How Many South Asians Does It Take? Coronary Artery Calcium to Refine Statin Allocation in a High-Risk Ethnicity
Quick Takes
- Among South Asian adults at intermediate risk, 30% had coronary artery calcium (CAC)=0; for participants at borderline risk, 54% had CAC=0, suggesting a potential for overtreatment in these patients.
- Instead of systemic recommendations for statins in all South Asians adults in the United States (SAUS) at intermediate and borderline risk, the use of additional risk stratification tools such as CAC score could aid to personalize allocation of preventive pharmacotherapy.
- It is important to focus on implementing strategies such as early screening for ASCVD risk factors (namely, hypertension, diabetes, and obesity) and promoting culturally appropriate awareness on a healthy diet and lifestyle choices to reduce the burden of cardiovascular disease among SAUS.
Commentary based on Haque W, Grandhi GR, Kanaya AM, et al. Implications of the 2019 American College of Cardiology/American Heart Association primary prevention guidelines and potential value of the coronary artery calcium score among South Asians in the US: the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study. Atherosclerosis 2021;334:48-56.1
South Asians are at an approximately two-fold elevated risk for atherosclerotic cardiovascular disease (ASCVD) when compared to other racial and ethnic groups.2-6 To improve prevention efforts among South Asians in the United States (SAUS), the 2018 American Heart Association (AHA)/American College of Cardiology (ACC)/Multi-society guideline on the management of blood cholesterol7 and the 2019 ACC/AHA primary prevention guideline8 lists South Asian ethnicity as a "risk-enhancing factor" to guide ASCVD risk stratification. Based on these guidelines, statin therapy is often recommended in SAUS patients at "borderline/intermediate" risk.
However, the pooled cohort equations (PCE) tend to overestimate risk in SAUS, which may lead to a substantial increase in the number of prescriptions for statin pharmacotherapy. Importantly, if drug therapy is considered, the intensity of therapy should match one's absolute risk as to maximize benefit and minimize harms.9 Considering the heterogenous risk encountered among those at intermediate risk, the selective use of coronary artery calcium (CAC) has been shown to improve risk estimation more than any currently available risk marker. Specifically, a CAC=0 is associated with low ASCVD event rates.
Considering this, Haque et al. explored the implications of implementing the ACC/AHA recommendations for ASCVD risk assessment in SAUS and of considering South Asian ethnicity as a risk-enhancing feature using data from the prospective, observational Mediators of Atherosclerosis in South Asians Living in America (MASALA) study.
Summary of the Study
- Overall, 1,114 adults of South Asian ancestry (ages of 40 to 75 years), free of known baseline ASCVD were enrolled. The study group had a median age of 56 years and 48% were women. The prevalence of current tobacco use was very low (3%), 19% used medications for hypertension, 61% had prediabetes, and 79% had abdominal obesity. Among the enrolled participants, 447 participants (41%) were either current statin users or would be considered to benefit from statin therapy, irrespective of their ASCVD risk. Among the remaining 660 study participants (59%) who qualified for a 10-year ASCVD risk assessment for statin allocation purposes, the prevalence of low, borderline, intermediate, and high estimated ASCVD risk was 65%, 11%, 20% and 5%, respectively. The prevalence of CAC=0 decreased with increasing ASCVD risk. Within these 660 study participants, 72 were categorized as borderline risk and 131 were at intermediate risk, respectively.
- An absence of CAC was found in 30% of participants at intermediate estimated-risk, and in 54% at borderline-risk, respectively. As opposed to only treating participants in the high-risk group, additional statin consideration in patients with intermediate risk would significantly increase the number of patients with CAC=0 being treated with statins from 1% to 10% of all participants with CAC=0. For those at borderline risk, the absolute number of individuals with CAC=0 being treated with statins would increase from 44 to 83 (19% of participants with CAC=0).
- The prevalence of features associated with incident diabetes, namely prediabetes and abdominal obesity, was very high across all the groups in the MASALA population, including in those considered to be at low risk for ASCVD, 66% overall and 59% in individuals with CAC=0 for prediabetes, and 79% overall and 89% for individuals with CAC=0 for abdominal obesity.
The Cholesterol 2018 Guideline7 suggests that statin therapy should be considered in all SAUS at intermediate and borderline-risk. However, the PCE does not accurately assess cardiovascular risk among SAUS patients. As the PCE was derived from populations devoid of South Asians, an inherent limitation is that South Asian ethnicity is defaulted to "White" race, despite considerably different risk factor profiles.
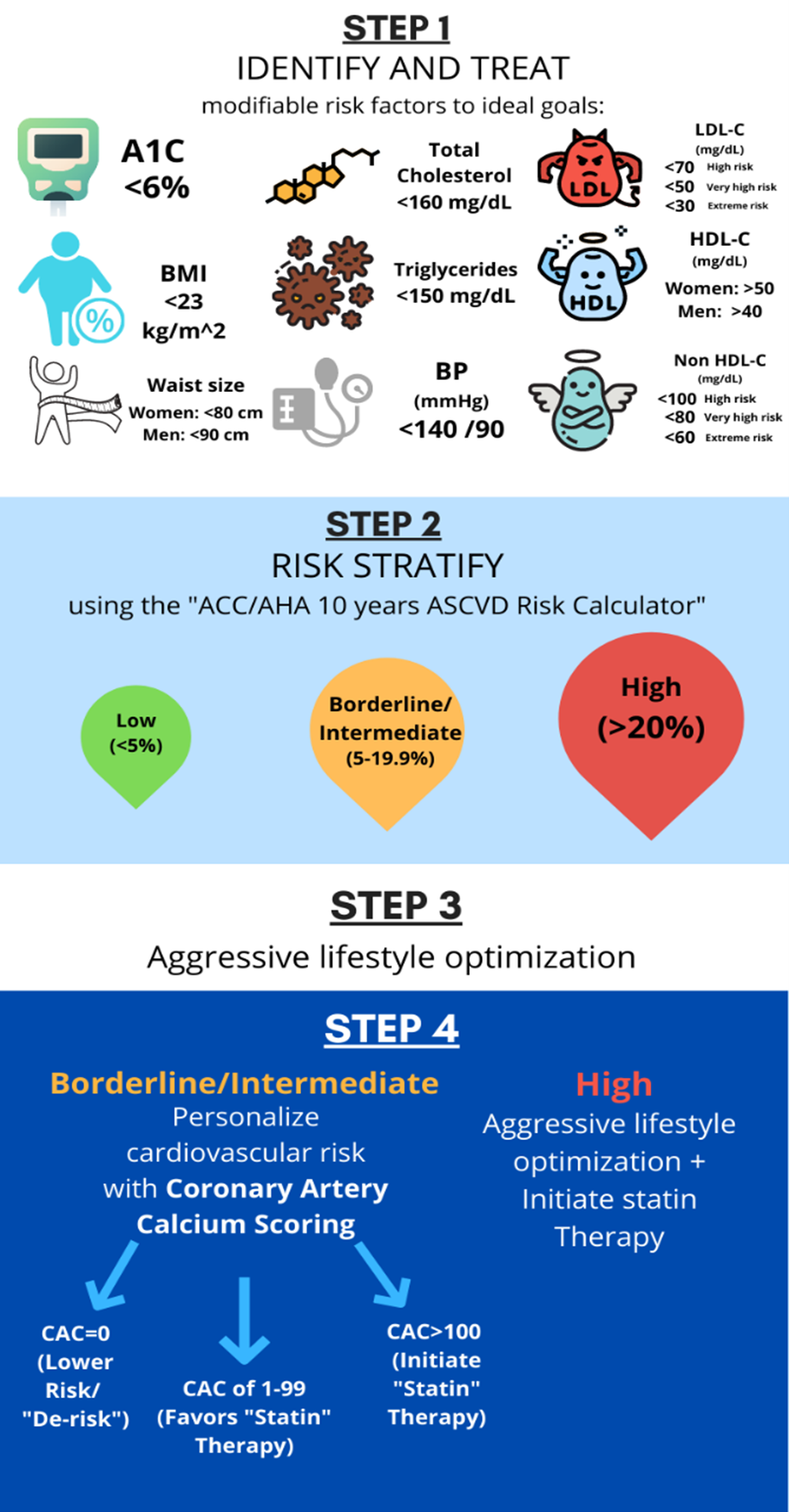
Statin consideration in SAUS participants at intermediate and borderline risk would greatly increase the number of SAUS qualifying for statins, which may result in over treatment of those with no CAC. Findings from this study suggest that the use of CAC scoring may aid in short-term risk stratification to guide allocation of preventive cardiovascular therapies, such as statins and aspirin, with potential to expand to antihypertensive and cardiometabolic medications.10,11 Notably, the use of CAC may have the greatest impact in those at borderline-risk, where the frequency of CAC=0 was four-fold that of CAC>100. Figure 1 depicts strategies for individualizing cardiovascular risk stratification among SAUS patients.
Figure 1
MASALA is a contemporary cohort with a larger proportion of younger patients than other prospective studies such as Multi-Ethnic Study of Atherosclerosis (MESA) and the Framingham Heart Study. As such, risk may be underestimated considering age is a significant factor in the PCE. However, once CAC is assessed, chronological age is less important.12 While we await further data on cardiovascular events in MASALA, additional evidence from the Coronary Artery Risk Development in Young Adults (CARDIA) study demonstrates that the presence of CAC in young patients suggests a heightened risk of future ASCVD.13,14 Indeed, the presence of traditional risk factors was associated with increased risk of cardiovascular events across all the CAC strata, including among those with CAC=0 among young patients (18-45 years) from the Western Denmark Heart Registry.14
Cautious Use of CAC Scoring in SAUS
One limitation of the MASALA study arises in generalizing the protective prognosis associated with CAC=0 to SAUS given the characteristics of the cohort: younger, established statin use, highly educated and high-income, and mainly Indian origin (lower-risk SAUS subgroup compared to adults from Pakistan and Bangladeshi). It is advisable to use caution given the lack of incident data among SAUS. Nonetheless, other prospective populations such as MESA, Atherosclerosis Risk in Communities Study (ARIC), and the Dallas Heart Study, for example, provide reassurance that CAC scoring can aid risk stratification and "de-risking" when CAC=0 even in the presence of traditional (such as hypertension and diabetes) and risk-enhancing factors across different ethnicities.15-17
Risk Factor Management
A concerningly high prevalence of prediabetes and abdominal obesity was observed in the MASALA population, including in those considered to be low risk for ASCVD. In line with established lower body mass index (BMI) thresholds and recommendations offered by the American Diabetes Association, diabetes screening should be offered to SAUS with a BMI>23 kg/m2.18 The staggering preponderance of prediabetes among MASALA participants highlights the elevated prevalence witnessed in other SAUS populations.19 This underscores the significance of primordial prevention and, once again, underscoring the need for early, aggressive interventions aimed at identifying, preventing, and easing the progression of these risk factors; a crucial step towards curtailing the development of ASCVD in SAUS.
Conclusion
While it is a commendable step to consider South Asian ethnicity as a risk-enhancing factor and further prevention efforts in this high-risk group, systematic consideration of statins in all intermediate and borderline-risk individuals would greatly increase the number of SAUS with CAC=0 being treated with statins, likely resulting in overtreatment. Enriched clinician-patient discussions and risk stratification with CAC may aid appropriate allocation of preventive pharmacotherapies in this ethnic group. It is critical to educate our patients and implement culturally appropriate, guideline recommended screening and aggressive lifestyle interventions to reduce the future risk of incident cardiovascular disease.
References
- Haque W, Grandhi GR, Kanaya AM, et al. Implications of the 2019 American College of Cardiology/American Heart Association primary prevention guidelines and potential value of the coronary artery calcium score among South Asians in the US: the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study. Atherosclerosis 2021;334:48-56.
- Forouhi NG, Sattar N, Tillin T, McKeigue PM, Chaturvedi N. Do known risk factors explain the higher coronary heart disease mortality in South Asian compared with European men? Prospective follow-up of the Southall and Brent studies, UK. Diabetologia 2006;49:2580-88.
- Tillin T, Hughes AD, Mayet J, et al. The relationship between metabolic risk factors and incident cardiovascular disease in Europeans, South Asians, and African Caribbeans: SABRE (Southall and Brent Revisited) -- a prospective population-based study. J Am Coll Cardiol 2013;61:1777-86.
- Hajra A, Li Y, Siu S, et al. Risk of coronary disease in the South Asian American population. J Am Coll Cardiol 2013;62:644-45.
- Klatsky AL, Tekawa I, Armstrong MA, Sidney S. The risk of hospitalization for ischemic heart disease among Asian Americans in northern California. Am J Public Health 1994;84:1672-75.
- Lee J, Heng D, Chia KS, Chew SK, Tan BY, Hughes K. Risk factors and incident coronary heart disease in Chinese, Malay and Asian Indian males: the Singapore Cardiovascular Cohort Study. Int J Epidemiol 2001;30:983-88.
- Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;73:e285-e350.
- Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019;74:1376-1414.
- Mitchell JD, Paisley R, Moon P, Novak E, Villines TC. Coronary artery calcium and long-term risk of death, myocardial infarction, and stroke: the Walter Reed Cohort Study. JACC Cardiovasc Imaging 2018;11:1799-1806.
- Nasir K, Cainzos-Achirica M. Role of coronary artery calcium score in the primary prevention of cardiovascular disease. BMJ 2021;373:n776.
- Patel J, Mehta A, Rifai MA, et al. Hypertension guidelines and coronary artery calcification among South Asians: results from MASALA and MESA. Am J Prev Cardiol 2021;6:100158.
- Tota-Maharaj R, Blaha MJ, McEvoy JW, et al. Coronary artery calcium for the prediction of mortality in young adults <45 years old and elderly adults >75 years old. Eur Heart J 2012;33:2955-62.
- Nasir K, Hecht H. Age is just a number: lowering the bar for coronary artery calcium testing. JACC Cardiovasc Imaging 2021;Aug 11:[Epub ahead of print].
- Mortensen MB, Dzaye O, Bødtker H, et al. Interplay of risk factors and coronary artery calcium for CHD risk in young patients. JACC Cardiovasc Imaging 2021;Jun 16:[Epub ahead of print].
- Patel J, Al Rifai M, Cainzos-Achirica M, et al. Family history of CHD is associated with severe CAC in South Asians: comparing the MASALA and MESA studies. JACC Cardiovasc Imaging 2017;10:958-60.
- Dzaye O, Dudum R, Reiter-Brennan C, et al. Coronary artery calcium scoring for individualized cardiovascular risk estimation in important patient subpopulations after the 2019 AHA/ACC primary prevention guidelines. Prog Cardiovasc Dis 2019;62:423-30.
- Patel J, Pallazola VA, Dudum R, et al. Assessment of coronary artery calcium scoring to guide statin therapy allocation according to risk-enhancing factors: the Multi-Ethnic Study of Atherosclerosis. JAMA Cardiol 2021;6:1161-70.
- Hanif W, Ali SN, Bellary S, et al. Pharmacological management of South Asians with type 2 diabetes: consensus recommendations from the South Asian Health Foundation. Diabet Med 2021;38:e14497.
- Eastwood SV, Tillin T, Sattar N, Forouhi NG, Hughes AD, Chaturvedi N. Associations between prediabetes, by three different diagnostic criteria, and incident CVD differ in South Asians and Europeans. Diabetes Care 2015;38:2325-32.
Clinical Topics: Cardiovascular Care Team, Diabetes and Cardiometabolic Disease, Dyslipidemia, Prevention, Lipid Metabolism, Nonstatins, Novel Agents, Statins, Hypertension
Keywords: Hydroxymethylglutaryl-CoA Reductase Inhibitors, Antihypertensive Agents, Prospective Studies, Ethnic Groups, Body Mass Index, Cardiovascular Diseases, Coronary Vessels, American Heart Association, Prediabetic State, Obesity, Abdominal, Aspirin, Risk Factors, Atherosclerosis, Primary Prevention, Risk Assessment, Prognosis, Hypertension, Asian Continental Ancestry Group, Cholesterol, Registries, Tobacco Use, Prescriptions, Heart Disease Risk Factors
< Back to Listings