COVID-19 Increases Long-Term Risk of Ischemic and Non-Ischemic Cardiovascular Disease
Quick Takes
- COVID-19 infection is associated with an increase in the incidence and burden of long-term CVD, including arrythmias, ischemic and non-ischemic heart disease, myopericarditis, ischemic stroke, and venous thromboembolism.
- The severity of the acute phase of the COVID-19 infection correlates with the incidence and burden of CVD, but even non-hospitalized patients with relatively mild cases of COVID-19 have an increased risk.
- Clinicians should counsel patients on the risks of CVD to emphasize the importance of primary prevention through vaccination for COVID-19.
Introduction
The SARS-CoV-2 virus, which causes coronavirus disease 2019 (COVID-19), has caused a pandemic of unparalleled proportions.1 Although initially thought to be a disease of respiratory symptoms alone, further studies have elucidated its impact on other organ systems, including the cardiovascular system.2
COVID-19 is linked to an increased risk of ST-elevation myocardial infarction (STEMI)3 and myocarditis4 during the acute, hospitalized phase; even myocardial injury has been associated with higher morbidity and mortality for patients with COVID-19.5 The cardiovascular effects of COVID-19 appear to be more common than those seen in other viruses, such as influenza.6 However, until recently, an understanding of the long-term cardiovascular effects of COVID-19 has not been established.
Long-Term Risk of Cardiovascular Disease with COVID-19
A recent publication by Xie et al. demonstrated that COVID-19 causes a long-term increase in arrythmias, ischemic and non-ischemic heart disease, myopericarditis, ischemic stroke, and venous thromboembolism. The authors analyzed a cohort of 153,760 patients from the US Department of Veterans Affairs (VA) national healthcare database and compared these patients to two control cohorts (one cohort without COVID-19 during the same period and another cohort of any patients who visited the VA pre-dating the pandemic). They found an increased incidence and burden of cardiovascular disease (CVD) at 1-year for patients with any severity of COVID-19 disease.7
The severity of the acute infectious phase correlated with the increased incidence and burden of CVD. Severity of infection was defined by level of care required. Patients with the most severe COVID-19, such as those who were treated in the intensive care unit, had greater CVD. However, even patients with relatively mild cases of COVID-19, such as those who were not hospitalized, had an increased risk of future CVD.7
The greatest increase was in atrial fibrillation and heart failure for patients with COVID-19 regardless of sex, age, race, or pre-existing traditional risk factors including hypertension, obesity, diabetes, and hyperlipidemia.7 These findings demonstrate the profound adverse impact of COVID-19 on the cardiovascular system, even for patients who were formerly healthy.
The Role of Endothelial Dysfunction
SAR-CoV-2 infects the host cell through the angiotensin converting enzyme 2 (ACE2) receptor. ACE2 receptors are expressed in multiple sites, including the lung, heart, kidney, intestine, and vasculature. Endothelial cells have emerged as a key target of research in the pathophysiology for COVID-19. Post-mortem analyses in pathology have demonstrated direct infection of the virus into endothelial cells. This direct infection can lead to diffuse endothelial inflammation, extensive endothelial dysfunction, and cellular apoptosis.8
Endothelial dysfunction is part of the pathophysiology for both COVID-19 and CVD. Patients who are elevated risk for CVD often show evidence of endothelial dysfunction, and endothelial dysfunction has been linked to atherosclerosis through an inflammatory response to shear stress.9 Diabetic patients demonstrate accelerated atherosclerosis for their age thought to be secondary to endothelial dysfunction,10 which has also been linked to the pathophysiology of heart failure with reduced and preserved ejection fraction.11 This connection may explain why diseases with known endothelial dysfunction, such as hypertension, obesity, and diabetes, are associated with worse COVID-19 outcomes.12
Myocardial inflammation is another source of cardiovascular dysfunction in COVID-19. Active inflammation has been seen on cardiac magnetic resonance imaging (MRI) 2-3 months after COVID-19 infection regardless of preexisting medical conditions.13 Arrhythmias may be secondary to myocardial inflammation, which can lead to fibrosis and the development of abnormal conduction pathways, such as atrial fibrillation.14 Inappropriate sinus tachycardia and postural orthostatic tachycardia syndrome may be related to persistent or inappropriate adrenergic stimulation and cytokine activation.15
These mechanisms of endothelial dysfunction, myocardial inflammation, and catecholamine activation may explain how COVID-19 increases risk of CVD, even after the acute infection.7 Much like diabetes and obesity, COVID-19 causes endothelial dysfunction, coagulopathy, and inflammation, leading to increased CVD.16
Impact on Patient Counseling
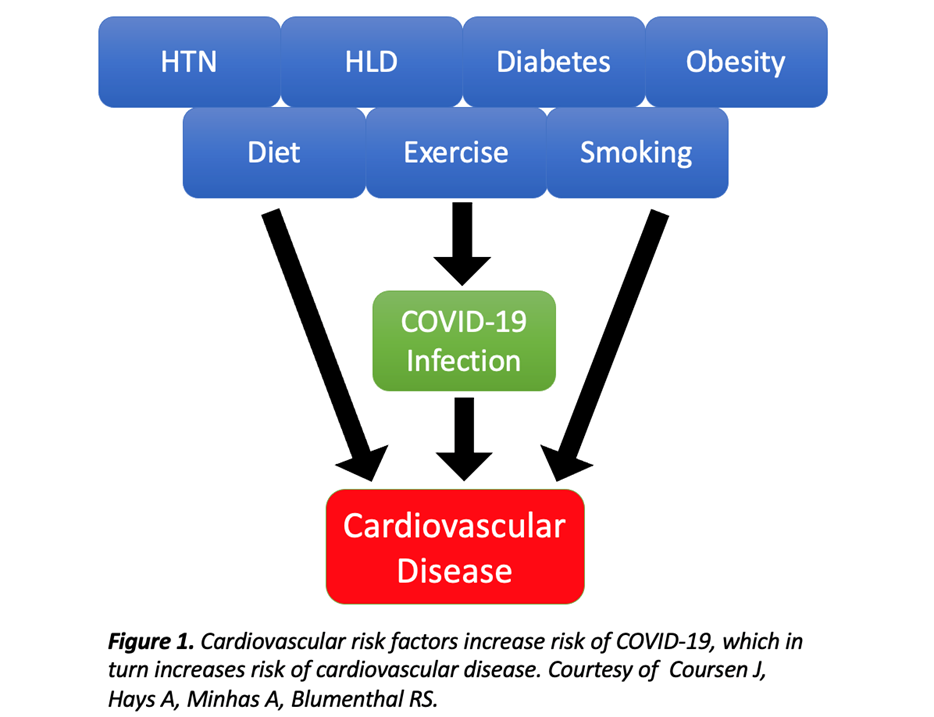
The increased risk of long-term CVD emphasizes the importance of primary prevention of COVID-19 infection. When counseling patients about COVID-19 infection, clinicians should include the established risks of CVD to motivate patients to follow public health guidelines, including pursuing COVID-19 vaccination. Counseling on the risks of CVD with COVID-19 is especially important for our patients with known cardiovascular risk factors and diseases of pre-existing endothelial dysfunction, such as atherosclerosis, hypertension, and diabetes (Figure 1).
Figure 1
Counseling on COVID-19 should also include the benefits of a healthy lifestyle. A healthy diet can improve microvascular dysfunction,17 as is present in COVID-19 infection. Therefore, COVID-19 counseling should emphasize the importance of aggressive lifestyle interventions and improvement of modifiable health behaviors.
Next Steps
Clinics for post-acute care of COVID-19 patients should monitor for CVD. There may be a role for serial clinical exams, electrocardiograms, biomarkers such as troponin, or echocardiograms for patients with persistent cardiac symptoms, such as palpitations, chest pain, and dyspnea.15
Further research is needed to understand how COVID-19 affects long-term risk for CVD, particularly to determine if COVID-19 may be a persistent cardiovascular risk-enhancing factor. Given the endothelial dysfunction seen in both CVD and COVID-19, it is also worthwhile to explore if typical cardiac medications, such as antiplatelet agents or statins, may be beneficial in the acute and post-acute treatment of COVID-19.
Another interesting area of exploration is the risk of thrombosis with COVID-19. Post-mortem examinations have shown venous thromboemboli in patients with COVID-19 despite prophylactic anticoagulation.18 There can be sustained endothelial dysfunction, inflammation, and coagulation activation more than 3 months after acute COVID-19 infection.19 Given the relationship of thromboemboli and pulmonary hypertension, it will be important to determine if microthrombi associated with COVID-19 lead to an increased risk of chronic thromboembolic pulmonary hypertension.
Conclusions
COVID-19 infection increases the risk and severity of CVD in the acute and long-term setting. Clinicians should counsel patients on the risks of CVD to emphasize the importance of primary prevention through vaccination for COVID-19. Further research is needed to understand the pathophysiology of COVID-19 infection and its relationship to endothelial dysfunction.
References
- Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis 2020;20:533–34.
- Gupta A, Madhavan MV, Sehgal K, et al. Extrapulmonary manifestations of COVID-19. Nat Med 2020;26:1017–32.
- Stefanini GG, Montorfano M, Trabattoni D, et al. ST-elevation myocardial infarction in patients with COVID-19: clinical and angiographic outcomes. Circulation 2020;141:2113-16.
- Boehmer TK, Kompaniyets L, Lavery AM, et al. Association between COVID-19 and myocarditis using hospital-based administrative data - United States, March 2020-January 2021. MMWR Morb Mortal Wkly Rep 2021;70:1228-32.
- Guo T, Fan Y, Chen M, et al. Cardiovascular implications of fatal outcomes of patients with Coronavirus Disease 2019 (COVID-19). JAMA Cardiol 2020;5:811-18.
- Ackermann M, Verleden SE, Kuehnel M, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N Engl J Med 2020;383:120-28.
- Xie Y, Xu E, Bowe B, Al-Aly Z. Long-term cardiovascular outcomes of COVID-19. Nat Med 2022;28:583-90.
- Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet 2020;395:1417-18.
- Souilhol C, Serbanovic-Canic J, Fragiadaki M, et al. Endothelial responses to shear stress in atherosclerosis: a novel role for developmental genes. Nat Rev Cardiol 2020;17:52-63.
- Kaur R, Kaur M, Singh J. Endothelial dysfunction and platelet hyperactivity in type 2 diabetes mellitus: molecular insights and therapeutic strategies. Cardiovasc Diabetol 2018;17:121.
- He X, Zeng H, Chen JX. Emerging role of SIRT3 in endothelial metabolism, angiogenesis, and cardiovascular disease. J Cell Physiol 2019;234:2252-65.
- Huertas A, Montani D, Savale L, et al. Endothelial cell dysfunction: a major player in SARS-CoV-2 infection (COVID-19)? Eur Respir J 2020;56:2001634.
- Puntmann VO, Carerj ML, Wieters I, et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from Coronavirus Disease 2019 (COVID-19). JAMA Cardiol 2020;5:1265-73.
- Mitrani RD, Dabas N, Goldberger JJ. COVID-19 cardiac injury: implications for long-term surveillance and outcomes in survivors. Heart Rhythm 2020;17:1984-90.
- Nalbandian A, Sehgal K, Gupta A, et al. Post-acute COVID-19 syndrome. Nat Med 2021;27:601-15.
- Gu SX, Tyagi T, Jain K, et al. Thrombocytopathy and endotheliopathy: crucial contributors to COVID-19 thromboinflammation. Nat Rev Cardiol 2021;18:194-209.
- Millan-Orge M, Torres-Peña JD, Arenas-Larriva A, et al. Influence of dietary intervention on microvascular endothelial function in coronary patients and atherothrombotic risk of recurrence. Sci Rep 2021;11:20301.
- Lax SF, Skok K, Zechner P, et al. Pulmonary arterial thrombosis in COVID-19 with fatal outcome: results from a prospective, single-center, clinicopathologic case series. Ann Intern Med 2020;173:350-61.
- Willems LH, Nagy M, Ten Cate H, et al. Sustained inflammation, coagulation activation and elevated endothelin-1 levels without macrovascular dysfunction at 3 months after COVID-19. Thromb Res 2022;209:106-14.
Clinical Topics: Anticoagulation Management, Arrhythmias and Clinical EP, Cardiovascular Care Team, COVID-19 Hub, Diabetes and Cardiometabolic Disease, Dyslipidemia, Heart Failure and Cardiomyopathies, Noninvasive Imaging, Prevention, Pulmonary Hypertension and Venous Thromboembolism, Stable Ischemic Heart Disease, Anticoagulation Management and Atrial Fibrillation, Anticoagulation Management and Venothromboembolism, Atrial Fibrillation/Supraventricular Arrhythmias, Nonstatins, Novel Agents, Statins, Acute Heart Failure, Heart Failure and Cardiac Biomarkers, Pulmonary Hypertension, Magnetic Resonance Imaging, Diet, Hypertension, Chronic Angina
Keywords: Angiotensin-Converting Enzyme 2, Cardiovascular Diseases, COVID-19, COVID-19 Vaccines, SARS-CoV-2, Hydroxymethylglutaryl-CoA Reductase Inhibitors, Platelet Aggregation Inhibitors, ST Elevation Myocardial Infarction, Endothelial Cells, Atrial Fibrillation, Brain Ischemia, Diet, Healthy, Hyperlipidemias, Hypertension, Pulmonary, Pandemics, Postural Orthostatic Tachycardia Syndrome, Public Health, Stroke Volume, Subacute Care, Tachycardia, Sinus, Venous Thromboembolism, Risk Factors, Stroke, Atherosclerosis, Inflammation, Biomarkers, Heart Disease Risk Factors, Magnetic Resonance Imaging, Cardiovascular System, Intensive Care Units, Electrocardiography, Primary Prevention, Ischemic Stroke, Anticoagulants, Catecholamines, Heart Failure, Adrenergic Agents, Chest Pain, Counseling, Delivery of Health Care, Thrombosis, Apoptosis, Cytokines, Troponin, Diabetes Mellitus, Dyspnea, Fibrosis, Obesity
< Back to Listings