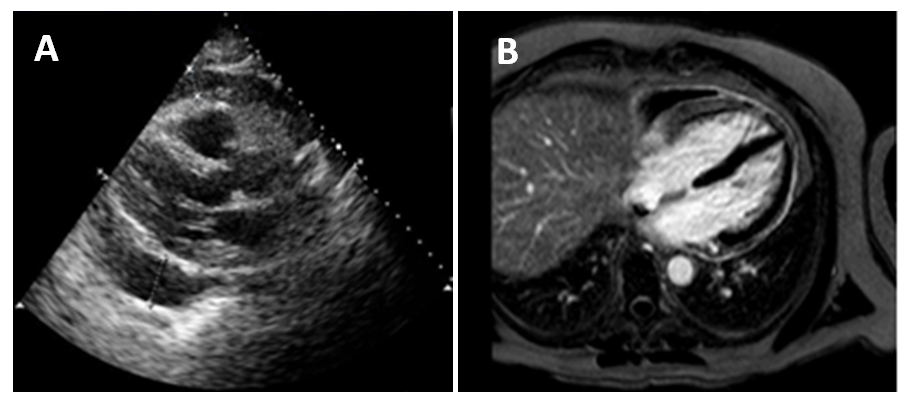
A 63-year-old man presented with complaints of worsening dyspnea, generalized weakness and fatigue for six weeks. He also had a one-year history of frequent upper respiratory tract infections, recurrent otitis media and bilateral hearing loss not responding to antibiotics and steroids. The patient denied chest pain, orthopnea, paroxysmal nocturnal dyspnea, peripheral edema, palpitations or dizziness. On physical examination, his blood pressure was 127/71 mmHg, temperature was 98.7F, respiratory rate was 20 breaths per minute, with an oxygen saturation of 97% and his heart rate was 112 beats per minute. Jugular venous distention was noted at 7 cm H2O. Cardiac exam revealed normal heart sounds, with no murmurs or pericardial rub. Lung exam was clear on auscultation. Electrocardiogram (EKG) revealed sinus tachycardia. Transthoracic echocardiography (Fig A) and subsequent cardiac MRI were performed (Fig B). A complete blood count was unremarkable, with no eosinophilia. B-type Natriuretic Peptide (BNP) was 167. Westergren sedimentation rate (WSR) and C-reactive protein (CRP) levels were elevated at 71 mm/hour and 157 mg/dl respectively. Myeloperoxidase antineutrophil cytoplasmic antibody (MPO ANCA) was positive at 44 units.
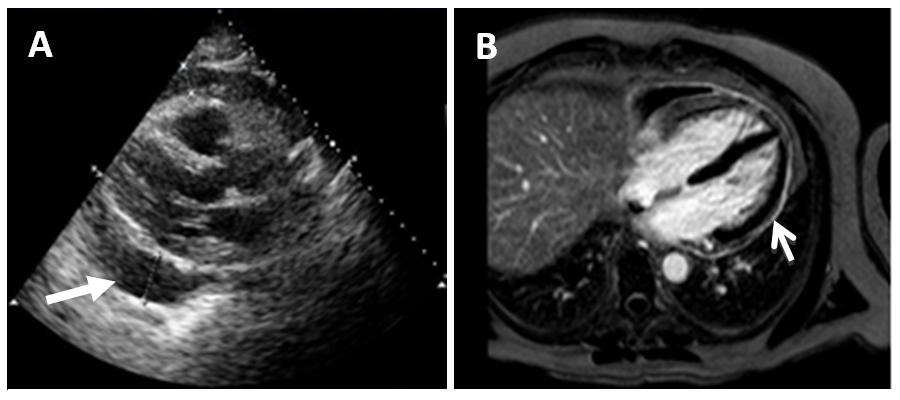
Figures A & B
The correct answer is: C. Acute pericarditis due to granulomatosis with polyangiitis
Granulomatosis with polyangiitis (GPA) (Wegener's disease) is a rare but important cause of acute pericarditis.Cardiovascular examination can frequently be unremarkable as a pericardial rub may not be audible in the presence of a pericardial effusion1. EKG changes typical of pericarditis such as diffuse ST elevation and PR depression are notable in only 60 percent of cases2.
In the above patient, a parasternal long-axis view on transthoracic echocardiogram (Fig A) demonstrated a large (2.7 cm) circumferential pericardial effusion (arrow).
Cardiac magnetic resonance imaging (CMR) (Fig B) demonstrated increased pericardial signal intensity on delayed enhancement imaging (arrow), consistent with acute or sub-acute pericardial inflammation.
Figures A & B
The high levels of WSR and CRP, along with positive symptoms of upper airway tract involvement and positive MPO ANCA, favor the diagnosis of GPA pericarditis in our patient.
Pericardiocentesis was performed and 400 cc of pericardial fluid was removed. Pericardial fluid analysis results were negative for bacteria, red blood cells and malignant cells, with elevated levels of white blood cells. Initially the patient was treated with methotrexate 15 mg/week and prednisone 60/mg per day. Subsequently, methotrexate was changed to cyclophosphamide 150 mg/day. Four weeks later the patient reported marked improvement of symptoms. Prednisone started to taper at a rate of 5 mg/week.
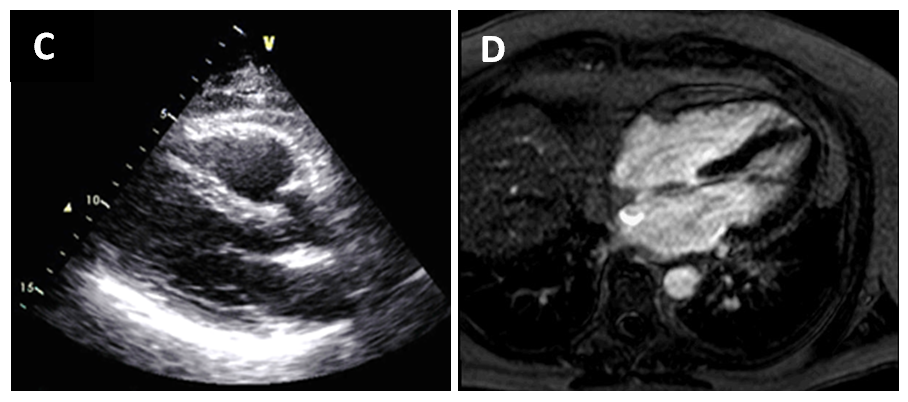
40 days later, repeat imaging was done and showed resolution of the pericardial effusion on transthoracic echocardiography (Fig C) and pericardial enhancement on CMR (Fig D).
Figures C & D
Patients with Churg-Strauss Syndrome often have a long standing history of asthma and demonstrate tissue eosinophilia3. These patients can present with pericarditis, valvular insufficiency and heart failure4, 5.
A diagnosis of drug-induced vasculitis requires identification of a possible offending drug in temporal relation to the symptoms6. Clear evidence for an association with the development of drug-induced vasculitis has been shown for the following drugs: Propylthiouracil, hydralazine, anti-tumour necrosis factor-a (TNF-a) agents, sulfasalazine, D-penicillamine and minocycline7. MPO-ANCA can more often be high along with positive Anti-Histone antibodies.
Echocardiographic features typical for infective endocarditis are 1) an independently mobile intra-cardiac mass on a valve, supporting structure or iatrogenic device, which may be in the path of a regurgitation jet, 2) abscesses, 3) new partial dehiscence of a prosthetic valve, or 4) new valvular regurgitation. Typically, blood cultures are positive in this scenario.
Myocarditis should be suspected in patients with or without cardiac signs and symptoms, who have a rise in cardiac biomarkers (e.g., troponin) but no evidence of myocardial ischemia due to underlying coronary artery disease. They may also present with arrhythmias or heart failure due myocardial dysfunction (typically evident on echocardiogram or CMR)7, 8. A definitive diagnosis of myocarditis is based upon endomyocardial biopsy (EMB)9, 10.
References
- Zayas, R., et al., Incidence of specific etiology and role of methods for specific etiologic diagnosis of primary acute pericarditis. Am J Cardiol, 1995. 75(5): p. 378-82.
- Imazio, M., et al., Day-hospital treatment of acute pericarditis: a management program for outpatient therapy. J Am Coll Cardiol, 2004. 43(6): p. 1042-6.
- Churg, J. and L. Strauss, Allergic granulomatosis, allergic angiitis, and periarteritis nodosa. Am J Pathol, 1951. 27(2): p. 277-301.
- Comarmond, C., et al., Eosinophilic granulomatosis with polyangiitis (Churg-Strauss): clinical characteristics and long-term followup of the 383 patients enrolled in the French Vasculitis Study Group cohort. Arthritis Rheum, 2013. 65(1): p. 270-81.
- Neumann, T., et al., Cardiac involvement in Churg-Strauss syndrome: impact of endomyocarditis. Medicine (Baltimore), 2009. 88(4): p. 236-43.
- Calabrese, L.H., et al., The American College of Rheumatology 1990 criteria for the classification of hypersensitivity vasculitis. Arthritis Rheum, 1990. 33(8): p. 1108-13.
- Caforio, A.L., et al., A prospective study of biopsy-proven myocarditis: prognostic relevance of clinical and aetiopathogenetic features at diagnosis. Eur Heart J, 2007. 28(11): p. 1326-33.
- Howlett, J.G., et al., Canadian Cardiovascular Society Consensus Conference guidelines on heart failure, update 2009: diagnosis and management of right-sided heart failure, myocarditis, device therapy and recent important clinical trials. Can J Cardiol, 2009. 25(2): p. 85-105.
- Richardson, P., et al., Report of the 1995 World Health Organization/International Society and Federation of Cardiology Task Force on the Definition and Classification of cardiomyopathies. Circulation, 1996. 93(5): p. 841-2.
- Elliott, P., et al., Classification of the cardiomyopathies: a position statement from the European Society Of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J, 2008. 29(2): p. 270-6.