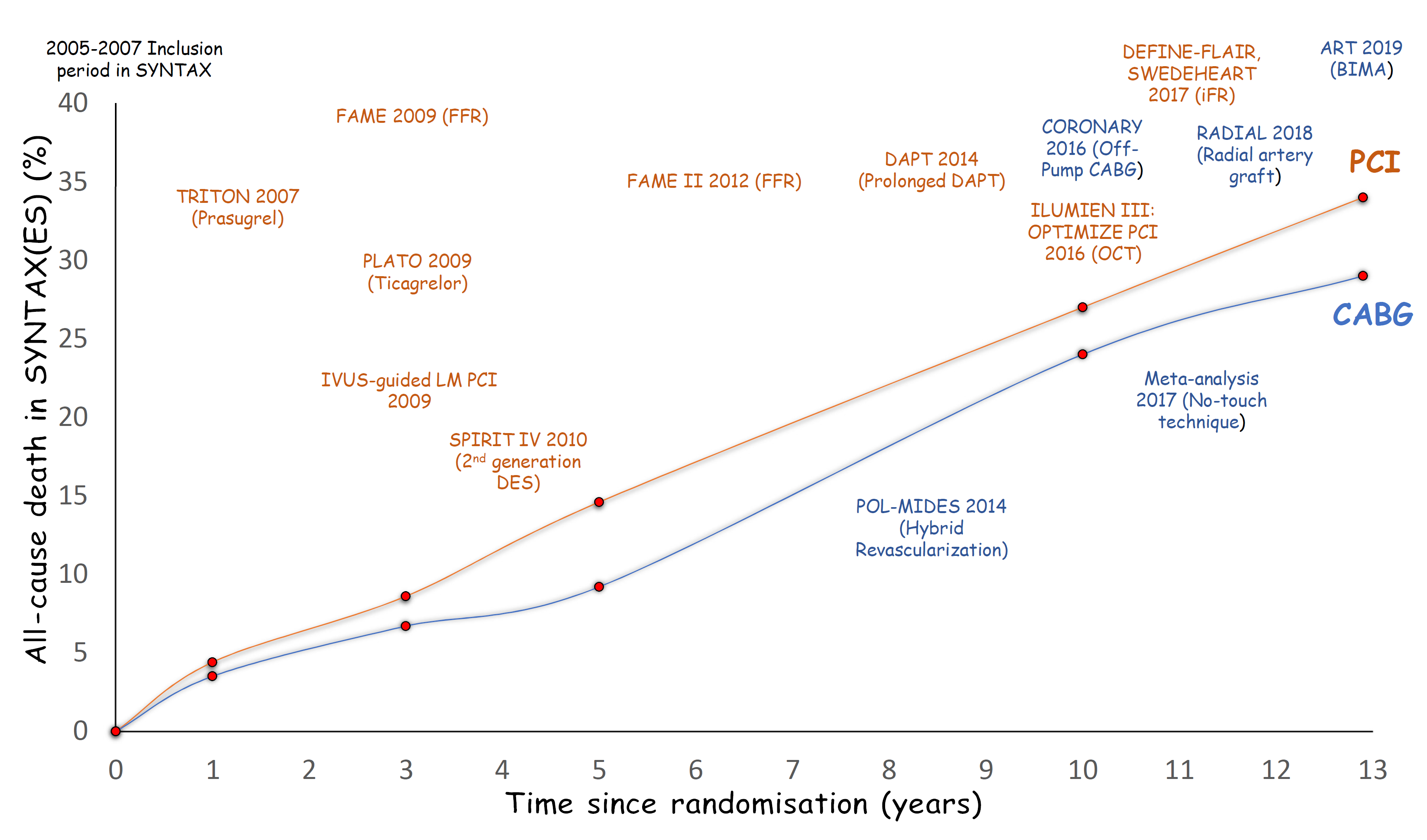
SYNTAXES is the longest study to date to follow patients treated with first-generation DES and compare outcomes with CABG. Moreover, despite the long duration of follow-up, 94% of the patients had a complete follow-up. However, the results of the study have to be considered and applied to practice. Disappointingly, the primary endpoint of major adverse cardiac and cerebrovascular events used in previous SYNTAX trial reports was not available due to the design of this study. Thus, any speculation on the exact cause of the deaths reported within SYNTAXES is not possible.13 Indeed, due to the formal end of the original SYNTAX trial, any data after the 5 years of follow-up on contemporary medical treatment, invasive treatment, or possible cross-over are lacking. Additionally, these data do not reflect contemporary practice, including use of first-generation DES that are known to have higher repeat revascularisation and stent thrombosis rates,14 incomplete revascularisation in many patients, no intracoronary imaging, and a lack of physiological guidance for strategy (Figure 1). Many of these limitations have been addressed in the SYNTAX II trial.15 In this study, patients were selected using an evolution of the SYNTAX score—the SYNTAX II score—that combined the angiographic score with some clinical characteristics. Revascularisation was based on pressure wire assessment, a third-generation stent was used, and the result was analysed and optimized using intravascular ultrasound. Better complete revascularisation rates were achieved using contemporary techniques for chronic occlusions, and, finally, improved, more potent antithrombotic agents were available. These newer dual antiplatelet therapy (DAPT) regimes have been shown to improve results after PCI in extensive CAD.16 Encouragingly, initial data from SYNTAX II shows significantly better results than the PCI arm in SYNTAX and data comparable to the surgical arm at 2-year follow-up.17
Figure 1
In our opinion, results of the SYNTAXES trial provide useful information on outcomes after revascularization in complex CAD. CABG provided better (more complete) revascularisation then and, unsurprisingly, better long-term survival compared with PCI. In 2019, we must prioritise complete revascularisation and abolition of ischaemia, and this requires more than an angiographically based procedural algorithm. Use of comparative risk score informs the heart team decisions, and availability of contemporary guideline-directed PCI techniques will facilitate better outcomes. Notably, mortality rates are suboptimal in SYNTAXES even in the CABG patients, and improved drug therapy to modify prognosis is required, especially in patients with diabetes.
References
- Serruys PW, Morice MC, Kappetein AP, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med 2009;360:961-72.
- Kappetein AP, Feldman TE, Mack MJ, et al. Comparison of coronary bypass surgery with drug-eluting stenting for the treatment of left main and/or three-vessel disease: 3-year follow-up of the SYNTAX trial. Eur Heart J 2011;32:2125-34.
- Mohr FW, Morice MC, Kappetein AP, et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet 2013;381:629-38.
- Head SJ, Davierwala PM, Serruys PW, et al. Coronary artery bypass grafting vs. percutaneous coronary intervention for patients with three-vessel disease: final five-year follow-up of the SYNTAX trial. Eur Heart J 2014;35:2821-30.
- Head SJ, Milojevic M, Daemen J, et al. Mortality after coronary artery bypass grafting versus percutaneous coronary intervention with stenting for coronary artery disease: a pooled analysis of individual patient data. Lancet 2018;391:939-48.
- Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J 2019;40:87-165.
- Collet C, Capodanno D, Onuma Y, et al. Left main coronary artery disease: pathophysiology, diagnosis, and treatment. Nat Rev Cardiol 2018;15:321-31.
- Doenst T, Haverich A, Serruys P, et al. PCI and CABG for Treating Stable Coronary Artery Disease: JACC Review Topic of the Week. J Am Coll Cardiol 2019;73:964-76.
- Farina P, Gaudino MFL, Taggart DP. The Eternal Debate With a Consistent Answer: CABG vs PCI. Semin Thorac Cardiovasc Surg 2019;Aug 20:[Epub ahead of print].
- Taggart DP, Pagano D. Expansion or contraction of stenting in coronary artery disease? Lancet 2019;394:1299-300.
- Thuijs DJFM, Kappetein AP, Serruys PW, et al. Percutaneous coronary intervention versus coronary artery bypass grafting in patients with three-vessel or left main coronary artery disease: 10-year follow-up of the multicentre randomised controlled SYNTAX trial. Lancet 2019;394:1325-34.
- Farkouh ME, Domanski M, Dangas GD, et al. Long-Term Survival Following Multivessel Revascularization in Patients With Diabetes: The FREEDOM Follow-On Study. J Am Coll Cardiol 2019;73:629-38.
- Milojevic M, Head SJ, Parasca CA, et al. Causes of Death Following PCI Versus CABG in Complex CAD: 5-Year Follow-Up of SYNTAX. J Am Coll Cardiol 2016;67:42-55.
- Stone GW, Rizvi A, Newman W, et al. Everolimus-eluting versus paclitaxel-eluting stents in coronary artery disease. N Engl J Med 2010;362:1663-74.
- Escaned J, Collet C, Ryan N, et al. Clinical outcomes of state-of-the-art percutaneous coronary revascularization in patients with de novo three vessel disease: 1-year results of the SYNTAX II study. Eur Heart J 2017;38:3124-34.
- Kotsia A, Brilakis ES, Held C, et al. Extent of coronary artery disease and outcomes after ticagrelor administration in patients with an acute coronary syndrome: Insights from the PLATelet inhibition and patient Outcomes (PLATO) trial. Am Heart J 2014;168:68-75.e2.
- Serruys PW, Kogame N, Katagiri Y, et al. Clinical outcomes of state-of-the-art percutaneous coronary revascularisation in patients with three-vessel disease: two-year follow-up of the SYNTAX II study. EuroIntervention 2019;15:e244-e252.
Clinical Topics: Cardiac Surgery, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Stable Ischemic Heart Disease, Atherosclerotic Disease (CAD/PAD), Aortic Surgery, Cardiac Surgery and SIHD, Interventions and Coronary Artery Disease, Interventions and Imaging, Angiography, Echocardiography/Ultrasound, Nuclear Imaging, Chronic Angina
Keywords: Coronary Artery Disease, Drug-Eluting Stents, Percutaneous Coronary Intervention, Platelet Aggregation Inhibitors, Fibrinolytic Agents, Taxus, Prospective Studies, Tomography, Optical Coherence, Mammary Arteries, Confidence Intervals, Constriction, Pathologic, Follow-Up Studies, Fractional Flow Reserve, Myocardial, Radial Artery, Coronary Artery Bypass, Heart Diseases, Diabetes Mellitus, Angiography, Coronary Angiography, Prognosis, Thrombosis, Treatment Outcome, Algorithms, Risk Assessment, Ultrasonography, Interventional, Evidence-Based Medicine, Angina, Stable
< Back to Listings