Comparing Guideline Recommendations of Statin Use For the Primary Prevention of ASCVD
Quick Takes
- Implementation of the 2022 USPSTF guideline for statin therapy for primary prevention would reduce the opportunity for ASCVD risk reduction in a large number of adults who would likely benefit from statin initiation, particularly in younger adults and those with diabetes mellitus.
- Traditional ASCVD risk calculations may underestimate risk in younger patients who do not meet defined thresholds for statin initiation.
Introduction
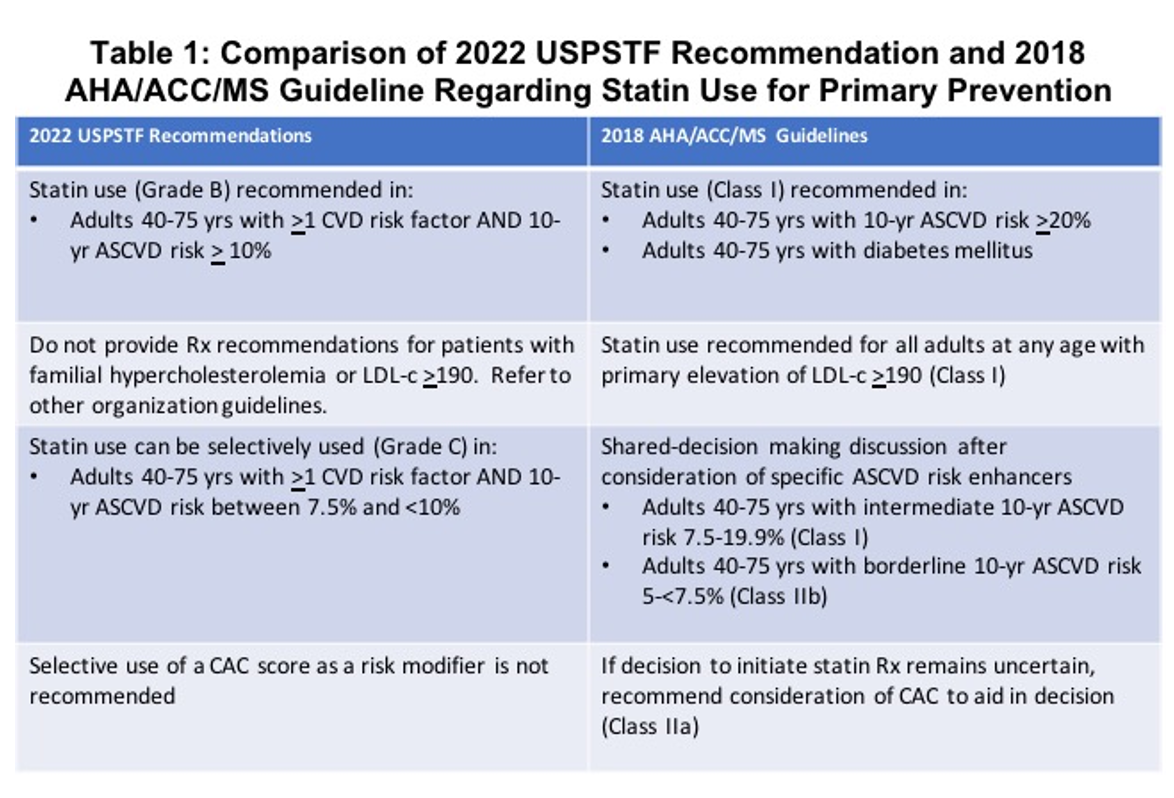
The United States Preventative Services Taskforce (USPSTF) recently released its guidance for the use of statin therapy in primary prevention of atherosclerotic cardiovascular disease (ASCVD). Their guideline recommends statin therapy for adults aged 40-75 with ≥1 CVD risk factor (hypertension, dyslipidemia, diabetes, smoking) and calculated 10-year ASCVD risk of ≥10% (Grade B).1
The 2018 American Heart Association/American College of Cardiology/Multisociety (AHA/ACC/MS) guideline recommends statin therapy for primary prevention in adults with low density lipoprotein-cholesterol (LDL-C) >190mg/dL (Class 1), those aged 40-75 years with diabetes mellitus irrespective of ASCVD risk (Class 1), and those aged 40-75 years with 10-year ASCVD risk ≥20% (Class 1).2 They further recommend consideration of additional risk enhancers and emphasize shared decision making in the decision to initiate statin therapy in patients with borderline (5 to <7.5%) and intermediate (7.5% to <20%) 10-year ASCVD risk (Class 2b and Class 1, respectively).2
In a recently published study,3 Gupta et al. utilized National Health and Nutrition Examination Survey (NHANES) data to predict the proportion and absolute number of US adults who would be eligible for statin therapy for primary prevention under the 2022 USPSTF guideline compared to the 2018 AHA/ACC/MS guideline.
We aim (1) to summarize the results presented in Gupta et al.'s study and (2) to discuss the major differences between the USPSTF and AHA/ACC/MS recommendations accounting for the discrepancy in the number of adults eligible for statin initiation with implementation of the respective guidelines.
Summary and Results
Eligible participants (n=1,799) were non-pregnant adults aged 40-75 years with LDL-C <190 mg/dL and no self-reported ASCVD from NHANES (2017-2020). The 10-year ASCVD risk was calculated using pooled cohort equations irrespective of current statin therapy. Participants were considered eligible for statin therapy per USPSTF guidelines if 10-year ASCVD risk was ≥10% and ≥1 CVD risk factor was present, and eligible per AHA/ACC/MS guidelines if they had diabetes mellitus or if 10-year ASCVD risk was ≥7.5%. Fasting subsample weighted proportions were extrapolated to the US population to predict the absolute number of adults who would be eligible for statin therapy according to the respective guidelines.
Utilizing the USPSTF recommendations, 31.8% (95% CI 28.6-35.1%) of participants were eligible for statin initiation for primary prevention representing 33.7 million US adults. This was in comparison to 46.8% of participants, representing 49.7 million US adults, who were eligible per the 2018 AHA/ACC/MS guidelines.
In participants aged 40-55 years, 8.3% and 21.2% were eligible for statin initiation per the USPSTF and AHA/ACC/MS guidelines, respectively. In participants aged 56-75 years, 54.4% and 71.4% (66.3, 76.0) were eligible for statin initiation, respectively.
In regard to participants with diabetes mellitus, 63% met eligibility criteria under the USPSTF recommendations (compared to all participants under the AHA/ACC/MS guideline). Participants with diabetes mellitus who were not eligible per USPSTF recommendations were younger (mean age 50.9 years ± 0.8) and had a shorter duration of diabetes mellitus (mean duration 6.7 years ± 0.6) as compared to those who were eligible.
Perspective
The above results indicate that implementation of the 2022 USPSTF guidelines, as compared to the 2018 AHA/ACC/MS guidelines, would greatly reduce the number of adults eligible for statin therapy for primary prevention. Importantly, both younger patients 40-55 years and those with diabetes mellitus are much less likely to be eligible for statin initiation per the USPSTF guidelines.
Only 8.3% of participants aged 40-55 years were eligible for statin initiation per the USPSTF guidelines. These participants did not meet the ASCVD risk threshold of ≥10% per the USPSTF guidelines, as age has the highest relative contribution in ASCVD risk calculation. Furthermore, all participants with diabetes mellitus qualified for statin therapy under AHA/ACC/MS guidelines, but only those with ASCVD risk ≥10% qualified under USPSTF guidelines. This accounts for the >2-fold difference in eligible proportions observed in the younger cohort of participants. Irrespective of age, a striking 37% of participants with diabetes mellitus aged 40-75 years were eligible for statin initiation per the AHA/ACC/MS guideline but not the USPSTF guideline.
These results are consistent with a previously published study using NHANES data to compare the 2016 USPSTF and 2013 AHA/ACC recommendations for statin initiation in primary prevention. Their results indicated that younger adults and persons with diabetes mellitus accounted for the majority of individuals who were recommended for statin therapy under the AHA/ACC guidelines but not the USPSTF guidelines.4
The higher ASCVD risk threshold recommended by the USPSTF disproportionately reduces the number of younger adults eligible for statin therapy who may be at risk for ASCVD. Age is the dominant factor in the pooled cohort equations and, thus, it is more difficult for younger patients to cross the ≥10% threshold per USPTSF guidelines.2,5
Prior NHANES data from 2005-2010, however, suggests that half of all cardiovascular events in men and one-third in women occur before the age of 65.6 Further studies have shown that even an ASCVD risk threshold of ≥7.5% may have a low sensitivity for capturing 10-year ASCVD risk in younger populations.5,7,8 Thus, reliance on calculated ASCVD risk alone may frequently underestimate risk, especially in younger individuals whose calculated scores may not meet defined thresholds for initiation of statin therapy.
The 2018 AHA/ACC/MS guideline recommends the assessment of risk enhancers when considering statin therapy for patients with borderline and intermediate 10-year ASCVD risk (5 to <20%, respectively). The use of risk enhancers, stable characteristics that indicate increased risk over the life course, allows for a qualitative assessment of individual risks to complement the quantitative ASCVD risk calculation.2,8
The AHA/ACC/MS guideline supports the selective use of coronary artery calcium (CAC) scoring to reclassify risk accurately to aid in the decision of statin initiation in patients with a borderline or intermediate ASCVD risk.2,8 With the use of risk enhancers and CAC scoring, the AHA/ACC/MS guideline allows for a more individualized cardiovascular risk assessment to guide statin initiation as opposed to reliance on the calculated ASCVD risk alone.
One limitation of Gupta et al.'s analysis was the inability to account for individualized risk assessment and shared decision making when determining eligibility for statin initiation. All participants with a calculated 10-year ASCVD risk of ≥7.5% were considered eligible. Thus, it is likely that their results underestimate the number of US adults that would be eligible for statin initiation per the AHA/ACC/MS guideline, as a number of participants with borderline risk (10-year ASCVD of 5% to <7.5%) may have been considered eligible after consideration of risk enhancers and/or CAC scoring.
The incidence of ASCVD events is markedly increased in patients with diabetes mellitus and the occurrence of a first ASCVD event in patients with diabetes mellitus is associated with increased morbidity and mortality.2,9 With an increasing number of adults being diagnosed with diabetes mellitus at a younger age, it is imperative that these patients be recommended to take statin therapy in a timely fashion.
Participants with diabetes mellitus who were not eligible for statin therapy per the USPSTF guidelines were younger, with a mean duration of diabetes mellitus of approximately 7 years. Implementation of the USPSTF guidelines would potentially withhold treatment from a large number of adults who would benefit from earlier ASCVD risk reduction efforts.
Conclusions
As compared to the 2018 AHA/ACC/MS guideline, implementation of the 2022 USPSTF guideline for statin therapy for primary prevention would reduce the opportunity for ASCVD risk reduction in a large number of adults who would likely benefit from statin initiation, particularly in younger adults and those with diabetes mellitus.
Table 1
References
- Chou R, Cantor A, Dana T, et al. Statin use for the primary prevention of cardiovascular disease in adults: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA 2022;328:754-71.
- Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines J Am Coll Cardiol 2019;73:3168-3209.
- Gupta K, Kakar TS, Jain V, et al. Comparing eligibility for statin therapy for primary prevention under 2022 USPSTF recommendations and the 2018 AHA/ACC/multi-society guideline recommendations: from National Health and Nutrition Examination Survey. Prog Cardiovasc Dis 2022;Aug 26:[Epub ahead of print].
- Pagidipati NJ, Navar AM, Mulder H, Sniderman AD, Peterson ED, Pencina MJ. Comparison of recommended eligibility for primary prevention statin therapy based on the US Preventive Services Task Force recommendations vs the ACC/AHA guidelines. JAMA 2017;317:1563-67.
- Navar-Boggan AM, Peterson ED, D'Agostino RB Sr, Pencina MJ, Sniderman AD. Using age-and sex-specific risk thresholds to guide statin therapy: one size may not fit all. J Am Coll Cardiol 2015;65:1633-39.
- Sniderman AD, Thanassoulis G, Williams K, Pencina M. Risk of premature cardiovascular disease vs the number of premature cardiovascular events. JAMA Cardiol 2016;1:492-94.
- Zeitouni M, Nanna MG, Sun JL, Chiswell K, Peterson ED, Navar AM. Performance of guideline recommendations for prevention of myocardial infarction in young adults. J Am Coll Cardiol 2020;76:653-64.
- Stone NJ, Greenland P, Grundy SM. Statin usage in primary prevention—comparing the USPSTF recommendations with the AHA/ACC/Multisociety guidelines. JAMA Cardiol 2022;Aug 23:[Epub ahead of print].
- de Vries FM, Denig P, Pouwels KB, Postma MJ, Hak E. Primary prevention of major cardiovascular and cerebrovascular events with statins in diabetic patients. Drugs 2012;72:2365-73.
Clinical Topics: Cardiovascular Care Team, Diabetes and Cardiometabolic Disease, Dyslipidemia, Prevention, Lipid Metabolism, Nonstatins, Novel Agents, Statins, Diet, Hypertension, Smoking
Keywords: Hydroxymethylglutaryl-CoA Reductase Inhibitors, Cardiovascular Diseases, Cholesterol, LDL, American Heart Association, Nutrition Surveys, Calcium, Fasting, Coronary Vessels, Decision Making, Shared, Life Change Events, Risk Factors, Heart Disease Risk Factors, Primary Prevention, Dyslipidemias, Risk Assessment, Diabetes Mellitus, Risk Reduction Behavior, Hypertension, Smoking
< Back to Listings