Feature Story | Coronary Total Occlusions and PCI: New Insights, New Data
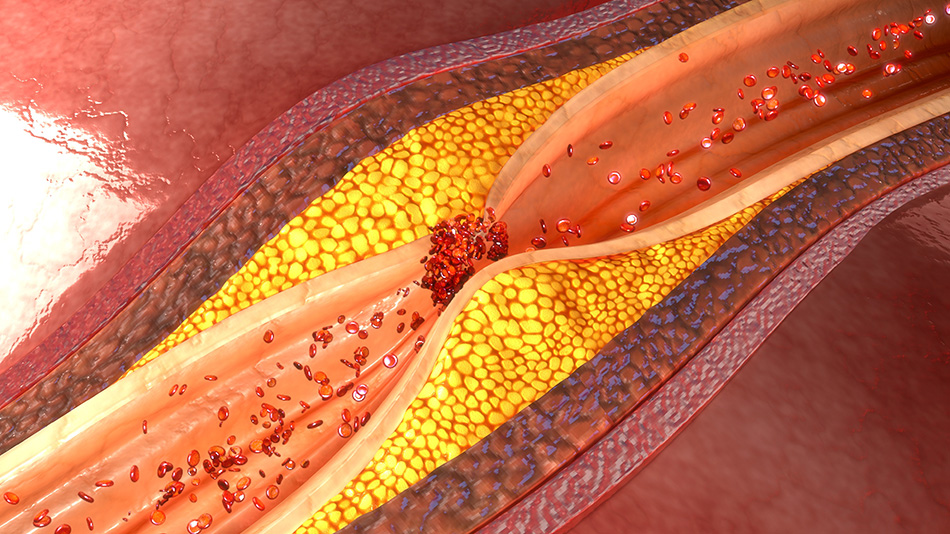
The risks and benefits of PCI for chronic total occlusion (CTO) along with its place in treatment continues to be debated. CTO is generally considered the most complex lesion subset in contemporary practice and has even been called the last frontier in interventional cardiology. The tremendous strides in dedicated technology and techniques in recent years has translated to higher procedural success without sacrificing safety. Yet, the rate of CTO PCIs performed, compared with non-CTO PCIs, in the U.S. is stagnant.
“The key barriers limiting the transition of CTO PCI from a niche to conventional procedure are widespread interventional expertise and a limited amount of randomized trial-generated evidence to support its use,” write Manesh R. Patel, MD, FACC, and J. Antonio Gutierrez, MD, in a recent editorial in JACC: Cardiovascular Interventions.
The ACC/American Heart Association guideline limits the performance of CTO PCI to experienced, expert operators – and the number of these is limited, as is the number of training programs. As David J. Moliterno, MD, FACC, writes in the same issue of the journal, CTO lesions are “more challenging, more time consuming, and have dynamic and relatively steep learning curves.” As he writes, “the successful practice of treating CTOs cannot be casual or stagnate – no dabbling allowed… this is an area with continuous training opportunity.”
"The key barriers limiting the transition of CTO PCI from a niche to conventional procedure are widespread interventional expertise and a limited amount of randomized trial-generated evidence to support its use." — Manesh R. Patel, MD, FACC, and J. Antonio Gutierrez, MD
The hybrid algorithm developed by Emmanouil S. Brilakis, MD, FACC, et al., has been shown to enhance success rates in complex CTO lesions and to be reproducible and teachable. It has become the basis of discussion and reference for CTO PCI worldwide. “They are to be credited with executing a remarkable and efficacious proctoring program that has radically altered the landscape of CTO intervention in North America and Europe,” write Scott A. Harding, MD, et al., also in this issue of JACC: Cardiovascular Interventions. However, they note that in the Asia Pacific region, where most of the world’s population resides, there’s been infrequent adoption of the hybrid algorithm. In part this is because of traditional wire-based CTO teaching dominant in the region, limited access to the CrossBoss and Stingray systems and lower rates of CABG.
The Asia Pacific CTO club has proposed a new algorithm for CTO PCI that would be relevant and applicable globally, says Harding and colleagues. Formed by a group comprised of 10 high-volume CTO operators recognized as leaders in CTO in their respective countries, the Asia Pacific CTO club has developed an algorithm that allows for differing skill sets and equipment availability and contains practical teachings for CTO PCI. “It is hoped that this algorithm will serve as the basis for future CTO PCI proctoring and training,” write Harding et al.
The hybrid approach is based upon accurate and detailed angiographic assessment of both the CTO vessel and the vessel providing collaterals. After considering the anatomy and quality of the proximal cap, the distal vessel, and the collateral supply, an antegrade or retrograde approach is selected. The next step involves assessing the lesion length and favoring pursuit of the true lumen for shorter lesions and a dissection/reentry plan if this fails or for longer lesions.
The new Asia Pacific CTO club algorithm uses these same feature assessments, although it places less emphasis on lesion length and more on a combination of factors including tortuosity, calcification and prior failed attempts. There’s more emphasis on imaging, including pre-procedural coronary computed tomography and procedural intravascular ultrasound. Importantly, Harding and colleagues recommend that cases with a J-CTO score ≥2 should be reserved for operators who have performed at least 200 CTO procedures and who can achieve a ≥85 percent success rate in unselected cases. Moliterno notes this provide the opportunity to gain proctoring or guidance, especially for dissection/reentry cases and use of new devices.
To advance the field, along with the need for randomized trial data, there’s a need to harmonize clinical endpoints and key data elements, write Luiz Fernando Ybarra, MD, MBA, et al., in another article in the issue. The significant heterogeneity in this regard limits the interpretation and comparisons between the CTO trials published to date and the design of future CTO trials. They call for a Chronic Total Occlusion Academic Research Consortium. The Academic Research Consortium that developed a set of consensus definitions for regular coronary stent trials, contributing to the advancement of that field, can serve as a model.
New Data on CTO PCI
Most data on CTO PCI comes from registries and meta-analyses in patients with stable coronary artery disease and suggest symptom improvement is the primary benefit. Angina is ameliorated and exercise capacity and left ventricular ejection fraction (LVEF) improved with CTO PCI compared with optimal medical therapy.
Only three randomized clinical trials contribute to the evidence base for CTOs. None show an improvement in major adverse cardiac and cerebrovascular events (MACCE). The EXPLORE trial of 304 patients with STEMI and concurrent CTO of a native coronary artery (reference vessel ≥2.5 mm) showed no difference in the primary outcome of LVEF after four months between the patients who did and did not have PCI CTO. In the two trials comparing CTO PCI and optimal medical therapy, one showed improvement in quality of life. The EURO-CTO trial in 396 patients, presented at EuroPCR 2017, found a significant improvement in the primary outcome of quality of life as measured by the Seattle Angina Questionnaire but no difference in the secondary outcome of MACCE.
The DECISION-CTO trial in 834 patients, presented at ACC.17, did not find an improvement in the primary outcome of MACCE or the secondary outcome of quality of life. Patel and Gutierrez note that in DECISION-CTO, patients were randomized before symptomatic non-CTO lesions were treated, thus it’s likely the study did demonstrate an improvement in quality of life. Neither the EURO-CTO or DECISION-CTO trial has been published.
"Whether CTO-PCI may improve patient outcomes remains controversial. These findings from REVASC are a good first step in assessing the benefits, but should be considered preliminary given the small study size." — Kim Eagle, MD, MACC, ACC.org Editor-in-Chief
New data from the OPEN-CTO PCI registry showed that 412 patients with diabetes enjoyed a similarly robust improvement in symptoms after CTO PCI as 588 patients without diabetes. At one year, angina burden, quality of life and overall health status scores were similar in both groups. OPEN-CTO was a single-arm, prospective registry of consecutive patients who underwent attempted CTO PCI using the hybrid approach at 12 high-volume centers in the U.S. between January 2014 and July 2015. Complication rates were similar in patients with and without diabetes, according to Adam S. Salisbury, MD, MSc, FACC, who reported the results of their retrospective subgroup analysis in JACC: Cardiovascular Interventions. The crude technical success rate was significantly lower in patients with diabetes (83.5 percent, vs. 88.1 percent without diabetes; p = 0.04). However, the difference was no longer significant after adjustment for baseline characteristics, complexity of coronary artery disease and prior CABG.
Another high-risk group, patients with LVEF ≤35 percent with a CTO, were shown to benefit equally from PCI as patients with an LVEF of 35-50 percent or ≥50 percent in a prospective, observational study reported by Alfredo R. Galassi, MD, FACC, et al., in JACC: Cardiovascular Interventions. At two years, MACCE-free survival was similar in the groups (75.2 percent, 82.8 percent and 86 percent, respectively). Conducted at three centers in Europe, the study included 839 patients who underwent CTO PCI attempts, of whom 72 (8.6 percent) had an LVEF ≤35 percent. The angiographic success was high at 93.6 percent overall and similar across the three groups. Notably, successful CTO PCI significantly improved LVEF in those with a low LVEF (from 29.1 percent to 41.6 percent; p < 0.001).
Patel and Gutierrez write this study reaffirms that in the hands of experienced operators, CTO PCI can be executed with a high degree of success (>90 percent) with minimal complications (<3 percent). Further, “the study extends prior findings regarding the benefit of successful CTO PCI and left ventricular function by demonstrating a mean improvement in LVEF of >10 units in patients with a baseline LVEF ≤35 percent,” they write. Studies will be needed to determine if this will translate to an improvement in survival with CTO PCI, to compare with the studies of CABG conducted in patients with a low LVEF.
In the REVASC study, presented at TCT 2017, neither regional or global LV function was improved with CTO PCI in patients receiving optimal medical therapy. Presented by Kambis Mashayekhi, MD, the study did not find a difference between the two strategies for the primary outcome of segmental wall thickening after six months as measured by cardiac MRI.
REVASC included 205 patients with a CTO and clinical symptoms or a positive functional test for ischemia. They were randomized to PCI of the CTO plus optimal medical therapy (n = 101) or optimal medical therapy with the option of PCI for non-CTO lesions (no-PCI-CTO group; n = 104). Patients with an LVEF <25 percent were excluded, along with those with an acute coronary syndrome within 72 hours or contraindications to cardiac MRI. At baseline, the LVEF was 59.6 percent in the no-CTO-PCI group and 54.7 in the CTO-PCI group.
In a subset of patients without major non-CTO lesions, they found that CTO-PCI was “associated with a trend towards larger improvement in segmental wall thickening than no-CTO-PCI.” The number of major adverse cardiovascular events at 12 months was also lower in the CTO-PCI group compared with the no-CTO-PCI group (six vs. 17 events). Clinically driven repeat revascularization occurred in 16 patients in the no-CTO-PCI group, compared with five in the CTO-PCI group.
Mashayekhi noted the difficulty of measuring benefit with CTO PCI in patients with preserved global LV function. He also noted this study shows there’s time to consider how to address the CTO, because delaying its treatment will not reduce the benefit of PCI if it’s performed after optimal medical therapy is considered to have failed.
“Whether CTO-PCI may improve patient outcomes remains controversial,” said ACC.org Editor-in-Chief Kim Eagle, MD, MACC. “These findings from REVASC are a good first step in assessing the benefits, but should be considered preliminary given the small study size.”
The CrossBoss First trial, also presented at TCT 2017, showed the upfront use of the CrossBoss catheter for antegrade crossing of CTOs was associated with a similar crossing time, similar success and complication rates and similar equipment utilization and cost, compared with wire escalation. The results were presented by Brilakis and also published in the JACC: Cardiovascular Interventions.
The study randomized 246 patients between 2015 and 2017 to CrossBoss (n = 122) or wire escalation (n = 124) at 11 centers in the U.S. Baseline and clinical angiographic characteristics of both groups were similar. The mean patient age was 65.5 years, 82 percent of patients were men, 37 percent had diabetes and 26 percent had prior coronary bypass surgery.
The primary endpoints were time required to cross the CTO or abort the procedure, and the frequency of procedural major adverse cardiovascular events. Researchers also assessed secondary endpoints related to technical and procedural success, total procedure time, fluoroscopy time required to cross and total fluoroscopy time, total air kerma radiation dose, total contrast volume and equipment utilization.
Results showed technical and procedural success were 87.8 percent and 84.1 percent, respectively, and were similar in the two groups. Crossing time, the primary endpoint, was also similar at 56 minutes in the CrossBoss and 66 minutes in the wire escalation group (p = 0.323).
Researchers noted that post hoc subgroup analyses showed upfront use of the CrossBoss was associated with shorter crossing time than wire escalation in CTOs due to in-stent restenosis, but “there was no difference in short (<20 mm) or longer (≥20 mm) lesions, lesions with and without proximal cap ambiguity, moderate or severe calcification, and moderate or severe tortuosity.”
“The post hoc subgroup analysis needs to be viewed as a preliminary finding, given there was no overall difference in the primary endpoint,” says Eagle.
The incidence of major adverse cardiovascular events was also similar across the CrossBoss and wire escalation groups at 3.28 percent vs. 4.03 percent, respectively. Additionally, researchers did not find any significant differences in other secondary endpoints, including equipment utilization and equipment cost. What’s next? The researchers suggest “new devices and crossing techniques are needed to further improve the success rates and procedural efficiency and reduce the complication rates of coronary chronic total occlusion interventions.”
Overall for the CTO PCI field, it’s hoped that the SHINE-CTO trial will shed more light on the benefits of CTO PCI. Led by Brilakis and colleagues, the study is randomizing patients to CTO PCI or a sham procedure and the primary endpoint is the change in disease-specific health status.
Clinical Topics: Acute Coronary Syndromes, Anticoagulation Management, Cardiac Surgery, Cardiovascular Care Team, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Atherosclerotic Disease (CAD/PAD), Anticoagulation Management and ACS, Cardiac Surgery and SIHD, Interventions and ACS, Interventions and Coronary Artery Disease, Interventions and Imaging, Magnetic Resonance Imaging, Nuclear Imaging
Keywords: ACC Publications, Cardiology Interventions, Acute Coronary Syndrome, Algorithms, American Heart Association, Angina Pectoris, Calcification, Physiologic, Calcinosis, Consensus, Coronary Artery Bypass, Coronary Artery Disease, Diabetes Mellitus, Fluoroscopy, Health Status, Hirudins, Incidence, Learning Curve, Magnetic Resonance Imaging, Prospective Studies, Quality of Life, Radiation Dosage, Registries, Research Personnel, Retrospective Studies, Risk Assessment, Myocardial Infarction, Stents, Stroke Volume, Tomography, Ventricular Function, Left
< Back to Listings


