Key CVOTs with Semaglutide: SUSTAIN 6 and PIONEER 6
Semaglutide is a potent glucagon-like peptide 1(GLP-1) analogue with a high degree of homology to human GLP-1. Two formulations of semaglutide have been approved by the FDA; semaglutide for subcutaneous injection once-weekly (marketed as Ozempic®)1 and semaglutide for oral administration once-daily (marketed as Rybelsus®).2 Two large phase 3a pre-approval Cardiovascular Outcomes Trials (CVOTs), SUSTAIN 63 and PIONEER 6,4 investigated the effects of subcutaneous and oral semaglutide versus placebo on Major Adverse Cardiovascular Events (MACE) in patients with type 2 diabetes (T2D) and high cardiovascular (CV) risk. These trials were designed and conducted in accordance with the 2008 US Food and Drug Administration (FDA) guidance for evaluating CV safety in new glucose-lowering therapies.5 In both trials, at least 122 first MACE were required to rule out a hazard ratio of 1.8 (preapproval boundary for noninferiority assessment). The SUSTAIN 6 CVOT was designed with the additional requirement of minimum 104 weeks of treatment exposure for assessment of long-term efficacy and safety. Besides the difference that SUSTAIN 6 was both event-driven and duration-driven, and PIONEER 6 was purely event-driven, the design of PIONEER 6 resembled that of SUSTAIN 6. The adjudication process, conducted by an independent and blinded Events Adjudication Committee (EAC), and event definitions were similar across the CVOTs. The primary endpoint was time from randomization to first occurrence of an adjudicated 3-component composite MACE endpoint defined as CV death, non-fatal myocardial infarction (MI), or non-fatal stroke. In SUSTAIN 6, the hierarchical testing strategy included a test for noninferiority versus placebo as the first step; a test for superiority was not pre-specified.3 In PIONEER 6, the hierarchical testing strategy included a test for noninferiority as a first step, followed by test of superiority versus placebo.4 In SUSTAIN 6, two treatment doses were investigated (0.5 and 1 mg) whereas PIONEER 6 evaluated one treatment dose of 14 mg.
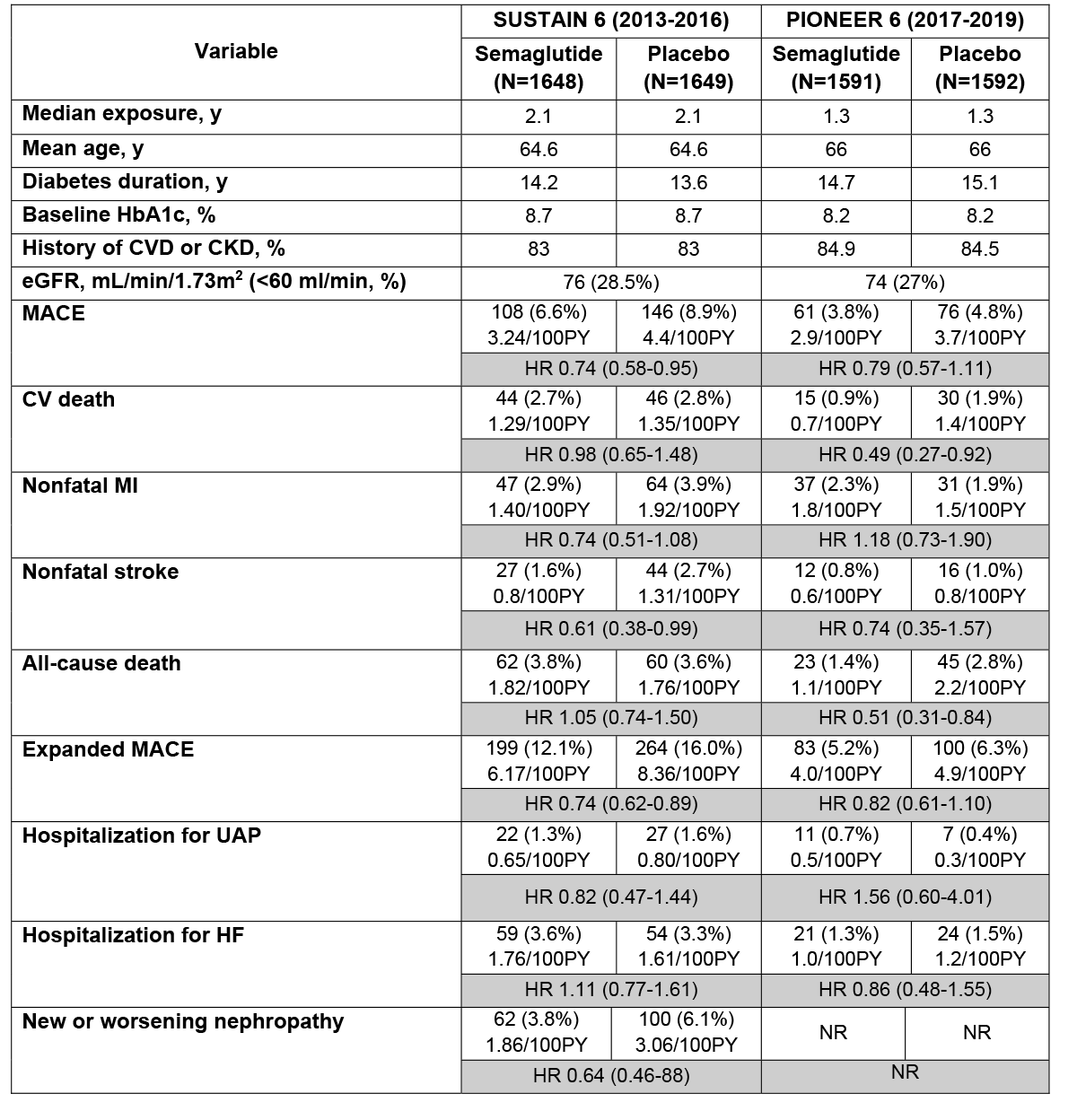
Both CVOTs employed an enrichment strategy to enroll patients with T2D at high CV risk. The majority of patients were enrolled based on established CVD and/or chronic kidney disease (CKD) (Table 1). A substantial proportion of patients was 65 years of age or above. Background therapy, including glucose-lowering treatments, was in accordance with the standards of care commonly used in the T2D population.
In both the CVOTs, trial completion rate was high (SUSTAIN 6: 97.6%; PIONEER 6: 99.7%) with vital status at end-of-trial known for 99.6% of patients in SUSTAIN 6 and 100% in PIONEER 6. The median duration of exposure was 21.6 months in SUSTAIN 6 and 15.9 months in PIONEER 6.
Key Results
The key CV outcome results are summarized in Table 1.
Table 1: Summary of Key Demographics and Results from CVOTs with Semaglutide
SUSTAIN-6
A total of 254 patients had an EAC-confirmed first MACE with fewer patients with events with semaglutide resulting in risk reduction of 26%. Similar risk reduction was observed with the 0.5 mg dose (HR 0.77, 95% CI 0.55,1.08) and 1 mg dose (HR 0.71, 95% CI 0.49, 1.02). The risk difference was driven by fewer non-fatal myocardial infarction and non-fatal stroke, whereas there was no difference in cardiovascular deaths. All-cause mortality was not reduced. The results of the expanded MACE were in line with the results for the primary MACE analysis. The HR point estimates for revascularization (0.65) and UAP (0.82), but not HHF (1.11) were below 1. The exploratory composite endpoint of new or worsening nephropathy was lower with semaglutide than with placebo, mainly driven by the component new onset of persistent macroalbuminuria.
The MACE results were consistent across multiple sensitivity analyses and subgroups including those with established CVD or CKD (HR 0.72, 95% CI 0.55, 0.93) versus CV risk factors only (HR 1.00, 95% CI 0.41, 2.46), interaction P =0.493.3
PIONEER-6
A total of 137 patients had an EAC-confirmed MACE, fewer with semaglutide than with placebo resulting in a 21% risk reduction. The risk difference was driven by fewer CV deaths and non-fatal stroke, but more patients experienced non-fatal myocardial infarction with semaglutide. In addition, a statistically significant reduction in all-cause mortality was observed with oral semaglutide. The results of the expanded MACE were in line with the results for the primary MACE analysis. The HR point estimate was 1.56 for hospitalization for UAP and 0.86 hospitalization for HF. The results of the sensitivity analyses were consistent with the primary results. With the exception of age (HR 0.51 for age ≤65 years and HR of 1.01 for age ≥65 years, interaction P =0.051),4 there was no significant heterogeneity of treatment effect across multiple subgroups.
Impact on cardiometabolic factors
In both SUSTAIN 6 and PIONEER 6 trials, semaglutide was associated with a favorable impact on systolic blood pressure (SBP) (placebo-controlled reduction in SBP of 1.3 and 2.6 mm Hg with 0.5 and 1mg dose in SUSTAIN 6; 2.6 mmHg reduction in PIONEER 6), weight loss (placebo-controlled weight loss of 2.9 and 4.3 kg with 0.5 and 1mg dose in SUSTAIN 6; 3.4 kg weight loss in PIONEER 6), and glycemic control (placebo-controlled reduction in HbA1c of 0.7% and 1.0% with 0.5 and 1mg dose in SUSTAIN 6; 0.7% reduction in PIONEER 6). The mean pulse rate increased by 2 and 2.5 bpm with 0.5 and 1.0 mg dose of semaglutide in SUSTAIN 6, and by 4 bpm in PIONEER 6.
Safety of Semaglutide
The safety profile of semaglutide was overall consistent with that of the GLP-1 receptor agonists (RA) class, with gastrointestinal adverse events being the most frequently reported adverse drug reactions with semaglutide. The risk of severe hypoglycemia was low, typically increased in conjunction with SU or insulin therapy. No increased risk of pancreatitis, pancreatic cancer or thyroid medullary cancer was observed, although the duration of exposure was limited. One new safety finding emerged from SUSTAIN 6 – an increased risk of diabetic retinopathy complications primarily in patients with pre-existing diabetic retinopathy (HR 1.76, 95% CI 1.11, 2.78).3 A similar, but nonsignificant risk was also observed with liraglutide in LEADER.6 The available data suggest that this might be associated with pronounced improvement in glycemic control as seen with insulin therapy. Despite patients with proliferative diabetic retinopathy being excluded from PIONEER 6, a 0.8% increase in diabetic retinopathy was observed with oral semaglutide.4 A dedicated ophthalmic trial (FOCUS) of 5 years treatment duration will assess the long-term effect of semaglutide on diabetic retinopathy development and progression.7
Regulatory Status
Both subcutaneous semaglutide (Ozempic®) and oral semaglutide (Rybelsus®) are indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus.1,2 Both are not recommended as first-line therapy for patients inadequately controlled on diet and exercise. The Ozempic® label states that there have been no clinical studies establishing conclusive evidence of macrovascular risk reduction with semaglutide, whereas the Rybelsus® label is silent with respect to CV risk.
The sponsor has submitted supplemental NDA for a CV risk reduction indication based on the combined CVOT data with both subcutaneous and oral preparation.
Arguments in favor include:
- The systemic effects of semaglutide are the same, whether administered subcutaneously or orally.
- The two CVOTs were well-conducted with high retention rates and vital status known at end-of-trial for nearly all patients, allowing for robust conclusions.
- Primary endpoint of MACE was evaluated by an external independent blinded event adjudication committee, and MACE endpoints were defined using robust criteria in line with regulatory guidelines for trials designed to evaluate efficacy.
- The risk reduction in MACE in SUSTAIN 6 was supported by the favorable outcome in PIONEER 6, thereby providing independent confirmation.
- The impact on cardiometabolic factors were generally consistent.
- No difference in safety outcomes was observed across the trials.
Arguments against include:
- The overall quantum of evidence might not be sufficient to support a claim of CV risk reduction. Collectively, the two trials have 391 MACE events (254 in SUSTAIN-6 and 137 in PIONEER-6) and the follow-up is 2.1y and 1.3y, respectively, both less than what is recommended by the 2008 FDA guidance for CV safety indication (622 events over a minimum of 2 year follow-up to rule out a HR of 1.30).
- Both trials were not designed to either rule out post-approval noninferiority boundary of HR of 1.3, or to establish superiority.
- Closer scrutiny of the data reveals differences in individual CV outcomes among the trials. For example, with the exception of stroke findings, there are inconsistencies among the two trials with regards to impact on CV death and all-cause mortality (favorable impact in PIONEER-6), nonfatal MI and UAP (favorable impact in SUSTAIN-6) and hospitalization for heart failure (favorable impact in PIONEER-6). The discordant effects on the individual endpoints despite similar pharmacokinetic exposure challenges the argument of consistent exposure-response relationship.
- How does a treatment that does not reduce MI reduce mortality by 50%, and that too after only 1-year of treatment exposure? Given the small number of mortality events in PIONEER 6 (68 all-cause mortality and 45 CV deaths), it is difficult to rule out the possibility that the mortality risk reduction might represent a play of chance (so-called 'random high')?
- The FDA rarely utilizes pooled analysis or meta-analysis to justify regulatory decisions to support CV efficacy claims. Combining trial data for two different formulations of the same drug to support an efficacy claim would represent a precedent-setting decision, at least in this therapeutic area.
The FDA decision is expected in the first quarter of 2020. If approved for CV risk reduction, both subcutaneous and oral semaglutide would represent a major advance in mitigating CV risk in patient with T2D.
References
- https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/209637lbl.pdf. Accessed December 1, 2019.
- FDA approves first oral GLP-1 treatment for type 2 diabetes (FDA website). Available at: https://www.fda.gov/news-events/press-announcements/fda-approves-first-oral-glp-1-treatment-type-2-diabetes. Accessed December 1, 2019.
- Marso SP, Bain SC, Consoli A, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med 2016;375:1834-44.
- Husain M, Birkenfeld AL, Donsmark M, et al. Oral semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med 2019;381:841-51.
- U.S. Food and Drug Administration. Guidance for Industry. Diabetes Mellitus - Evaluating Cardiovascular Risk in New Antidiabetic Therapies to Treat Type 2 Diabetes. 2008. Available at: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/diabetes-mellitus-evaluating-cardiovascular-risk-new-antidiabetic-therapies-treat-type-2-diabetes. Accessed December 1, 2019.
- Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med 2016;375:311-22.
- A Research Study to Look at How Semaglutide Compared to Placebo Affects Diabetic Eye Disease in People With Type 2 Diabetes (FOCUS). Available at: https://clinicaltrials.gov/ct2/show/NCT03811561. Accessed December 1, 2019.
Clinical Topics: Arrhythmias and Clinical EP, Diabetes and Cardiometabolic Disease, Heart Failure and Cardiomyopathies, Atrial Fibrillation/Supraventricular Arrhythmias, Acute Heart Failure
Keywords: Diabetes Mellitus, Diabetes Mellitus, Type 2, Glucagon, Insulin Resistance, Heart Failure, Risk Factors, Retrospective Studies, Cohort Studies, Cardiovascular Diseases, Atrial Fibrillation, Coronary Vessels, Blood Pressure, Brain Ischemia, Stroke, Insulin, Regular, Human, Myocardial Infarction, Inflammation, Primary Health Care, Glucagon-Like Peptide 1, Hypoglycemia, Renal Insufficiency, Chronic, Injections, Subcutaneous, Blood Glucose, United States Food and Drug Administration, Diabetic Retinopathy, Creatinine, Heart Rate, Insulin, Regular, Human, Pancreatic Neoplasms, Drug-Related Side Effects and Adverse Reactions, Demography, Metabolic Syndrome
< Back to Listings