Exercise in Aortopathy: How Should We Counsel Our Patients?
Quick Takes
- Counseling an athlete with aortopathy on competitive sport participation requires an understanding of the hemodynamic stresses exercise can impose on the aortic wall.
- Identification of a potential inherited aortopathy is an important component of the evaluation of an athlete in whom there is concern.
- Professional society recommendations in this area are based largely on expert opinion rather than robust scientific evidence, necessitating an individualized, shared decision-making approach in many cases.
The biomechanics of physical exercise can impose acute hemodynamic stresses on the cardiovascular system. With regular intense exercise, the cardiac chambers may remodel in a manner that is often described as the "athlete's heart." While the adaptive changes in ventricular and atrial morphology are acknowledged, less appreciated are the effects of exercise on the aorta. Intense exercise induces elevations in systolic blood pressure (SBP) due to increased cardiac output in endurance sports and increased peripheral vascular resistance in strength-based sports. The hemodynamic effect of longstanding hypertension on aortic size is well documented and newer data suggests that the hemodynamic stress of high intensity exercise over many years may also result in aortic remodeling and enlargement.1 With increasing aortic size comes concern for risk of aortic injury, most concerningly aortic rupture and dissection. While it seems unlikely that the mild aortic enlargement seen in most athletes is dangerous, it may be significant in athletes who have an underlying aortopathy.
Aortopathies may be familial and related to connective tissue disorders, notably Marfan syndrome, and are also commonly observed in patients with bicuspid aortic valves (BAV). The impact of exercise in these conditions is understudied, but there are concerns that these athletes may be at increased risk of aortic rupture or dissection with exercise. Guidance in these scenarios necessitates a nuanced approach, directed by knowledge of the hemodynamic stresses of an athlete's sport and how these stresses may impact disease progression.
In this expert analysis, we review key questions that often arise when screening for and evaluating aortopathies in athletes.
Does exercise increase aortic sizes?
The normal range of aortic size depends on an individual's age, gender, and body size, as measured by body surface area (BSA). For the general population, gender and age specific nomograms based on BSA are available,2 and determination of the Z-score (standard deviations above or below predicted values) can help assess how a patient's aortic size compares to similarly sized individuals. Importantly, nomograms specific to athletes are not available. Notably, while aortic size tends to correlate with body size in the general population, there appears to be a plateau at approximately 40 mm for aortic root size. In a study of active players in the National Basketball Association, even in the tallest male athletes, it was uncommon for players to have an aortic root size >42 mm.3
In a meta-analysis by Iskandar et al., elite athletes were found to have larger aortic root diameters (3.2 mm larger at the sinuses of Valsalva) compared to non-athlete controls.4 Notably, this meta-analysis only included studies where the mean age of the cohort was between 15–40 years old. In these prior studies of young athletes, while they may have slightly larger aortic sizes compared to more sedentary controls, it is rare to find aortic root sizes ≥40 mm in men and ≥34 mm in women. Interestingly, a more recent cross-sectional analysis of veteran endurance athletes (masters level rowers and runners) with a mean age of 61 years found that roughly half of these athletes had clinically relevant dilation of their aortas (≥40 mm).1 Further, elite competitor status was independently associated with aortic size. Similarly, a cross-sectional study of retired National Football League players (mean age of 57 years) found that these elite athletes were twice as likely as demographically-matched controls in the Dallas Heart Study to have an aortic size >40 mm, even after adjusting for risk factors such as age, size, race, hypertension, diabetes mellitus, and smoking.5
It remains unclear whether the two major modalities of exercise – strength training and dynamic/endurance training – differ in their potential contributions to aortic enlargement. Strength training has been associated with increased aortic stiffness, while endurance training has been associated with increased aortic distensibility.6 In the previously mentioned cross-sectional analysis of veteran athletes, rowing (combination of high levels of both strength and endurance training) was independently associated with aortic size.1
Based on these observations, there is evidence to suggest that regular exercise may promote aortic enlargement, but even in elite athletes, this enlargement is minimal at younger ages, therefore, clinically significant enlargement warrants further investigation in the young athlete. However, with continued masters level endurance sport participation through the sixth decade of life, aortic dilation is commonly seen. More studies are needed to better understand the clinical relevance of aortic dilation in this population, but for now it is prudent to recommend serial monitoring of these veteran athletes.
How should we counsel athletes with known aortopathy on competitive sports participation?
An enlarged aortic root (>40 mm or Z-score >2) in a young athlete should prompt an evaluation for an inherited aortopathy. These include aortopathies associated with a BAV, Marfan syndrome, and other connective tissue disorders such as Loeys-Dietz syndrome. Echocardiography should be performed to identify BAV, while the diagnosis of Marfan syndrome can be aided by clinical criteria outlined in the Systemic Score.7 If there is sufficient concern, genetic testing should be pursued.
For athletes diagnosed with an aortopathy, counseling on exercise recommendations and competitive sports participation can be challenging as guidelines are largely based on expert recommendation given the limited data available in this area. The most recent guidelines are the 2015 American Heart Association (AHA) / American College of Cardiology (ACC) Eligibility and Disqualification Recommendations for Competitive Athletes with Cardiovascular Abnormalities.8 The primary goals of these recommendations are to avoid precipitating an acute aortic event (dissection or rupture) and to mitigate aortic enlargement. In the absence of clear safety data, these recommendations are understandably conservative.
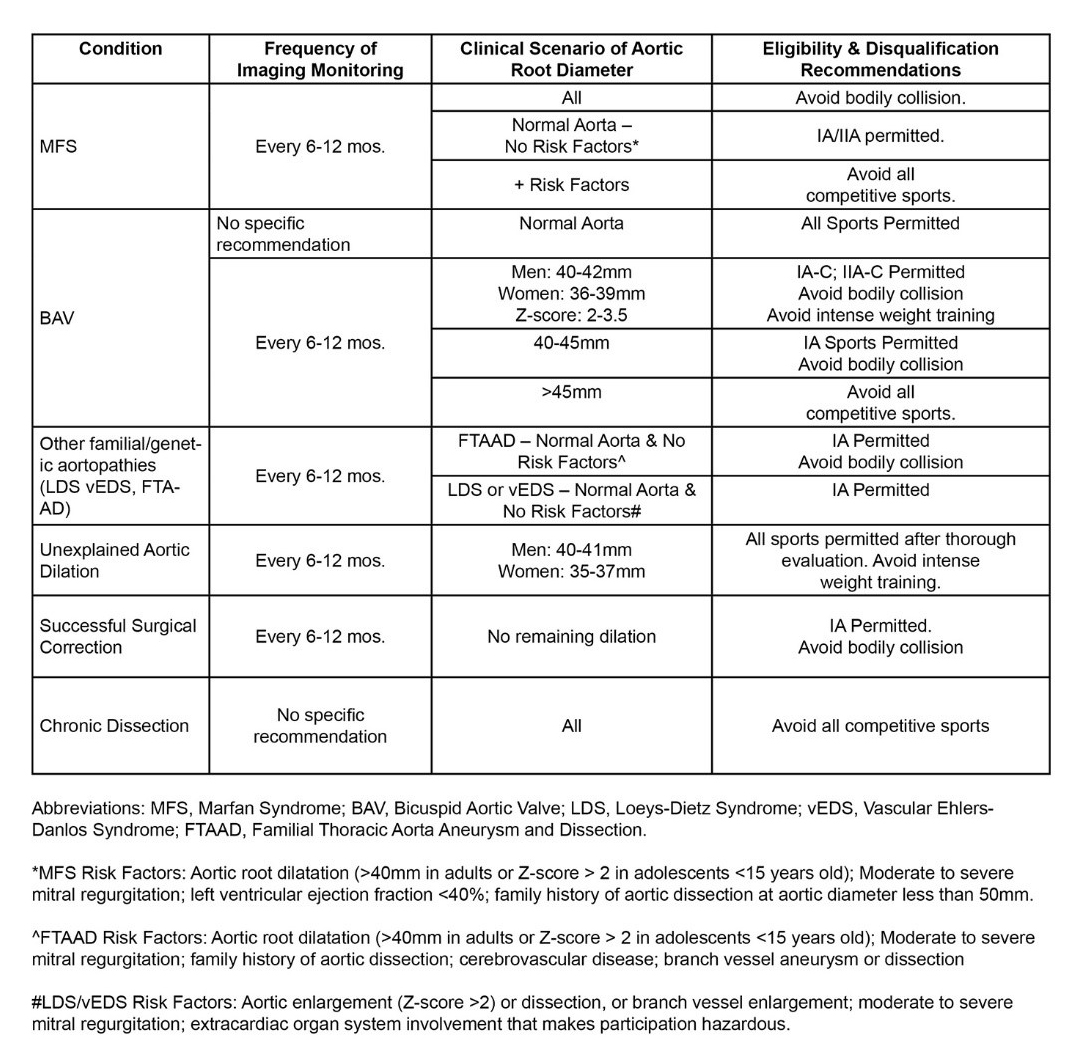
With regards to competitive sports participation, the two major components that guide recommendations are: (1) presence and type of underlying aortopathy, and (2) the presence of high-risk features. These high-risk features include the presence and degree of aortic enlargement (Z-score >2 or aortic root diameter >40 mm), and a family history of an acute aortic event. Additionally, the type of competitive sport played (evaluated in terms of the static and dynamic components) and the risk of bodily collision need to be considered. The AHA/ACC recommendations are summarized below in Table 1. Generally speaking, for athletes who have a known aortopathy as well as associated high-risk features, it is recommended that they avoid all competitive sports. For athletes who have a known aortopathy but no other risk factors, certain sports may be permitted depending on the underlying condition and the aortic size, though those that involve bodily collision should be approached with caution. For athletes who are found to have a mildly enlarged aorta (Z-scores of 2-2.5; aortic root of 40-41 mm in men or 35-37 mm in women) with no clear aortopathy identified after a thorough evaluation, it is reasonable to allow all competitive sports, but they should be counseled to generally avoid intense weight training. Importantly, serial monitoring of the aortic dimensions should be performed every 6-12 months to monitor for growth and rate of progression for all athletes with concern for aortic disease.
Table 1: Summary of Monitoring and Eligibility/Disqualification Recommendations for Athletes with Aortopathies (Reprinted with Permission from Hedley and Phelan9)
How should we counsel patients with known aortopathy on non-competitive exercise?
Unfortunately, there is little data to guide safe levels of exercise in athletes with aortopathy. Therefore, recommendations for exercise in such individuals should be individualized to the athlete, with specific attention to the expected blood pressure responses and risks of bodily collision in their exercises of choice. The goal in these athletes is to minimize the likelihood of hemodynamic stresses that could predispose to either an acute aortic event or acceleration of aortic enlargement. Such stresses could include acute and/or sustained large increases in mean arterial pressure (MAP) that exceed the rupture threshold of the aorta, as well as sudden decelerations that can occur during bodily collision.
In general, aerobic exercise (e.g., running, swimming) does not dramatically increase MAP. Thus, for most athletes with a mild or moderately dilated aorta, aerobic exercise is thought to be reasonably safe, with serial monitoring of aortic size and absent any risk of bodily collision.
On the contrary, resistance exercise (e.g., weightlifting) can dramatically and acutely increase both SBP and diastolic blood pressure (DBP), thereby increasing MAP. Some studies have shown that SBP can reach as high as 400 mmHg during weightlifting using large muscle groups.10 Thus, the general sentiment among providers has been to recommend that athletes with aortopathy avoid heavy weightlifting, and avoid using the Valsalva technique while lifting. However, the definition of "heavy weightlifting" is unclear and the impact of the Valsalva maneuver on aortic wall stress is controversial. The hemodynamic stress of weightlifting differs depending on the strength of the individual, the intensity of the exercise, the exercise maneuver, the level of muscle fatigue, and the breathing technique used while lifting. Knowledge of all these factors are required to provide an individualized weight-lifting prescription for the athlete with aortopathy. Importantly, during exercise, a number of forces are exerted on the aorta; while the intravascular SBP may increase acutely during weightlifting, a study by Hakykowsky et al. found that increases in transmural pressure may be opposed by increases in extravascular intrathoracic pressure during Valsalva.11 The transmural pressure (intravascular – intrathoracic pressure), describing the net outward pressure against the aortic wall, may not increase dramatically during weightlifting with the Valsalva technique, as Valsalva increases intrathoracic pressure significantly. More research is needed to better understand the hemodynamic stresses on the aortic wall during exercise, and an individualized approach that recognizes these nuances is recommended when counseling patients with aortopathies on isometric exercise.
How should we counsel athletes who have undergone aortic surgery on non-competitive exercise?
For athletes who have undergone surgical correction of their aortic dissection or aneurysm, the 2015 AHA/ACC Scientific Statement recommends that if there is no evidence of residual aortic enlargement or dissection, participation in low static and low dynamic (Class IA) sports without potential for bodily collision is reasonable.8 Importantly, one key question to ask is what caused the aneurysm or dissection? If there is a known aortopathy or syndromic condition that renders the unrepaired portion of the aorta at risk, recommendations should focus on preventing injury there. Athletes with bicuspid aortopathy, where the root and ascending aorta are replaced, are likely at minimal risk of further acute aortic syndrome, and we may be more permissive in their exercise recommendations. Of course, for athletes who have undergone sternotomy, adequate time should be allowed for wound healing and stabilization. For athletes who wish to participate in sports that require bodily collision, a discussion with the surgeon is recommended to assess suitability for alternative surgical approaches to full sternotomy or use of surgical techniques to reinforce the sternum given potential concerns about repetitive collisions. For most individuals, it is important to highlight the benefits and importance of maintaining an active lifestyle with regular moderate aerobic exercise. As discussed above, activities involving significant isometric maneuvers should be avoided in most. For athletes considering these activities, individualized exercise prescriptions can be helpful. Notably, while there are professional athletes who have returned to competition after aortic surgery without incident, these decisions were made using a shared decision-making strategy, against current recommendations and serve to highlight the importance of an individualized, tailored approach that should be used for athletes in these situations.
Conclusion
In summary, the aorta is exposed to significant hemodynamic stresses during exercise, and counseling on participation in competitive sports and routine exercise in those with aortic disease requires an understanding of the stresses these activities can impose on the aortic wall. Identifying potential inherited aortopathies is an important component of the evaluation of athletes in whom there is concern, as their presence will influence these recommendations. While professional society recommendations regarding sport participation in aortic disease do exist, it should be reiterated that these are based largely on expert opinion rather than robust scientific evidence. These recommendations can be a very helpful starting point in guiding exercise activities in athletic patients, but an individualized, shared decision-making approach is often required.
References
- Churchill TW, Groezinger E, Kim JH, et al. Association of ascending aortic dilatation and long-term endurance exercise among older masters-level athletes. JAMA Cardiol 2020;5:1-10.
- Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 2015;28:1-39.e14.
- Engel DJ, Schwartz A, Homma S. Athletic cardiac remodeling in US professional basketball players. JAMA Cardiol 2016;1:80–7.
- Iskandar A, Thompson PD. A meta-analysis of aortic root size in elite athletes. Circulation 2013;127:791–8.
- Gentry JL III, Carruthers D, Joshi PH, et al. Ascending aortic dimensions in former National Football League athletes. Circ Cardiovasc Imaging 2017;10:e006852.
- D'Andrea A, Cocchia R, Riegler L, et al. Aortic stiffness and distensibility in top-level athletes. J Am Soc Echocardiogr 2012;25:561–7.
- Loeys BL, Dietz HC, Braverman AC, et al. The revised Ghent nosology for the Marfan syndrome. J Med Genet 2010;47:476–85.
- Braverman AC, Harris KM, Kovacs RJ, Maron BJ. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: Task Force 7: aortic diseases, including Marfan syndrome: a scientific statement from the American Heart Association and American College of Cardiology. J Am Coll Cardiol 2015;66:2398–2405.
- Hedley JS, Phelan D. Athletes and the aorta: normal adaptations and the diagnosis and management of pathology. Curr Treat Options Cardiovasc Med 2017;19:88.
- Mayerick C, Carré F, Elefteriades J. Aortic dissection and sport: physiologic and clinical understanding provide an opportunity to save young lives. J Cardiovasc Surg (Torino) 2010;51:669–81.
- Haykowsky M, Taylor D, Teo K, Quinney A, Humen D. Left ventricular wall stress during leg-press exercise performed with a brief Valsalva maneuver. Chest 2001;119:150–4.
Clinical Topics: Cardiac Surgery, Cardiovascular Care Team, Congenital Heart Disease and Pediatric Cardiology, Diabetes and Cardiometabolic Disease, Heart Failure and Cardiomyopathies, Prevention, Sports and Exercise Cardiology, Valvular Heart Disease, Vascular Medicine, Aortic Surgery, Cardiac Surgery and CHD and Pediatrics, Cardiac Surgery and Heart Failure, Cardiac Surgery and VHD, Congenital Heart Disease, CHD and Pediatrics and Prevention, CHD and Pediatrics and Quality Improvement, Exercise, Sports and Exercise and Congenital Heart Disease and Pediatric Cardiology
Keywords: Sports, Marfan Syndrome, Cross-Sectional Studies, Blood Pressure, Resistance Training, Football, Basketball, Loeys-Dietz Syndrome, American Heart Association, Vascular Stiffness, Risk Factors, Body Surface Area, Aortic Rupture, Nomograms, Valsalva Maneuver, Muscle Fatigue, Arterial Pressure, Sternotomy, Expert Testimony, Aortic Valve, Lifting, Decision Making, Deceleration, Goals, Heart Valve Diseases
< Back to Listings