Cardiovascular Health in Early Life: Sign of What's to Come?
Quick Takes
- Poor cardiovascular health early in life portends worse outcomes later in life.
- Improving cardiovascular health reduces the risk of subsequent events.
- Increased focus should be placed on primordial prevention and longitudinal risk estimation practices.
While significant progress has been made in reducing the global morbidity and mortality attributable to cardiovascular disease (CVD), recent years have shown a stagnation, and in some demographics a reversal, of this progress.1 Furthermore, the mean age of patients suffering their first cardiac event is slowly decreasing. One contributor may be the increasing prevalence of cardiac risk factors beginning at younger ages.2 Obesity, diabetes, hypertension, and sedentary lifestyle are becoming increasingly prevalent early in life and are, unfortunately, not uncommon amongst pediatric and adolescent populations.3-5
This trend is especially concerning in light of our evolving understanding of how duration of risk factor exposure informs future disease risk. Studies have shown that suboptimal cardiovascular health (CVH) early in life is associated with worse CVD outcomes during follow-up and that cumulative risk factor exposure throughout the years is an independent predictor for future CVD events.6-8
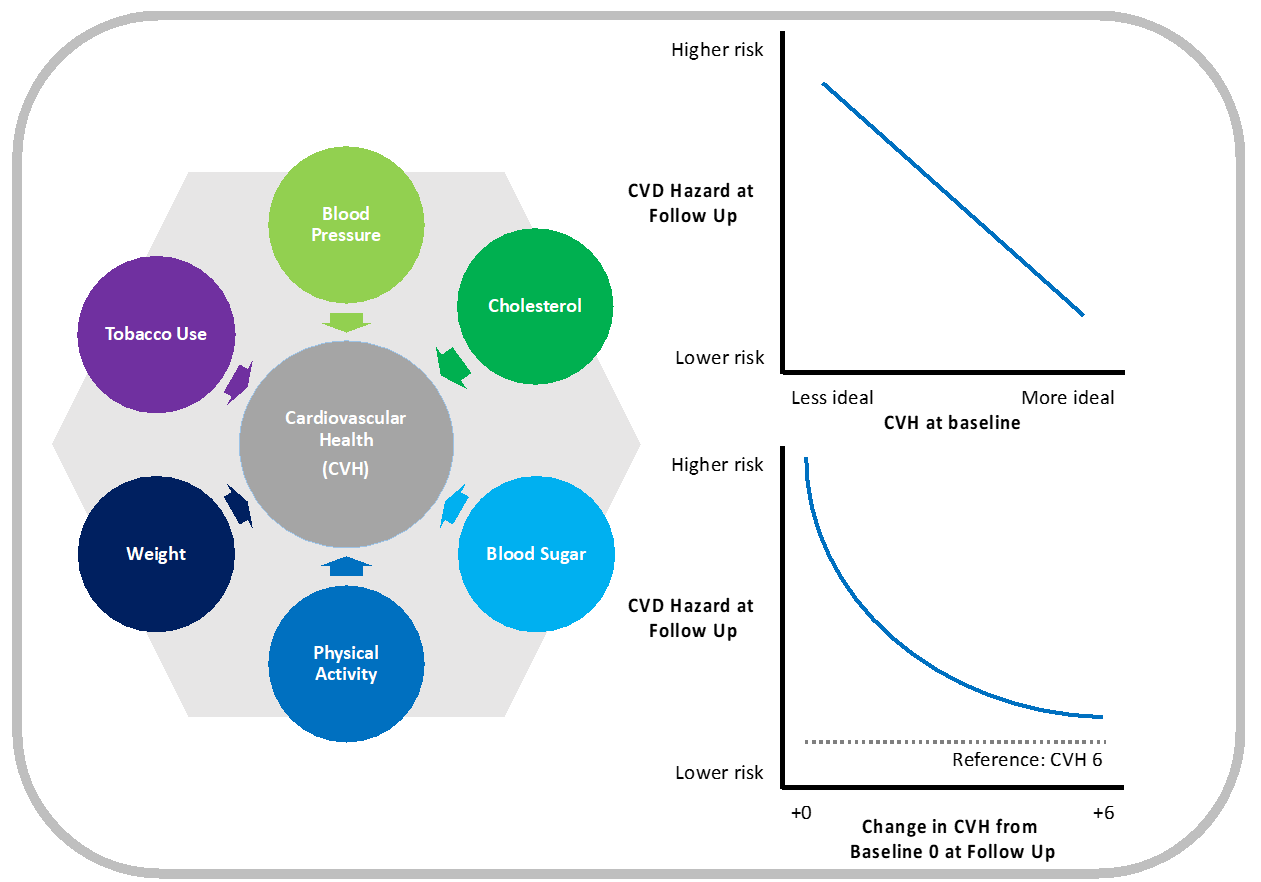
In a research letter recently published in Circulation, Lee et al.9 provide further evidence that suboptimal CVH early in life can have serious future consequences. Using the Korean National Health Insurance Service database, the authors compiled data on over 3.5 million participants aged 20-39 and stratified them by ideal CVH score. CVH scores were calculated based on a modified Life's Simple 7® score10 with one point being assigned for achieving "ideal" status on each of the 6 non-dietary components of the score (score 0 if no CVH components met, score 6 if all CVH components met). These participants, free from CVD at baseline, were followed during a median 16 years for a primary composite CVD event of first hospitalization for myocardial infarction, stroke or heart failure, or CV death.
During follow-up, a total of 39,165 CVD events were observed. Participants with higher CVH scores at baseline (indicating more ideal CVH) enjoyed lower odds of suffering a major CVD event than those with relatively worse CVH. In a multivariable adjusted model, a 30% risk reduction in CVD events was seen per 1-point increment in CVH score compared to the lowest CVH score group (hazard ratio 0.70 per 1-point higher CVH score, 95 % CI 0.70-0.71). The authors then examined a subgroup of 2.8 million participants who underwent repeat examinations 2-5 years after baseline exam and recalculated CVH scores at the second encounter. Those participants who demonstrated improvement in CVH score from their baseline enjoyed a lower hazard for CVD events than did their counterparts for whom CVH score did not change. However, participants with a low CVH score at baseline had the highest CVD risk even after attaining higher CVH scores during follow-up.
Lee and colleagues have provided evidence to suggest CVD risk estimation may be better served by adopting a framework that accounts for cumulative risk factor exposure starting in young adulthood and to consider dynamic changes during follow-up. The cumulative risk factor exposure as evidenced by worse CVH in early adulthood results in higher CVD risk. Improvement in CVH upon follow-up can result in lower incident CVD risk, although it may not completely mitigate risk among individuals with worse CVH at baseline.
Moreover, the prevailing CVD risk estimation paradigm focuses on snapshot estimations of risk based on metrics assessed at a single point in time, e.g., low-density lipoprotein cholesterol (LDL-C), blood pressure, etc. However, at subsequent clinical encounters these risk factors can change and alter the initial risk for incident CVD events.
For instance, current American College of Cardiology (ACC)/American Heart Association (AHA) guidelines on the primary prevention of CVD11 include risk-enhancing factors present early in life, such as premature menopause and other pregnancy-associated conditions that increase atherosclerotic cardiovascular disease (ASCVD) risk; however, a dynamic assessment of other traditional CVD risk factors is not contemplated. One can imagine a practice in which instead of entering only the most recent LDL-C and most recent blood pressure into a risk calculator tool, one would enter the last three to five values to produce a more precise risk estimate. There are also opportunities to apply this longitudinal perspective to other traditional risk factors, in particular those that can be modified to reduce cumulative exposure and, therefore, risk.
The findings presented by Lee and colleagues raise the question whether a longitudinal risk estimation model could yield a better CVD risk prediction than the current pooled cohort equation used in the ACC/AHA cholesterol guidelines, understanding that several risk factors are dynamic. The development of mathematical techniques to achieve this type of risk prediction are still in early stages,12 but clinicians should take a patient's high-risk history into account when counseling about future CVD risk. While further work is done to refine our understanding of risk estimation, increased efforts should be placed on primordial prevention strategies. With current estimates suggesting a mere 32% of Americans aged 20-39 achieve an ideal CVH score of 5 or more,13 much remains to be done to ensure the health of generations to come.
Figure 1
References
- Mensah GA, Wei GS, Sorlie PD, et al. Decline in cardiovascular mortality: possible causes and implications. Circ Res 2017;120:366-80.
- Agarwal S, Sud K, Thakkar B, Menon V, Jaber WA, Kapadia SR. Changing trends of atherosclerotic risk factors among patients with acute myocardial infarction and acute ischemic stroke. Am J Cardiol 2017;119:1532-41.
- Caprio S, Santoro N, Weiss R. Childhood obesity and the associated rise in cardiometabolic complications. Nat Metab 2020;2:223-32.
- Amutha A, Mohan V. Diabetes complications in childhood and adolescent onset type 2 diabetes—a review. J Diabetes Complications 2016;30:951-57.
- Song P, Zhang Y, Yu J, et al. Global prevalence of hypertension in children: a systematic review and meta-analysis. JAMA Pediatr 2019;173:1154-63.
- Domanski MJ, Tian X, Wu CO, et al. Time course of LDL cholesterol exposure and cardiovascular disease event risk. J Am Coll Cardiol 2020;76:1507-16.
- Echouffo-Tcheugui JB, Zhang S, Florido R, et al. Duration of diabetes and incident heart failure: the ARIC (Atherosclerosis Risk In Communities) study. JACC Heart Fail 2021;9:594-603.
- Perak AM, Ning H, Khan SS, et al. Associations of late adolescent or young adult cardiovascular health with premature cardiovascular disease and mortality. J Am Coll Cardiol 2020;76:2695-2707.
- Lee H, Yano Y, Cho SMJ, et al. Associations of ideal cardiovascular health and its change during young adulthood with premature cardiovascular events: a nationwide cohort study. Circulation 2021;144:90-92.
- Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic impact goal through 2020 and beyond. Circulation 2010;121:586-613.
- Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019;74:e177-e232.
- Wu CO, Tian X, Tian L, et al. Nonparametric estimation of risk tracking indices for longitudinal studies. Stat Methods Med Res 2020;29:481-97.
- Virani SS, Alonso A, Benjamin EJ, et al. Heart disease and stroke statistics—2020 update: a report from the American Heart Association. Circulation 2020;141:e139-e596.
Clinical Topics: Cardiovascular Care Team, Congenital Heart Disease and Pediatric Cardiology, Diabetes and Cardiometabolic Disease, Dyslipidemia, Heart Failure and Cardiomyopathies, Prevention, CHD and Pediatrics and Arrhythmias, CHD and Pediatrics and Prevention, CHD and Pediatrics and Quality Improvement, Lipid Metabolism, Nonstatins, Acute Heart Failure, Hypertension
Keywords: Adolescent, Child, Young Adult, Cholesterol, LDL, Cardiovascular Diseases, American Heart Association, Blood Pressure, Sedentary Behavior, Prevalence, Menopause, Premature, Pregnancy, Benchmarking, Follow-Up Studies, Data Management, Risk Factors, Myocardial Infarction, Risk Reduction Behavior, Primary Prevention, Heart Failure, Stroke, Hypertension, Hospitalization, National Health Programs, Counseling, Family Characteristics, Diabetes Mellitus, Obesity, Pediatric Obesity
< Back to Listings