New in Clinical Documents | New Guideline Outlines Recommendations For Evaluating Managing Bradycardia
A new guideline released by the ACC, American Heart Association (AHA) and the Heart Rhythm Society (HRS) outlines the clinical presentation and approach to clinical evaluation of patients who may have bradycardia or conduction diseases. The guideline supersedes the pacemaker recommendations made in the ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities.
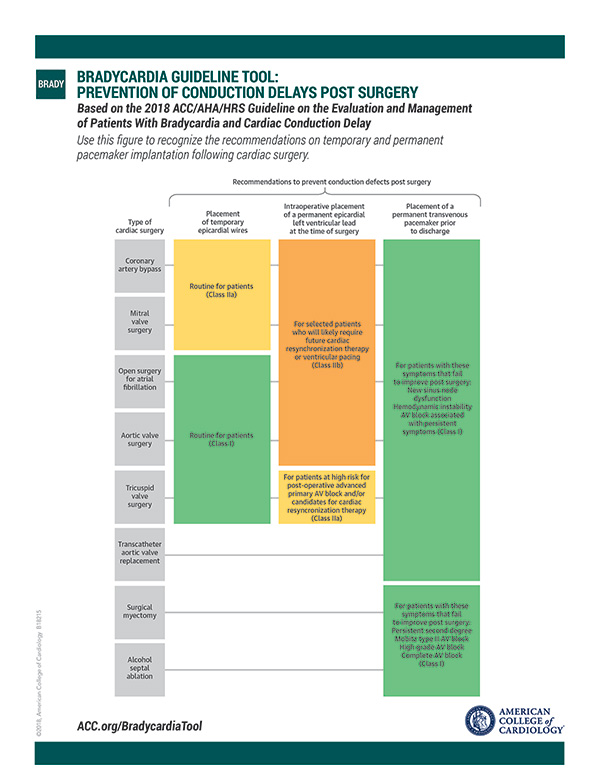
In developing the 2018 Guideline on the Evaluation and Management of Patients with Bradycardia and Cardiac Conduction Delay, the writing committee reviewed study data and developed recommendations addressing the selection and timing of diagnostic testing tools, as well as available treatment options such as lifestyle interventions, pharmacotherapy and external and implanted devices.
Read. Implement. Support Your Patients.
We've got all you need to understand the new guideline and resources and tools to put it into practice.
Visit the Bradycardia and Cardiac Delay Guideline Hub on ACC.org for the complete guideline and executive summary, slide set, podcast and perspectives.
Access the Guideline Clinical App for download to put the guideline in your pocket and download the Bradycardia Guideline Tool.
For your patients, link to the bradycardia resources on CardioSmart.org and download the hot-off-the-press bradycardia infographic.
Specifically, the guideline describes the clinical significance of bradycardia with respect to mortality, symptoms (i.e., syncope and impaired functional capacity) and exacerbations of related disorders like ischemia, heart failure and provoked tachyarrhythmias. It also aims to delineate the clinical presentation and general approach to clinical evaluation of patients with overt or suspected bradycardias or conduction diseases.
Inherited and acquired disorders of the sinus node, atrioventricular (AV) node, His-Purkinje fibers and intramyocardial conducting tissue, including the effects of medications, aging, metabolic derangements, trauma, radiation, infiltrative, ischemic and inflammatory disorders, infectious and toxic agents, and iatrogenic factors are also addressed by the new guideline.
For example, the guideline highlights that sinus node dysfunction, because it is often related to age-dependent progressive fibrosis of the sinus nodal tissue and surrounding atrial myocardium, will result in an array of different bradycardia or pause-related syndromes requiring different approaches to evaluation and management.
The guideline pays particular attention to indications for temporary and permanent pacing. For example, with sleep disorders of breathing and nocturnal bradycardias both relatively common, the guideline suggests the presence of nocturnal bradycardias is not in itself an indication for permanent pacing, but rather an opportunity to screen for sleep apnea.
However, "in patients with acquired second degree Mobitz type II AV block, high-grade AV block, or third-degree AV block not due to reversible or physiologic causes, permanent pacing is recommended regardless of symptoms." For all other types of AV blocks, the guideline recommends permanent pacing generally be considered only in the presence of symptoms that correlate with AV block. In sinus node dysfunction, establishing temporal correlation between symptoms and bradycardia is important when deciding on the necessity of permanent pacing, the writing committee states.
In other recommendations, the guideline suggests echocardiography is usually the most appropriate initial screening test for structural heart disease, including left ventricular systolic dysfunction.
In patients with AV block and left ventricular ejection fraction between 36 percent and 50 percent, who have an indication for permanent pacing and are expected to require ventricular pacing more than 40 percent of the time, the guideline recommends techniques that provide more physiologic ventricular activation (cardiac resynchronization therapy or His bundle pacing) compared with right ventricular pacing to prevent heart failure.
Recommendations on postprocedure surveillance and pacemaker implantation following transcatheter aortic valve replacement are also addressed, given the high chance of cardiac conduction abnormalities.
The writing committee also looked at special considerations for different populations based on age, comorbidities or other relevant factors. Key to addressing special considerations well: shared decision-making between the patient and clinicians, as well as patient-centered care.
"Treatment decisions are based not only on the best available evidence but also on the patient's goals of care and preferences," says Fred M. Kusumoto, MD, FACC, chair of the writing committee. "Patients should be referred to trusted material to aid in their understanding and awareness of the consequences and risks of any proposed action."
Looking ahead, the guideline also identifies knowledge gaps, pertinent trials in progress and directions for future research. In particular, the guideline stresses that more work is needed to understand how to manage bradycardia, especially the evolving role of and developing technology for pacing. Further investigations into these emerging technologies will need to occur as they are incorporated into clinical practice, the authors note.
"Identifying patient populations who will benefit the most from emerging pacing technologies, such as His bundle pacing and transcatheter leadless pacing systems, will require further investigation as these modalities are incorporated into clinical practice," Kusumoto says. "Regardless of technology, for the foreseeable future, pacing therapy requires implantation of a medical device, and future studies will be required to focus on the long-term implications associated with lifelong therapy."
Clinical Topics: Arrhythmias and Clinical EP, Cardiac Surgery, Cardiovascular Care Team, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Implantable Devices, EP Basic Science, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Cardiac Surgery and Arrhythmias, Cardiac Surgery and Heart Failure, Acute Heart Failure, Interventions and Imaging, Echocardiography/Ultrasound, Sleep Apnea
Keywords: ACC Publications, Cardiology Magazine, Atrioventricular Block, Bradycardia, Sick Sinus Syndrome, Cardiac Resynchronization Therapy, Sinoatrial Node, Transcatheter Aortic Valve Replacement, Purkinje Fibers, American Heart Association, Atrioventricular Node, Atrial Fibrillation, Iatrogenic Disease, Bundle of His, Stroke Volume, Pacemaker, Artificial, Syncope, Tachycardia, Heart Failure, Echocardiography, Sleep Apnea Syndromes, Decision Making, Writing, Comorbidity, Myocardium, Sleep Disorders, Circadian Rhythm, Patient-Centered Care, Life Style, Aging, Patient Care Planning
< Back to Listings