Cover Story | Gestational Hypertension and Preeclampsia: Nontraditional Risk Factors For Cardiovascular Disease
Pregnancy is a predictor of future cardiovascular health in women. Cardiovascular disease has been estimated to be present in 1 to 4 percent of pregnancies. The incidence of pregnancies in women with heart disease is rising, mainly due to an increased number of women with congenital heart disease reaching childbearing age, advancing maternal age and an increased incidence of risk factors, including diabetes, hypertension, preeclampsia (PE) and multifetal pregnancies.
Current guidelines concentrate on management of cardiovascular disorders in pregnancy, such as native valvular heart disease, prosthetic valve disease, congenital heart disease, arrhythmias, diseases of the aorta and dilated cardiomyopathies. However, many women are at risk of developing future cardiovascular disease from pregnancy-related complications such as PE, gestational hypertension (GH), gestational diabetes (GD), preterm labor, etc., and are often lost to follow-up.1,2
Defining Hypertension in Pregnancy
Hypertension during pregnancy can occur in one of three forms: chronic hypertension, GH and PE. Chronic hypertension is defined as elevated blood pressure known before conception or diagnosed before 20 weeks of gestation. GH is hypertension that develops any time after 20 weeks of gestation without proteinuria. PE is defined as hypertension (blood pressure >140/90 mm Hg) with organ damage that develops after 20 weeks of gestation and has the potential to result in serious adverse consequences for the mother and fetus. Target organ damage can be manifested by proteinuria, thrombocytopenia, elevated creatinine or liver transaminases, pulmonary edema or cerebral or visual symptoms. Severe hypertension is defined as systolic blood pressure >170 mm Hg or diastolic blood pressure >110 mm Hg.
Traditional and Nontraditional ASCVD Risk Factors in Women
Increasing among women and more impactful traditional risk factors for atherosclerotic cardiovascular disease (ASCVD) include diabetes, hypertension, dyslipidemia, smoking, obesity and physical inactivity. Emerging, nontraditional ASCVD risk factors include preterm delivery, hypertensive pregnancy disorders, GD, breast cancer treatments, autoimmune diseases and depression.1
Emerging Data on Association of PE, GH and Cardiovascular Disease
A recent study in Circulation found accelerated atherosclerosis in women aged 45-55 years with a history of PE.3 Computed tomographic angiography detected signs of coronary plaques in 30 percent of women who had PE 10 to 20 years prior compared with 18 percent of age-matched women in a reference group.
A large study published in the Annals of Internal Medicine in July 2018 helps provide some more insight into the cause and effect of PE and GH.4 Data from almost 60,000 participants in the historic Nurses' Health Study II were analyzed. This study reported that women with GH and PE had almost a threefold and sixfold increased rate of chronic hypertension in later life, respectively. It also showed that women who were hypertensive during their first pregnancy had a 70 percent increased risk of type 2 diabetes and 30 percent increased prevalence of hypercholesterolemia later in life. All associations remained after adjustment for prepregnancy body mass index, family history and other confounders.
A Norwegian study with a mean follow-up of 17.2 years found that women with PE alone had a twofold increased risk of a major cardiovascular disease event, whereas women with PE plus preterm delivery or small-for-gestational-age baby were four times as likely to have a major cardiac event compared with women with uncomplicated pregnancies.5
In a recent prospective observational study in the Journal of American College of Cardiology, women with severe PE had a higher right ventricular systolic pressure, decreased global right ventricular longitudinal systolic strain and lower mitral septal e' velocity when compared with the control cohort of normal pregnancies.6 Of the patients with PE, 12 percent also had grade II diastolic dysfunction and 9.5 percent had peripartum pulmonary edema. These data demonstrate that adverse outcomes of pregnancy are common and highlight the need for antenatal surveillance, risk stratification and close long-term follow-up of patients with these complications.
Management of Hypertensive Disorders in Pregnancy
For primary prevention of PE, the American College of Obstetricians and Gynecologists (ACOG) recommends the use of aspirin 60-80 mg daily in high-risk women, defined as previous history of early onset PE and preterm delivery before 34 weeks of gestation or PE in more than one pregnancy.7 If the pregnancy is at 37 weeks or later, the health care provider will usually want to deliver the fetus to treat preeclampsia and avoid further complications. If the pregnancy is at less than 37 weeks, however, the mother and her health care provider may consider treatment options that give the fetus more time to develop, depending on the severity of the condition.
For a mild increase in blood pressure, home blood pressure measurement and frequent check-ins at the clinic are recommended.8 The National Institutes of Health-sponsored Working Group on High Blood Pressure in Pregnancy recommends antihypertensive therapy for blood pressures exceeding a threshold of 150 to 160 mm Hg systolic or 100 to 110 mm Hg diastolic or in the presence of target organ damage, such as left ventricular hypertrophy or renal insufficiency.8
Medical therapy consists of the nonselective beta-blocker labetalol and the calcium-channel blocker (CCB) nifedipine. These first-line drugs have similar efficacy in controlling hypertension during pregnancy and are commonly used due to their good safety profiles. Closer monitoring of the woman and her fetus are recommended, with frequent tests to assess platelet counts, liver enzymes, and kidney function and urine protein levels. Tests for the fetus might include ultrasound, heart rate monitoring, assessment of fetal growth and assessment of amniotic fluid. Methyldopa has a long history of use in pregnancy and is still used, although it is not as effective and is considered a second-line therapy after CCBs and beta-blockers.
For severe hypertension, intravenous labetalol, oral nifedipine and intravenous hydralazine are equally effective. In such cases with severe preeclampsia, the woman will be admitted to the hospital for close and continuous monitoring. Loop diuretics like furosemide are used in patients with pulmonary edema and lower extremity edema. Treatment in the hospital may include intravenous medication to control blood pressure and anticonvulsive therapy with magnesium sulphate to prevent seizures or other complications, as well as steroid injections to help speed up the development of the fetus's lungs. Lastly, preterm labor may not be avoided due to the risk of complications to the mother and the fetus.
Take Action: Steps to Assess Gestational Risk

Lack of physician awareness is one of the main reasons women who have been pregnant are lost to follow-up and fall through the cracks. Gestational risk factors should be stressed during obstetric and internal medicine training. More focused patient education during pregnancy may help in reducing the knowledge gap.
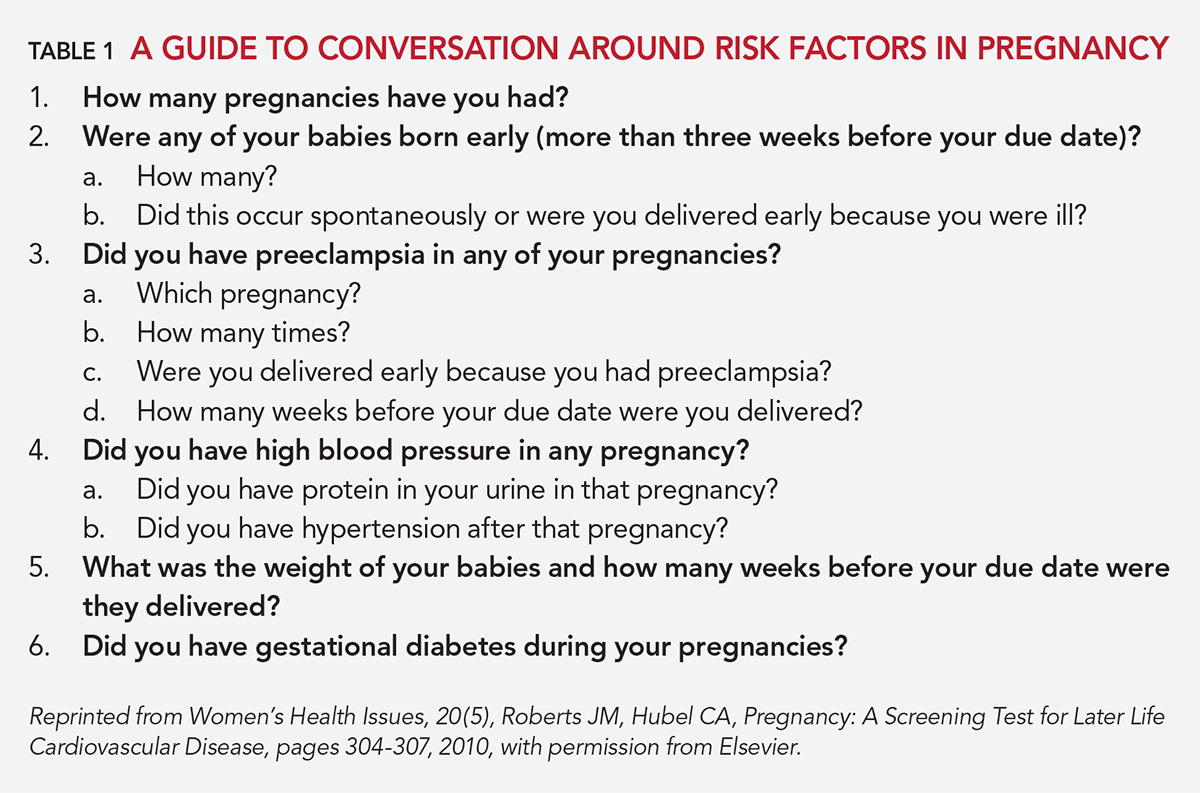
Increasing awareness among primary care providers, cardiologists and cardiovascular team members as well as gynecologic-obstetrical team members of the long-term risks of this unique population is a start. Importantly, all clinicians throughout the care continuum should engage a postpartum woman in a detailed conversation about her own health and discuss the potential health of her future pregnancies. Table 1 provides a guide for this conversation. Focused questions with patients can lead to easily identifying some of the pregnancy-related complications, such as PE, GH, preterm delivery and small-for-gestational-age birth.
Screening for cardiovascular diseases should begin soon after a pregnancy complicated by hypertensive disorder. A large study published in BMJ last year showed that women with a hypertensive disorder of pregnancy had rates of hypertension that were 12 to 25 times higher than women with a normotensive pregnancy in the year after delivery and an increased risk persisted for decades.9
Recently ACOG released a postpartum toolkit to address the care of women after delivery. They call the postpartum period "The Fourth Trimester" and the toolkit provides resources on postpartum weight management, postpartum follow-up of chronic disease of the cardiovascular and renal systems and long-term follow-up of pregnancy-related complications.
High-risk co-management clinics for postpartum cardiovascular disease counseling need to be created, with the participation of the obstetrical team, cardiovascular providers and primary care provider.
The increasing evidence of the impact of pregnancy on a woman's future cardiovascular health – and the increasing awareness by clinicians and women – will likely bring a paradigm shift in the next decade to early screening in pregnancy for ASCVD risk factors, which will require substantial changes to current models of antenatal care.
Garima Sharma, MD, FACC, is assistant professor of medicine at Johns Hopkins School of Medicine.
References
- Garcia M, Mulvagh SL, Merz CN, Buring JE, Manson JE. Circ Res 2016;118:1273-93.
- Abbasi J. JAMA 2018;October 17:[Epub ahead of print].
- Zoet GA, Benschop L, Boersma E, et al. Circulation 2018;137:877-9.
- Stuart JJ, Tanz LJ, Missmer SA, et al. Ann Intern Med 2018;169:224-32.
- Riise HK, Sulo G, Tell GS, et al. J Am Heart Assoc 2017;6.
- Vaught AJ, Kovell LC, Szymanski LM, et al. J Am Coll Cardiol 2018;72:1-11.
- American College of Obstetricians and Gynecologists; Task Force on Hypertension in Pregnancy. Obstet Gynecol 2013;122:1122-31.
- Ghanem FA, Movahed A. Cardiovasc Ther 2008;26:38-49.
- Behrens I, Basit S, Melbye M, et al. BMJ 2017;358:j3078.
Clinical Topics: Arrhythmias and Clinical EP, Cardiovascular Care Team, Congenital Heart Disease and Pediatric Cardiology, Diabetes and Cardiometabolic Disease, Dyslipidemia, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Prevention, Valvular Heart Disease, Vascular Medicine, Implantable Devices, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, CHD and Pediatrics and Arrhythmias, CHD and Pediatrics and Imaging, CHD and Pediatrics and Interventions, CHD and Pediatrics and Prevention, CHD and Pediatrics and Quality Improvement, Homozygous Familial Hypercholesterolemia, Statins, Acute Heart Failure, Interventions and Imaging, Interventions and Structural Heart Disease, Interventions and Vascular Medicine, Angiography, Nuclear Imaging, Hypertension, Smoking
Keywords: ACC Publications, Cardiology Magazine, Ambroxol, Amniotic Fluid, Angiography, Coronary Angiography, Antihypertensive Agents, Aorta, Arrhythmias, Cardiac, Aspirin, Atherosclerosis, Autoimmune Diseases, Blood Pressure, Blood Pressure Determination, Body Mass Index, Breast Neoplasms, Calcium Channel Blockers, Cardiomyopathy, Dilated, Chronic Disease, Cohort Studies, Continuity of Patient Care, Counseling, Creatinine, Depression, Diabetes Mellitus, Type 2, Diabetes, Gestational, Edema, Epidemiologic Studies, Fetus, Follow-Up Studies, Furosemide, Gestational Age, Heart Rate, Heart Valve Diseases, Hydralazine, Hypercholesterolemia, Hypertension, Pregnancy-Induced, Hypertension, Hypertrophy, Left Ventricular, Infant, Newborn, Internal Medicine, Labetalol, Liver, Lost to Follow-Up, Lower Extremity, Magnesium Sulfate, Maternal Age, Methyldopa, Mothers, National Institutes of Health (U.S.), Nifedipine, Obesity, Peripartum Period, Pharmaceutical Preparations, Platelet Count, Postpartum Period, Pre-Eclampsia, Pregnancy, Premature Birth, Prenatal Care, Prevalence, Primary Prevention, Primary Health Care, Prospective Studies, Proteinuria, Pulmonary Edema, Renal Insufficiency, Risk Factors, Seizures, Smoking, Sodium Chloride Symporter Inhibitors, Systole, Thrombocytopenia, Transaminases
< Back to Listings