There Is an Urgent Need to Re-Establish LDL-C Measurement and Control as Quality Metrics in the US Health Care System
Quick Takes
- New evidence-based guidelines and recommendations support low-density lipoprotein cholesterol (LDL-C) monitoring to assess response and adherence to therapies, as well as the value of add-on therapy for attaining recommended levels of LDL-C.
- Evidence strongly favors re-establishment of quality metrics for LDL-C measurement and control to improve population-wide cardiovascular morbidity, mortality, and health equity.
- The cardiology community must advocate for the use of such quality metrics for lipid management, similar to those currently in place for blood pressure control for patients with hypertension and glycemic control for patients with diabetes mellitus.
In a recent commentary in New England Journal of Medicine, Jacobs et al. describe a working group focused on development and implementation of a consistent approach under a "universal foundation" of quality measures across the Centers for Medicare and Medicaid Services (CMS) to focus providers' attention on those that are meaningful for the health of broad segments of the population.1 This effort is laudable.
However, conspicuously absent from the current slate of quality measures for chronic conditions are measurement and control of low-density lipoprotein cholesterol (LDL-C) levels. Atherosclerotic cardiovascular disease (ASCVD) remains the leading cause of mortality in the United States, and strong and consistent evidence exists for the efficacy of LDL-C level lowering to reduce ASCVD risk in both primary and secondary prevention.2-5 Nevertheless, inadequate LDL-C level control is common.
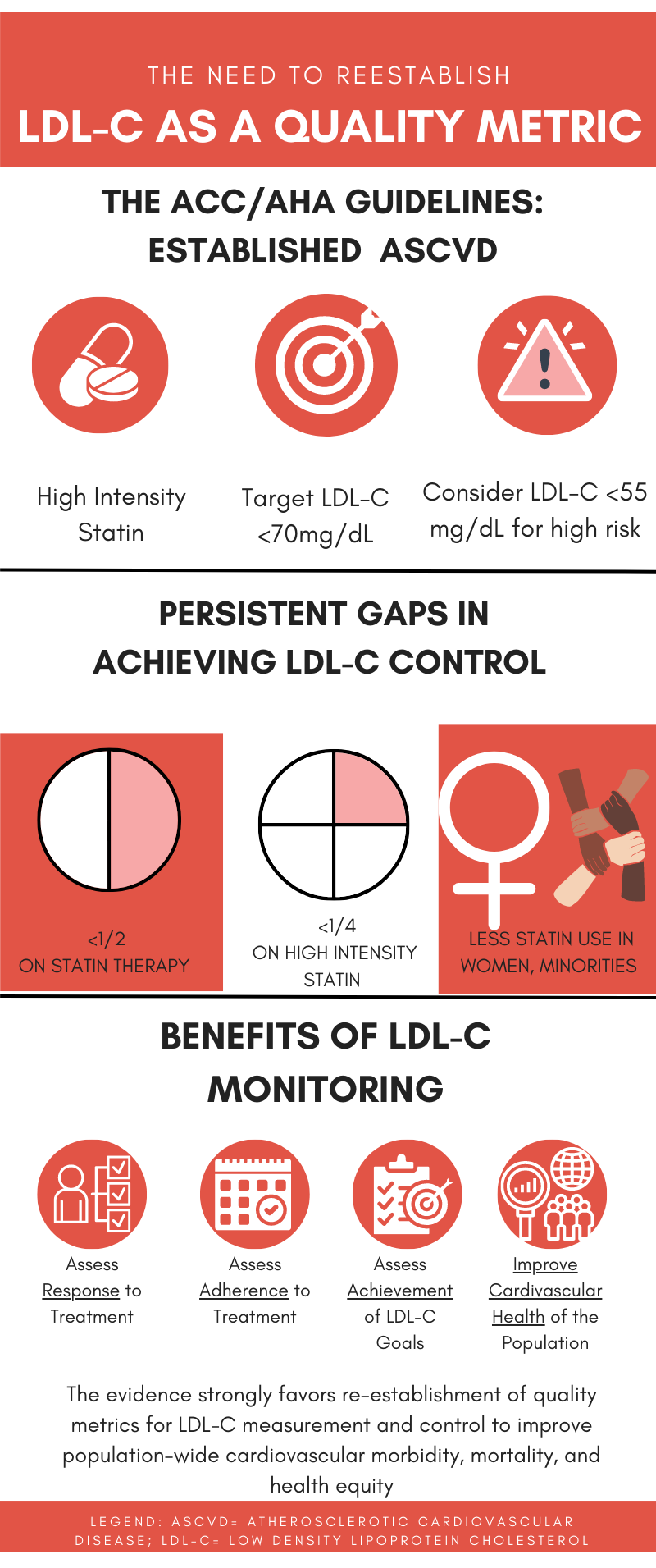
Guidelines recommend lifestyle plus high-intensity statin therapy for patients with ASCVD and the addition of nonstatin therapy if the LDL-C level remains ≥70 mg/dL.2 A 2022 American College of Cardiology (ACC) expert consensus decision pathway recommended an LDL-C threshold of ≥55 mg/dL for consideration of further intensification of LDL-C level lowering for patients with established ASCVD at the highest risk of a subsequent cardiovascular (CV) event (~50% of patients with ASCVD),6 which agrees with recommendations in the 2019 European Society of Cardiology/European Atherosclerosis Society (ESC/EAS) guidelines for management of dyslipidemia.7
In a recent survey of >600,000 patients with ASCVD in a commercial health plan, one-half were not taking a statin and only 22.5% were taking a high-intensity statin.8 In the GOULD (Getting to an Improved Understanding of Low‐Density Lipoprotein Cholesterol and Dyslipidemia Management) registry, an observational study of patients with ASCVD receiving lipid therapy at baseline between 2016 and 2018, only 17.1% had intensification of their lipid therapy after 2 years and two-thirds remained at an LDL-C level ≥70 mg/dL.9 These findings align with those from a study of health care claims and laboratory data in a representative sample of commercial and Medicare supplemental health plan participants in 2019.10 Those results indicate that, of the estimated 24 million individuals with ASCVD in the United States, 72.6% had an LDL-C level ≥70 mg/dL.10
Patient adherence and persistence with lifestyle and evidence-based medication for cholesterol management are best achieved through monitoring LDL-C levels (and non-high-density lipoprotein cholesterol levels).11 Lipid-related quality measures recommended by the National Committee for Quality Assurance (NCQA), Healthcare Effectiveness and Data Information Set (HEDIS), and CMS continue to emphasize as quality metrics only the percentage of patients in different categories (those with ASCVD, diabetes mellitus [DM], LDL-C level ≥190 mg/dL) who have been prescribed and are taking a statin during the measurement period.11
As summarized earlier, there are currently significant gaps between recommended and achieved levels of LDL-C control. These gaps are particularly large for some population subsets such as ethnic/racial minorities, women, and those with lower socioeconomic status, thus contributing to disparities in health outcomes.11 A recent clinical perspective issued jointly by the National Lipid Association (NLA) and the American Society for Preventive Cardiology (ASPC) summarized the evidence and rationale for re-establishing quality metrics for LDL-C level measurement and control for both primary and secondary prevention, especially for those with ASCVD for whom the need is most urgent.11 Key conclusions from this clinical perspective include:
- Recent data from the NCQA and independent surveys show minimal improvement in recent years regarding the use of statin therapy in individuals with ASCVD.
- Significant heterogeneity exists in the LDL-C response to statin therapy.
- Clinical trial evidence with nonstatin therapies supports the benefits of additional LDL-C level lowering in patients on statin therapy at high risk whose LDL-C levels are above recommended thresholds.
- New evidence-based guidelines and recommendations support LDL-C level monitoring to assess response and adherence to therapies, as well as the value of add-on therapy for attaining recommended levels of LDL-C.
- Advances in data analytics and the use of electronic health records allow health systems and providers to monitor LDL-C levels and prompt actions to address LDL-C level measurement and control, thus improving outcomes.
Therefore, the totality of evidence strongly favors re-establishment of quality metrics for LDL-C level measurement and control to improve population-wide CV morbidity, mortality, and health equity (Figure 1). The cardiology community is urged to advocate for the use of such quality metrics for lipid management, similar to those currently in place for blood pressure control for patients with hypertension and glycemic control for patients with DM.1
Figure 1
References
- Jacobs DB, Schreiber M, Seshamani M, Tsai D, Fowler E, Fleisher LA. Aligning quality measures across CMS - the universal foundation. N Engl J Med 2023;388:776-9.
- Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019;73:e285-e350.
- Silverman MG, Ference BA, Im K, et al. Association between lowering LDL-C and cardiovascular risk reduction among different therapeutic interventions: a systematic review and meta-analysis. JAMA 2016;316:1289-97.
- Rong S, Li B, Chen L, et al. Association of low-density lipoprotein cholesterol levels with more than 20-year risk of cardiovascular and all-cause mortality in the general population. J Am Heart Assoc 2022;Jul 29:[ePub ahead of print].
- Tsao CW, Aday AW, Almarzooq ZI, et al.; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics-2023 update: a report from the American Heart Association. Circulation 2023;147:e93-e621.
- Lloyd-Jones DM, Morris PB, Ballantyne CM, et al.; Writing Committee. 2022 ACC expert consensus decision pathway on the role of nonstatin therapies for LDL-cholesterol lowering in the management of atherosclerotic cardiovascular disease risk: a report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol 2022;80:1366-418.
- Mach F, Baigent C, Catapano AL, et al.; ESC Scientific Document Group. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J 2020;41:111-88.
- Nelson AJ, Haynes K, Shambhu S, et al. High-intensity statin use among patients with atherosclerosis in the U.S. J Am Coll Cardiol 2022;79:1802-13.
- Cannon CP, de Lemos JA, Rosenson RS, et al.; GOULD Investigators. Use of lipid-lowering therapies over 2 years in GOULD, a registry of patients with atherosclerotic cardiovascular disease in the US. JAMA Cardiol 2021;6:1-9.
- Gu J, Sanchez R, Chauhan A, Fazio S, Wong N. Lipid treatment status and goal attainment among patients with atherosclerotic cardiovascular disease in the United States: a 2019 update. Am J Prev Cardiol 2022;March 20:[ePub ahead of print].
- Virani SS, Aspry K, Dixon DL, et al. The importance of low-density lipoprotein cholesterol measurement and control as performance measures: a joint clinical perspective from the National Lipid Association and the American Society for Preventive Cardiology. J Clin Lipidol 2023;17:208-18.
Clinical Topics: Cardiovascular Care Team, Diabetes and Cardiometabolic Disease, Dyslipidemia, Prevention, Lipid Metabolism, Nonstatins, Novel Agents, Statins
Keywords: Cholesterol, LDL, Hydroxymethylglutaryl-CoA Reductase Inhibitors, Centers for Medicare and Medicaid Services, U.S., Cardiovascular Diseases, Medicaid, Medicare, Dyslipidemias, Atherosclerosis, Diabetes Mellitus, Cholesterol, Life Style, Morbidity, Registries, Socioeconomic Factors, Primary Prevention, Secondary Prevention
< Back to Listings