Implementing a Fontan Management Program
Quick Takes
- Patients with Fontan circulation are at increased risk for cardiac and extracardiac morbidities that lead to early mortality.
- A collaborative multidisciplinary approach may result in early detection of comorbidities, standardization of care, and may improve outcomes.
Background:
The Fontan operation has resulted in a significant improvement in the survival of patients with single ventricle congenital heart disease (CHD).1 Today, a generation of Fontan patients who benefited from improvement in surgical techniques as well as post-operative intensive and general cardiac care are now reaching adolescence and adulthood.2 There are at least 70,000 patients with a Fontan circulation worldwide, and the number is increasing.1 This unique physiology results in chronic elevation in central venous pressure and low cardiac output,3 resulting in co-morbidities, multi-organ involvement and increased mortality1,4 higher than in any other form of CHD.5 Multi-organ involvement and high mortality has led many centers to form multidisciplinary Fontan management programs with a focus on early detection and proactive management.6 We briefly discuss the risks associated with Fontan circulation and offer suggestions that may improve multidisciplinary management for these patients.
Table 1
| Morbidity | Brief description |
| Cardiac1 | Systolic and diastolic dysfunction, atrioventricular valve regurgitation, Fontan pathway obstruction, tachy- and bradyarrhythmias, cyanosis, Fontan circulatory failure affecting activities of daily living. |
| Liver disease7 | Fontan-associated liver disease includes varying degrees of hepatic fibrosis, compensated and decompensated cirrhosis, focal nodular hyperplasia, and neoplastic hepatocellular malignant and benign lesions. Portal hypertension, likely related to elevated Fontan pressure, is common. |
| Lymphatic insufficiency8 | Protein‐losing enteropathy, plastic bronchitis, ascites, or pleural effusion. |
| Lung disease1 | Plastic bronchitis, varying degrees of restrictive and obstructive lung disease, sleep apnea and elevated pulmonary vascular resistance. |
| Kidney disease9 | Chronic kidney disease in approximately 10%, decreased glomerular filtration rate, proteinuria, albuminuria. |
| Growth and physical developmental abnormalities1 | Short stature, decreased vitamin D levels, overweight, obesity, and decreased bone density. |
| Brain and psychosocial abnormalities1 | Neurodevelopmental abnormalities, learning disabilities, social challenges, mood, and anxiety disorders. |
| Unique adult issues1 | Contraception, pregnancy, employment, transition to adult congenital specialist and adult care, and insurance challenges. |
Current Status: Currently, a pediatric or adult cardiologist with training in CHD provides the care for the adolescent and adult with a Fontan circulation. Screening for multi-organ involvement is performed by the cardiologist who must be up to date with protocols. When multi-organ involvement develops, the patient is then referred to subspecialists who may not be familiar with Fontan related co-morbidities as it pertains to their subspecialty. Additionally, this approach may result in late detection or referral and fragmented care. The incidence of post Fontan morbidity peaks in the peri-operative period and then increases again in adolescence and early adulthood. Thus, it is important to detect extra-cardiac co-morbidities to improve both cardiac and non-cardiac status in older children and adult Fontan patients.6
Proposed Solutions:
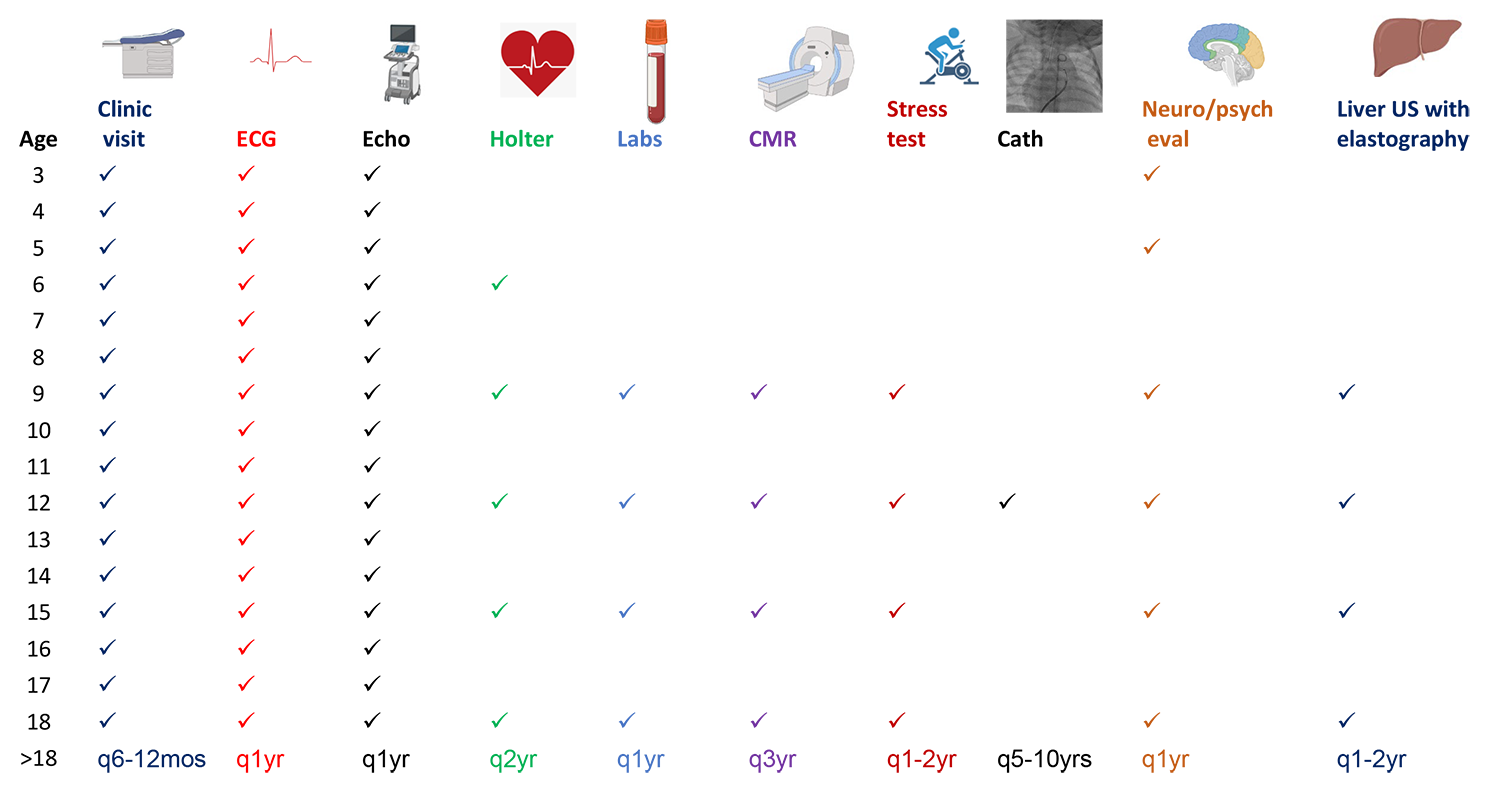
- To address late detection and delayed referral to appropriate subspecialists, "screening protocols " are important (Tables 2,3). These are best tailored to fit institutional preferences and expertise. The frequency for surveillance testing for cardiovascular and end-organ system involvement is age dependent, becoming more frequent during adolescence and adulthood.1
- To address the potential for fragmented care of Fontan patients, some programs have instituted multidisciplinary Fontan management clinics where the patient sees multiple specialists in a single day in one clinic space.
- Another approach is to foster "Fontan champions" from other clinical subspecialties who become familiar with the extra cardiac involvement associated with this unique circulation and allow multi-disciplinary evaluation at different times and locations. This may simplify challenges associated with co-locating all the sub-specialists to one clinic space.
- Some programs have begun multidisciplinary meetings where different specialists with interest and expertise in the Fontan circulation regularly discuss each patient. The patients will then see the specialists in person or virtually. This set-up aims to improve inter-specialty communication to achieve individualized care for each patient.
Current Challenges:
A combined clinic with all the specialists present in one space is resource-intensive. This may be over-come with the use of telehealth visits. Despite multidisciplinary care, the best care model is yet to be determined. Patient experience, cost, and testing safety should be taken into consideration and an individualized patient-centric approach is essential to identify those at elevated risk for severe multiorgan involvement, malignancy, or worsening cardiac status who may benefit from more invasive testing.
Table 2
| Age (yr) | ECG | Echo | Cardiac MRI/CT | Holter | Cardiac Cath | Liver ultrasound elastography | Quality of life assessment+ | Pulmonary function test | Multi-disciplinary evaluation | Labs† | Cardiopulmonary exercise test |
| Below 12 | q1yr | q1yr | One time | q3yr | One time* | One time | One time | As needed | q5yr | One time | One time |
| >12 | q1yr | q1yr | q3yr | q3yr | q10 yr | q2yr | q1yr | Baseline | q5yr | q2yr | q2yr |
| >18 | q1yr | q1yr | q3yr | q2yr | q5-10 yr | q1-2yr | q1yr | q3-5 yr | q1-2yr | q1yr | q1-2yr |
*Encouraged based on the primary cardiologist for baseline hemodynamic assessment.
† Labs may include: complete blood count, basic metabolic profile, hepatic function panel, coagulation studies, Vitamin D, TSH, cystatin C, alpha fetoprotein, brain natriuretic peptide, stool alpha1 antitrypsin, iron studies and lipid profile.
Yr: year; ECG: electrocardiogram; Echo: echocardiogram; MRI: magnetic resonance imaging; CT: computed tomography.
Table 3
Conclusion
The population of Fontan patients is growing, with a concomitant increase in their health care needs to address extra-cardiac co-morbidities requiring multidisciplinary care. To meet this growing need, we propose the institution of multidisciplinary clinics for Fontan patients. At the very least, "Fontan champions", subspecialists with interest in and who have gained familiarity with the unique aspects of the Fontan circulation, must be available to help manage these complex patients. Appropriate screening, with inter-specialty communication and collaboration, may improve access to health care and improve overall outcomes in this growing population.
References
- Rychik J, Atz AM, Celermajer DS, et al. Evaluation and management of the child and adult with Fontan circulation: a scientific statement from the American Heart Association. Circulation 2019:Jul 1:[Epub ahead of print].
- Alsaied T, Bokma JP, Engel ME, et al. Factors associated with long-term mortality after Fontan procedures: a systematic review. Heart 2017;103:104-10.
- Gewillig M, Brown SC. The Fontan circulation after 45 years: update in physiology. Heart 2016;102:1081-86.
- Gewillig M, Brown SC, van de Bruaene A, Rychik J. Providing a framework of principles for conceptualising the Fontan circulation. Acta Paediatr 2020;109:651-58.
- Diller GP, Kempny A, Alonso-Gonzalez R, et al. Survival prospects and circumstances of death in contemporary adult congenital heart disease patients under follow-up at a large tertiary centre. Circulation 2015;132:2118-25.
- Lubert AM, Alsaied T, Trout AT, et al. Developing an adolescent and adult Fontan management programme. Cardiol Young 2022;32-230-35.
- Alsaied T, Rathod RH, Aboulhosn JA, et al. Reaching consensus for unified medical language in Fontan care. ESC Heart Fail 2021;8:3894-3905.
- Kreutzer C, Kreutzer G. The lymphatic system: the Achilles Heel of the Fontan-Kreutzer circulation. World J Pediatr Congenit Heart Surg 2017;8:613-23.
- Zafar F, Lubert AM, Katz DA, et al. Long-term kidney function after the Fontan operation: JACC Review Topic of the Week. J Am Coll Cardiol 2020;76:334-41.
Clinical Topics: Arrhythmias and Clinical EP, Cardiac Surgery, Congenital Heart Disease and Pediatric Cardiology, Dyslipidemia, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Implantable Devices, Cardiac Surgery and Arrhythmias, Cardiac Surgery and CHD and Pediatrics, Cardiac Surgery and Heart Failure, Congenital Heart Disease, CHD and Pediatrics and Arrhythmias, CHD and Pediatrics and Imaging, CHD and Pediatrics and Interventions, CHD and Pediatrics and Prevention, CHD and Pediatrics and Quality Improvement, Lipid Metabolism, Heart Failure and Cardiac Biomarkers, Interventions and Imaging, Interventions and Structural Heart Disease, Computed Tomography, Echocardiography/Ultrasound, Magnetic Resonance Imaging, Nuclear Imaging, Sleep Apnea
Keywords: Fontan Procedure, Pregnancy, Quality of Life, Activities of Daily Living, Cystatin C, Natriuretic Peptide, Brain, alpha-Fetoproteins, Exercise Test, Albuminuria, Anxiety Disorders, Ascites, Bone Density, Bradycardia, Carcinoma, Hepatocellular, Cardiac Output, Low, Central Venous Pressure, Elasticity Imaging Techniques, Focal Nodular Hyperplasia, Glomerular Filtration Rate, Protein-Losing Enteropathies, Liver Neoplasms, Heart Defects, Congenital, Magnetic Resonance Imaging, Vascular Resistance, Lung Diseases, Obstructive, Renal Insufficiency, Chronic, Health Services Accessibility, Blood Cell Count, Learning Disabilities, Hypertension, Portal, Electrocardiography, Metabolome, Patient Outcome Assessment, Pleural Effusion, Liver Cirrhosis, Patient-Centered Care, Sleep Apnea Syndromes, Bronchitis, Telemedicine, Tomography, Vitamin D, Cyanosis, Kidney, Lipids, Thyrotropin, Tomography, X-Ray Computed
< Back to Listings