Cover Story The Robot Will See You Now... Robotics in the Cath Lab Have Staff Breathing a Sigh of Relief
Seeing a robot advance a guidewire and deploy a stent into the coronary vasculature may seem like the stuff of science fiction, but it turns out just such a robot may one day make an appearance at a catheterization laboratory near you.
In the last few years, several studies have shown not only the safety and efficacy of robotic PCI in the technical performance of the procedure, but also its benefit in reducing radiation exposure and orthopedic injuries to operators and staff who work daily to revascularize stenotic arteries.
"How do you put an economic value to the reduction in radiation, operator fatigue and orthopedic injuries associated with the practice of interventional cardiology?" — Ehtisham Mahmud, MD, FACC
Further making robotic PCI’s case is just published research that shows its ability to perform in complex PCI. Yet there remains limited data showing clear patient benefit, which will likely be needed to justify the cost of the system.
"The value proposition is the most important piece of the puzzle," Ehtisham Mahmud, MD, FACC, said in an interview with Cardiology: Interventions. "How do you put an economic value to the reduction in radiation, operator fatigue and orthopedic injuries associated with the practice of interventional cardiology?"
What is Robotic PCI?
Robotic PCI is U.S. Food and Drug Administration (FDA) and CE mark approved, albeit with only one company currently in the coronary PCI space. Corindus Vascular Robotics was started in Israel in 2002 by interventional cardiologist Rafael Beyar, MD, DSc, FACC, and Tal Wenderow. It is now a Waltham, MA-based, publicly-traded company.
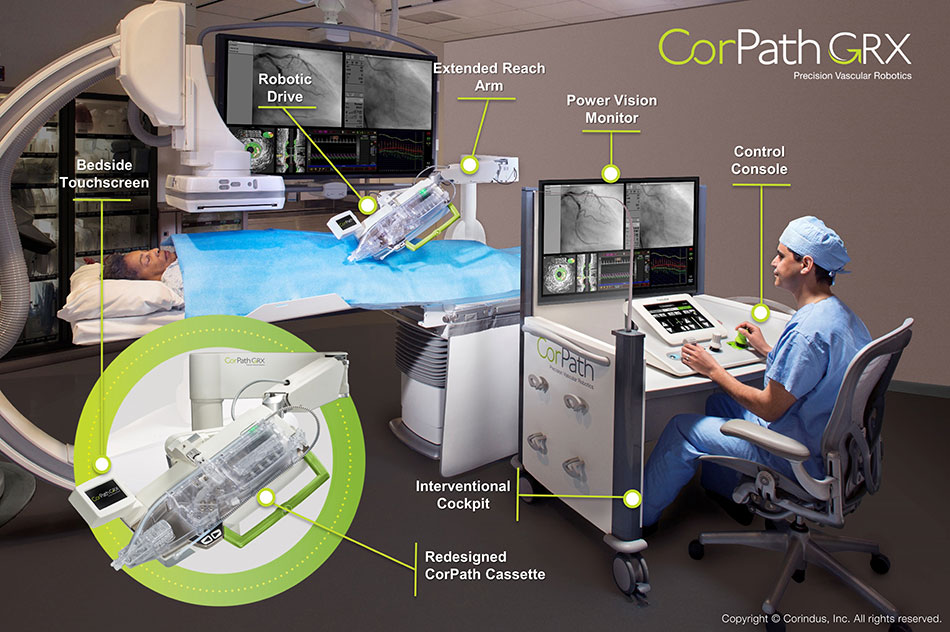
The Corindus CorPath 200 system has essentially two components: a bedside robotic arm that sits on the table with the patient and into which the interventional devices — balloons, guidewires, stents — are loaded. Removed from the bedside is the cockpit from which the physician operates. The cockpit is lead-lined and allows the operator to be seated and to use multiple joysticks and a touch-screen pad to control movement of the robotic arm.
PRECISE also showed, although with some stated limitations in how radiation exposure data were collected, that radiation exposure for the primary operator was 95.2 percent lower than the levels found at the traditional table position (p < 0.0001).
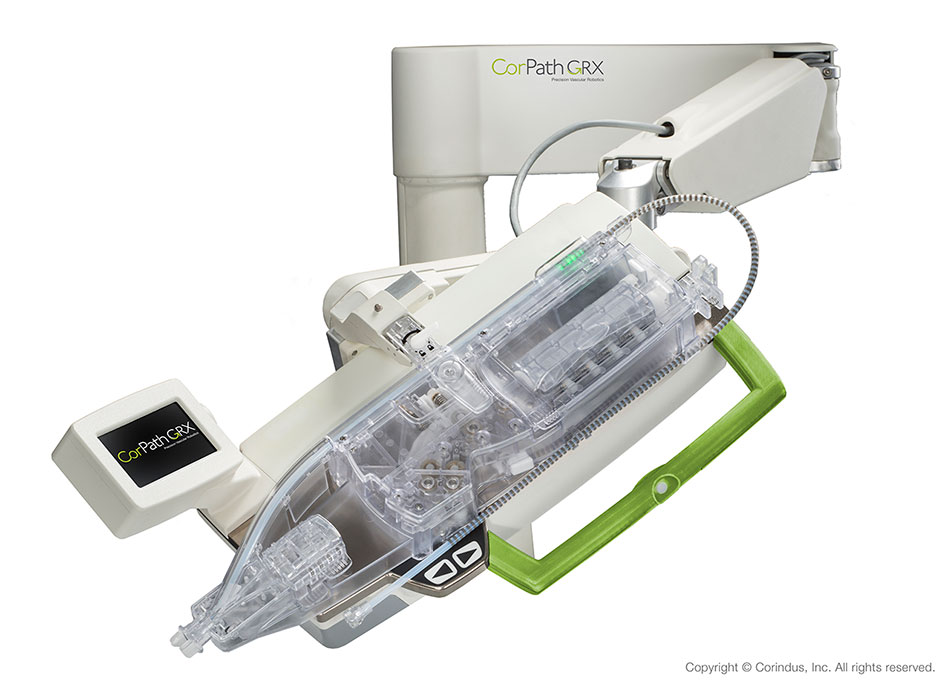
The next-generation CorPath GRX system offers enhancements to the platform by adding upgrades, including a third joystick that controls the guide catheter, and extends the range of procedures that can be performed robotically.
While the robotic arm facilitates advancing the guidewire and stent, manual access of the artery is necessary. Also, diagnostic angiograms still need to be done bedside, which, of course, still leaves physicians and staff exposed to radiation and wearing lead aprons.
For Ryan Madder, MD, FACC, the answer to not being able to perform diagnostic angiograms with the robotic system is to use a lead suit suspended from the ceiling. "I can probably count on one hand the number of times I actually wore lead garments in the course of a year."
With current robotic PCI systems, only the operator is behind the protected console. The other staff in the lab are able to stand farther away from the radiation source, said Mahmud, but the extent to which the technology protects non-physician staff from radiation exposure is not yet clear.
Could it be that CorPath will soon face competition? Robocath, a robotics company in Rouen, France, just announced the conclusion of a fundraising round worth $5.2 million to market their medical robotic platform, R-one, for use in interventional cardiovascular medicine. The R-one is currently "in the approval phase" and will be marketed from 2018, mainly in Europe and the Middle East, says the company. Its U.S. launch is anticipated in 2019.
PRECISE
The CorPath 200 received FDA 510(k) clearance in 2012 for use in the "remote delivery and manipulation of coronary guidewires and balloon/stent catheters during PCI." The approval was based on findings from the PRECISE trial, which showed excellent technical and procedural success for robotic PCI in 164 patients (98.8 percent and 97.6 percent, respectively).1 The majority (83.2 percent) of lesions treated were non-C lesions, based on the ACC/American Heart Association (AHA) classification.
Only two patients had their procedures converted to manual operation when the operators experienced severe resistance during stent placement. All procedures were performed via femoral artery access.
PRECISE also showed, although with some stated limitations in how radiation exposure data were collected, that radiation exposure for the primary operator was 95.2 percent lower than the levels found at the traditional table position (p <0.0001).
"I think this was the most important piece of information to come from the PRECISE study," said Madder. To better understand this finding, he offered some perspective in a SCAI 2017 talk. In an example of two physicians who begin their careers at the same time, one who decides to only do manual PCI throughout his career and one who decides to do only robotic PCI, the annual radiation exposure for 100 PCIs would be just over 2000 µGy [2,060 µGy] for the manual-only operator — and just 98 µGy for the robotic-only operator. After 20 years, the robotic-only operator’s exposure would be 1,960 µGy — less than the exposure in just the first year for the manual-only operator, whose cumulative exposure at 20 years would be 41,200 µGy.
"These differences, with a 95 percent reduction in radiation exposure with these devices, I think can really add up and may have a dramatic effect on radiation safety," said Madder.
Maximizing PRECISION and Beyond
Nothing opens a hospital administrator’s pocket quite as quickly as improved outcomes, or the converse: seeing other hospitals report better outcomes than yours. Could robotic PCI improve angiographic or patient-related outcomes via some of its enhanced technical features?
The PRECISION multicenter post-market registry evaluates CorPath 200 success stratified by access site. The findings presented at SCAI 2017 by Mahmud covered 754 patients with a total of 949 lesions who were treated with robotic PCI using transradial access in 59.9 percent and transfemoral access in 39.5 percent, with the choice being left to patients and operators. With both approaches, roughly two-thirds of lesions treated were type B2 or type C ACC/AHA lesions, making this a more complex set of lesions than previously treated robotically.
"With both the femoral and radial approach, the visually estimated length turned out to be lower than it was measured with the robotic platform… and this led to changes in the stent selection made based on the visual estimate." — Ehtisham Mahmud, MD, FACC
Operators were asked to visually estimate the lesion length and select a stent for each lesion before stenting. Interestingly, said Mahmud, and offering a hint that robotic PCI might improve patient-related outcomes, "with both the femoral and radial approach, the visually estimated length turned out to be lower than it was measured with the robotic platform… and this led to changes in the stent selection made based on the visual estimate."
In the femoral arm, stent selection was changed 22.5 percent of the time using the measurement made by the robotic system, and in the radial arm, it was changed 33.2 percent of the time.
Clinical success, defined as completion of the PCI procedure with stent implantation and <30 percent stenosis with final TIMI 3 flow and no in-hospital major adverse cardiovascular event, was high in both groups, but significantly higher with transradial access (98.9 percent radial vs. 94.9 percent femoral; p = 0.0012).
When manual assistance or conversion to manual was needed, the reasons included guidewire or catheter support issues, robotic platform limitations, such as the need to do bifurcation stenting or kissing balloon angioplasty, or in a small proportion of patients, MACE.
Technical success, defined as clinical success plus no unplanned manual assistance was 88.6 percent with the transradial approach and 82.4 percent for the transfemoral approach (p = 0.02).
The just-published CORA-PCI trial takes robotic PCI one step further.2 The trial, led by Mahmud and first presented at SCAI 2016, included 413 individual PCI procedures performed either with the CorPath system or manually.
Patients with complex coronary lesions, including mild to moderate calcification, chronic total occlusions, bifurcation disease, severe tortuosity and unprotected left main disease were enrolled. From these, 79 cases were excluded because they were not technically feasible using robotic assistance (e.g., over-the-wire device requirement, planned bifurcation stenting).
A total of 315 patients underwent 334 PCI procedures (108 robotic PCIs, 157 lesions, 78.3 percent type B2/C lesions; 226 manual PCIs, 336 lesions, 68.8 percent type B2/C lesions).
Technical success for robotic PCI was seen in 91.7 percent: manual assistance was needed in 11.1 percent and manual conversion in 7.4 percent. Clinical success was seen in 99.1 percent.
Stent use and fluoroscopy time did not differ between the manual and robotic arms, but procedure time was longer with transfemoral robotic PCI (44 min vs. 36 min; p = 0.002).
Corindus is now launching the PRECISION GRX study, a post-market registry of the second-generation CorPath GRX System, which offers improvements in guide catheter control that may help reduce the need for manual assistance.
What is the Value Proposition?
Probably the biggest question surrounding robotic PCI today is not a clinical one, but whether its proponents can define their value proposition.
Looking at the bulk of the evidence, it appears the benefits of robotic PCI are mostly for the physician, with some spill over to the rest of the cath lab staff and hints, but not waves, of benefit for patients themselves.
The initial cost of the CorPath GRX is in the range of $650,000, along with an additional $650-750 cost for the single-use accessory cartridge. Currently, there are 48 CorPath Systems installed worldwide, 45 of which are located in the U.S.
Looking at the bulk of the evidence, it appears the benefits of robotic PCI are mostly for the physician, with some spill over to the rest of the cath lab staff and hints, but not waves, of benefit for patients themselves.
For his part, Mahmud uses the CorPath whenever he can. At his center, they have four cardiac cath labs, one equipped with a CorPath 200 System, and the second with the CorPath GRX system. They are training fellows on the system and he estimates that it takes them between 20 and 25 cases to "get comfortable" with complex cases, but adds that the more experience an operator has the quicker the transition to the robotic system.
Mahmud figures about 75 percent of his cases can be done robotically, which should be sufficient for a high-volume operator to, hopefully, avoid radiation- and lead-related issues. He hopes further study will show that the system can be used to conduct PCI in remote areas, allowing local interventionalists to attempt more complex cases knowing they can rely on robotic assistance delivered remotely by more experienced operators.
Another path to purchase may require a small uprising from physicians cath lab staff who opt to act upon the growing body of knowledge that shows they are putting their own lives at risk every time they go to work.
Unfortunately, said Mahmud, physicians don’t tend to advocate for themselves very well, and may need to step up pressure on hospital administration. Patient and physician acceptance and satisfaction with robotic PCI is high, but will hospital administrators wary of pricey, niche capital investments foot the bill?
References
- Weisz G, Metzger DC, Caputo RP, et al. J Am Coll Cardiol 2013;61:1596-600.
- Mahmud E, Naghi J, Ang L, et al. JACC Cardiovasc Interv 2017;10:1320-27.
|
Tweet this article: Tweet
 |
|
| Click the cover image above to read the latest issue of Cardiology Interventions in e-pub format or click here to read it on the web! | |
Clinical Topics: Invasive Cardiovascular Angiography and Intervention, Interventions and Imaging, Angiography, Nuclear Imaging
Keywords: ACC Publications, Cardiology Interventions, Femoral Artery, Robotics, United States Food and Drug Administration, American Heart Association, Coronary Vessels, Catheters, Angiography, Stents, Catheterization, Radiation
< Back to Listings