Feature | Educational Needs in Cardio-Oncology

There has been a rapid growth in the field of cardio-oncology over the last several years, including an emerging focus on this topic by the ACC and other cardiology societies. This is in large part driven by advances in cancer treatment with increasing longevity in the oncologic population. Currently, there are an estimated 15.5 million cancer survivors in the U.S. with projected growth to more than 20 million by 2026 , contributing to a large at-risk cohort for downstream post-chemotherapy and post-radiation cardiotoxicity.
In 2015, Ana Barac, MD, PhD, FACC, et al., conducted an ACC survey of 444 adult and pediatric cardiology division chiefs and cardiovascular fellowship program directors and identified several gaps:
- Sixty-five percent felt that access to cardio-oncology specialists would improve care for patients with cardiotoxicity, yet only 27 percent of centers reported having an established cardio-oncology service.
- Thirty-nine percent of respondents were not confident with providing cardiovascular care to cancer patients, averaging 2.5 out of 5.0 for level of understanding.
- Seventy percent of respondents felt educational training materials would be beneficial, but with 43 percent of programs having no training in cardio-oncology and another 43 percent having exposure limited to usual cardiology rotations.
With the development and recognition of cardio-oncology as an emerging field, learning materials are evolving and becoming more available. Continued growth has been evident by the ongoing development of the ACC Cardio-Oncology Section, multiple consensus statements and review articles (posted at the end of this article), dedicated seminars and conferences including the annual ACC Cardio-oncology Symposium. Despite this, there remains a lack of consolidated resources common to other specialties.
Many centers have burgeoning cardio-oncology programs yet there remains an unmet need for structured training in the field and ongoing clarification of what determines adequate knowledge and skills for a full-fledged cardio-oncologist. There have been published proposals for cardio-oncology training including from leaders in the field and a formal proposal from the ICOS and Canadian Cardiac Oncology Network. These highlighted critical aspects of training including the incorporation of COCATS 4 and its associated training levels.
We seek to highlight key educational training needs for cardiology fellows and early career providers in the field of cardio-oncology. This article is not intended to be a comprehensive outline of how to develop a fellowship, which has previously been described in the above referenced literature.
A hallmark of an effective training program includes proper identification and training in key skillsets that are critical for efficient clinical care, development of an in-depth understanding of active problems in the field with recognition of gaps in knowledge, and translation of these questions into research opportunities. One critical precursor to strong cardio-oncology training is a well-supported program with dedicated faculty to ensure adequate volume and sustainability. Additionally, a strong collaborative relationship between an institution’s cardiac and cancer programs in regard to multidisciplinary patient care and research is essential to the success of its cardio-oncology program.
A common question from fellows is what particular skills they might gain from time spent in a cardio-oncology fellowship. As training requirements have become prolonged (dedicated training for heart failure [HF], two-year programs for electrophysiology and adult congenital heart disease, sequential structural or vascular years after interventional), fellows are increasingly attuned to maximizing time spent in training. This will be an important stepping stone for cardio-oncology to develop into a competitive subspecialty fellowship. Current skills specific to cardio-oncologists include but are not limited to the following:
- Knowledge/Patient Care: Comprehensive understanding of potential for cardiotoxicity from specific chemotherapy regimens is built upon core knowledge from internal medicine and general cardiology training. Other knowledge areas include concerns before and during cancer treatment, how to minimize and treat cardiovascular complications, and a fundamental grasp of cancer progression and mechanism of action for associated treatments. The initial proposal is that approximately 100 unique patient visits during the year would be needed to gain desired competence.
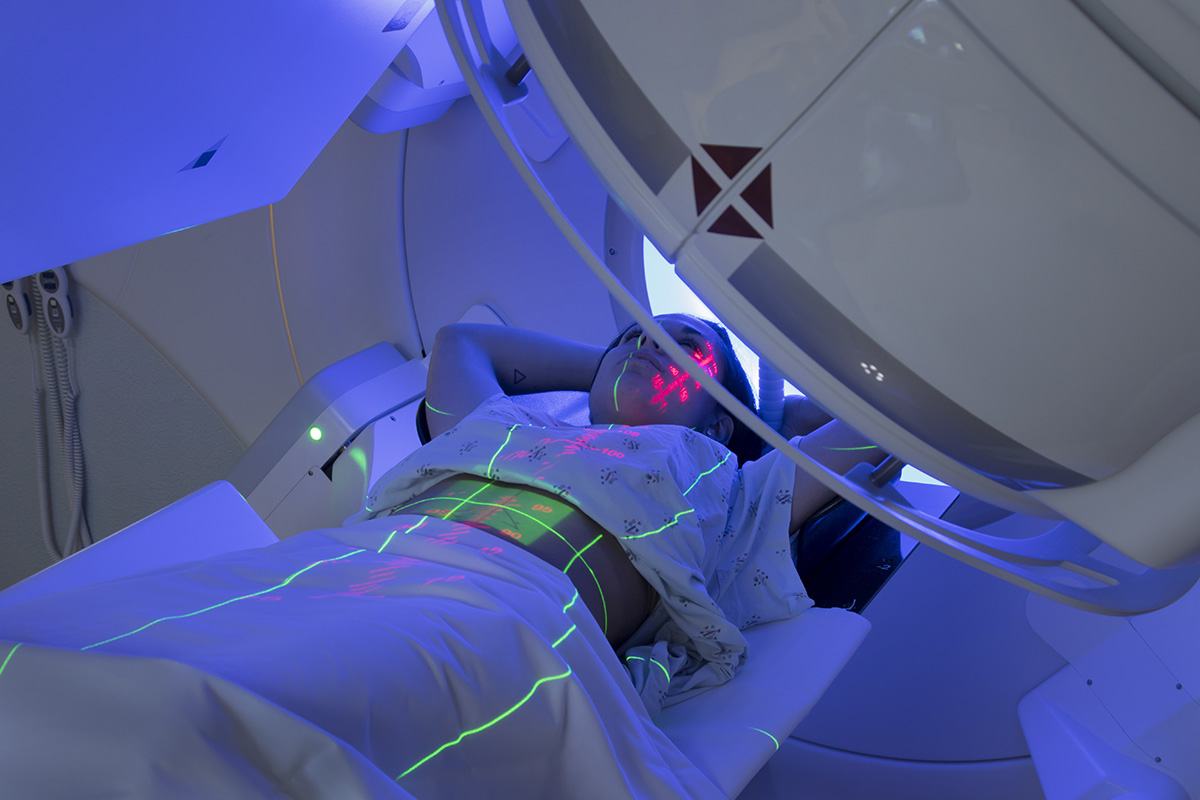
- Imaging: Cardio-oncology integrates a strong focus on cardiac imaging, including advanced modalities such as strain imaging, 3-D and valvular assessment with echocardiography, cardiac magnetic resonance imaging and vascular imaging. These are critical in the evaluation for cardiotoxicity.
- Procedural: Currently, there are no specific procedures performed by cardio-oncologists, with the exception of increased focus on advanced cardiac imaging. Although this aspect of cardiac care is relatively underexplored compared to imaging, the trainee should be exposed to invasive diagnostic and interventional treatments including cardiac catheterization for hemodynamic assessment of pericardial/restrictive disease, angiography and fractional flow reserve/intravascular ultrasound/optical coherence tomography for vasculotoxic manifestations of treatment. Trainees should also learn to manage and balance hematologic derangements and ischemic sequelae (i.e. accelerated atherosclerosis, acute coronary syndrome) both pharmacologically and with percutaneous coronary/valvular interventions.
- Electrophysiology: Chemoradiation therapies are known to cause arrhythmogenic sequelae (i.e. ibrutinib causing atrial fibrillation). Trainees can evaluate both noninvasive (i.e. exercise testing, ambulatory rhythm monitoring, autonomic reflex screening) and invasive (i.e. electrophysiologic invasive testing and/or ablation) diagnostic modalities in evaluating for and treating arrhythmias related to cancer treatments.
- Research: There are abundant opportunities for clinical and translational research in cardio-oncology to understand biologic pathways of cancer agents and associated risk of cardiotoxicity, cardioprotective strategies and treatment for patients with overt cardiac complications.

The initial advanced cardio-oncology training proposal recognized that not all cardio-oncologists come from a cardiology background, and that there may be oncologists who seek advanced training in cardio-oncology. Similar to general cardiology fellows who desire additional training, a critical question is figuring out what additional skills an oncologist would gain in that extra year. Extra training should translate to a more in-depth understanding of how to manage these complex patients while balancing risk of cancer progression with potential for worsening or repeated cardiac complications. Perspectives for different manifestations of cardiotoxicity may vary depending on degree of training and underlying specialty. Such major types of cardiotoxicity include:
Cardiomyopathy/Myocarditis
One of the more common presentations from cardiotoxicity in the acute setting. Severity can range from asymptomatic left ventricular (LV) dysfunction to cardiogenic shock.
- General cardiologist: Guideline-directed management of acute decompensated HF; may lack the in-depth knowledge of related chemotherapy toxicity.
- Oncologist: In-depth understanding of cancer treatment and consequences of holding or changing chemotherapy; lacks in-depth knowledge on management of HF and may not fully comprehend the extent of association of chemotherapy with cardiac complications.
- Cardio-oncologist: A dedicated specialist can make the determination on whether the presentation was directly related to recent cancer treatment; fully considers the benefits and drawbacks of holding or switching chemotherapy agents from both the oncology and cardiac standpoints.
- Sub-specialist (HF): Understands detailed management for LV dysfunction and advanced options in cases of cardiogenic shock.
Arrhythmias
Presentation can be variable, with atrial fibrillation common with specific agents including ibrutinib and increased risk of ventricular tachycardia with certain tyrosine kinase inhibitors for chronic myelogenous leukemia.
- Oncologist: In-depth understanding of what alternative cancer treatments may be possible; limited knowledge regarding management of arrhythmias.
- Cardio-oncologist: Clarify whether specific arrhythmia is associated with cancer therapy and risk/benefit ratio of continuing current regimen and balancing risks and benefits of anticoagulation; management of most arrhythmias.
- Sub-specialist (Electrophysiology): Complex management of arrhythmias and consideration for non-pharmacologic approaches such as devices or ablation.
Coronary artery disease (CAD)/ischemia
- Oncologist: Understand options for avoiding future exposure to class effects of cancer treatment that may predispose to ischemia.
- Cardio-oncologist: Recognize which agents may increase risk of both short and long-term development of atherothrombosis-ischemia and how to minimize risk, balancing risk and benefit from both an oncology and cardiac standpoint.
- Sub-specialist (Interventional): Evaluation for extent of CAD and percutaneous intervention when indicated.
Pericardial disease
- Oncologist: Assists in cases of acute pericardial disease by altering culprit chemotherapy or radiation therapy; less likely to participate in long-term management.
- Cardio-oncologist: Recognition and management of acute and long-term pericardial complications related to cancer treatment including acute pericarditis and constriction. Works collaboratively with oncology to minimize future risk of recurrence or worsening of disease.
- Sub-specialist (HF): Confirm diagnosis of significant pericardial disease by imaging and/or invasive catheterization, particularly in cases of constriction; explores potential treatment strategies such as pericardiectomy if indicated.
Long-term cardiovascular health
- Oncologist: Shared understanding of long-term effects of chemotherapy on cardiovascular risk with cardiology.
- Cardio-oncologist: Primary role in aggressive cardiac risk factor reduction, particularly in patients who received high-risk chemotherapy regimens or high mean heart-dose of radiotherapy.
These are exciting times for the field of cardio-oncology with innumerable developments in screening and prevention, diagnostic and treatment modalities, and clinical and translational research. It is essential that we provide a dedicated learning environment for our fellows that parallels the rapidly expanding focus on cardiotoxicity of cancer treatment.
Consensus Statements and Review Articles
Armenian SH, Lacchetti C, Barac A et al. Prevention and Monitoring of Cardiac Dysfunction in Survivors of Adult Cancers: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol 2017;35:893-911.
Plana JC, Galderisi M, Barac A et al. Expert consensus for multimodality imaging evaluation of adult patients during and after cancer therapy: a report from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 2014;27:911-39.
Virani SA, Dent S, Brezden-Masley C et al. Canadian Cardiovascular Society Guidelines for Evaluation and Management of Cardiovascular Complications of Cancer Therapy. Can J Cardiol 2016;32:831-41.
Hamo CE, Bloom MW, Cardinale D et al. Cancer Therapy-Related Cardiac Dysfunction and Heart Failure: Part 2: Prevention, Treatment, Guidelines, and Future Directions. Circ Heart Fail 2016;9:e002843.
Bloom MW, Hamo CE, Cardinale D et al. Cancer Therapy-Related Cardiac Dysfunction and Heart Failure: Part 1: Definitions, Pathophysiology, Risk Factors, and Imaging. Circ Heart Fail 2016;9:e002661.
Zamorano JL, Lancellotti P, Rodriguez Munoz D et al. 2016 ESC Position Paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for Practice Guidelines: The Task Force for cancer treatments and cardiovascular toxicity of the European Society of Cardiology (ESC). Eur Heart J 2016;37:2768-2801.
Chang HM, Okwuosa TM, Scarabelli T, Moudgil R, Yeh ETH. Cardiovascular Complications of Cancer Therapy: Best Practices in Diagnosis, Prevention, and Management: Part 2. J Am Coll Cardiol 2017;70:2552-2565.
Chang HM, Moudgil R, Scarabelli T, Okwuosa TM, Yeh ETH. Cardiovascular Complications of Cancer Therapy: Best Practices in Diagnosis, Prevention, and Management: Part 1. J Am Coll Cardiol 2017;70:2536-2551.
Denlinger CS, Sanft T, Baker KS et al. Survivorship, Version 2.2017, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 2017;15:1140-1163.

This article was authored by Richard K. Cheng, MD, FACC, cardiologist at the University of Washington Medical Center in Seattle, WA, and Eric H. Yang, MD, FACC, cardiologist at the University of California at Los Angeles Medical Center Cardio-Oncology Program in Los Angeles, CA.

