ACC, AHA Release First-Ever Guideline For Treatment and Management of Acute PE
The new ACC/AHA Guideline for the Evaluation and Management of Acute Pulmonary Embolism (PE) in Adults is a de novo document offering comprehensive, evidence‑based recommendations for the evaluation, management and follow‑up of adults with acute PE. Collaborated on and endorsed by an additional eight societies, the new guideline recognizes that management of patients with acute PE "is uniquely multidisciplinary and crosses emergency department, inpatient settings and outpatient clinics."
Central to the new guideline is the creation of five "Acute PE Clinical Categories" (A-E) and subcategories that provide a framework designed to define the severity of an acute PE, improve prognostic accuracy, and guide therapeutic decision‑making across the acute and early post‑acute phases of care.
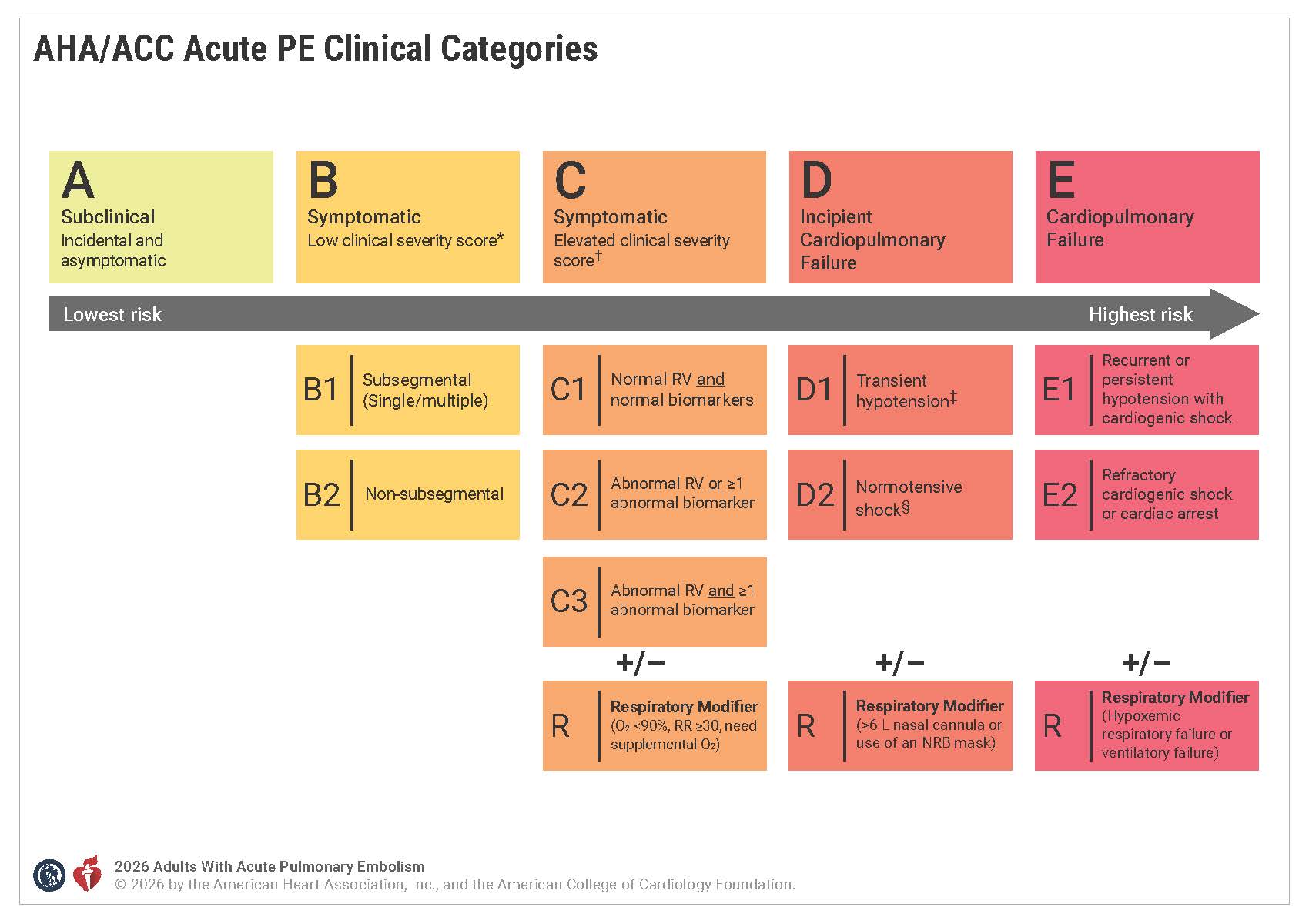
For example, individuals who fall under Category A (subclinical) can safely be discharged home from the emergency room without hospitalization, while those in Category B (symptomatic/low clinical severity) can generally be discharged early. Symptomatic patients with elevated clinical severity scores (Categories C-E) should be hospitalized in order to optimize treatment strategies that could include anticoagulation therapy or advanced therapies like systemic thrombolysis, catheter-based thrombolysis, mechanical thrombectomy and surgical embolectomy depending on the category and level of risk.
When it comes to anticoagulation guidance, low-molecular-weight heparin is recommended over unfractionated heparin in patients with acute PE requiring initial parenteral anticoagulant therapy. In patients deemed eligible for oral anticoagulation, direct oral anticoagulants are recommended over vitamin K antagonists, unless contraindicated, to minimize major bleeding and to prevent recurrent venous thromboembolism. Additionally, continuation of anticoagulation treatment beyond the initial three- to six-month treatment phase is recommended in patients experiencing their first acute PE without a major reversible risk factor and/or in patients with a persistent risk factor.
In other highlights, the guideline includes additional risk factors, and notes that "during a targeted history and physical examination, assessment for PE risk factors should include recent surgery, hospitalization for medical therapy, immobility, pregnancy, estrogens, trauma, cancer, inflammatory disorders, and inherited and acquired thrombophilias, among others." Other risk factors, which may vary by sex, include atherosclerotic cardiovascular disease, pulmonary disease, cancer, chronic venous disease, prolonged immobility, and hormonal therapy.
The importance of PE response teams (PERTs) in improving timeliness of care is also a focus. According to the guideline, representatives from vascular medicine, pharmacy, nursing, emergency medicine, cardiac surgery, etc., as well as the patient and/or family members, are all potential PERT members. According to the authors, the diversity of insights and roles associated with a PERT can help with risk stratification, selection and implementation of advanced therapies, navigation of gaps in evidence, as well as improve follow-up care and clinician education, among other benefits.
As is customary with all guidelines, a section outlining where significant evidence gaps persist across multiple domains of care is also included. The authors note that "refining risk stratification tools – such as validating the ACC/AHA clinical categories and integrating novel predictors like thrombus burden and [right ventricular] enlargement metrics – to better guide therapeutic decisions" are among the challenges that need to be addressed going forward.
"There have been significant advances in the understanding of pulmonary embolism and treatments to effectively manage this condition," said Writing Committee Chair Mark A. Creager, MD, FACC. "This guideline is a road map to help clinicians navigate these advances for the safest and most effective approaches to care for people with this condition."
Clinical Topics: Anticoagulation Management, Cardiac Surgery, Invasive Cardiovascular Angiography and Intervention, Pulmonary Hypertension and Venous Thromboembolism, Vascular Medicine, Anticoagulation Management and Venothromboembolism, Interventions and Vascular Medicine
Keywords: Thrombolytic Therapy, Embolectomy, Catheters, Thrombosis, Lung Diseases, Emergency Medicine, Thrombectomy, Thrombophilia, Heparin, Low-Molecular-Weight, Pulmonary Embolism, Neoplasms, Anticoagulants, Venous Thromboembolism, Heparin, Pregnancy
< Back to Listings
