Prioritizing Health | Improving Delivery of Care: Decision Tools Work!

When it comes to treating cardiovascular diseases, we're fortunate to have a range of guideline-directed medical therapies (GDMT), but a persistent challenge is getting the right treatment to all the right patients at the right time – and at optimal doses.
New research from ACC.23/WCC suggests that clinical decision support tools including automated and electronic messages can help clinicians deliver guideline-recommended therapies and lead to better treatment and better clinical outcomes.
In the BETTER CARE HF trial, researchers found that prescribing of mineralocorticoid receptor antagonists (MRAs) for eligible patients with heart failure with reduced ejection fraction (HFrEF) was 2.5-times more likely if clinicians received a customized electronic health record (EHR) alert.
The three-arm, cluster-randomized study, which was also published in JACC, compared the effectiveness of two automated EHR-embedded tools to usual care in prescribing MRAs. One tool provided an alert during individual patient encounters while the other provided a message about multiple patients between encounters.
Among 2,211 patients, with an average age of 72 years and average EF of 33%, new MRA prescribing occurred in 29.6% of patients in the alert group, 15.6% in the message group and 11.7% in the usual care group.
"This shows the power of electronic tools and reminders to dramatically improve care across a wide population of patients," said Amrita Mukhopadhyay, MD. "These tools have great potential to improve prescribing and improve care, especially where we know gaps exist."
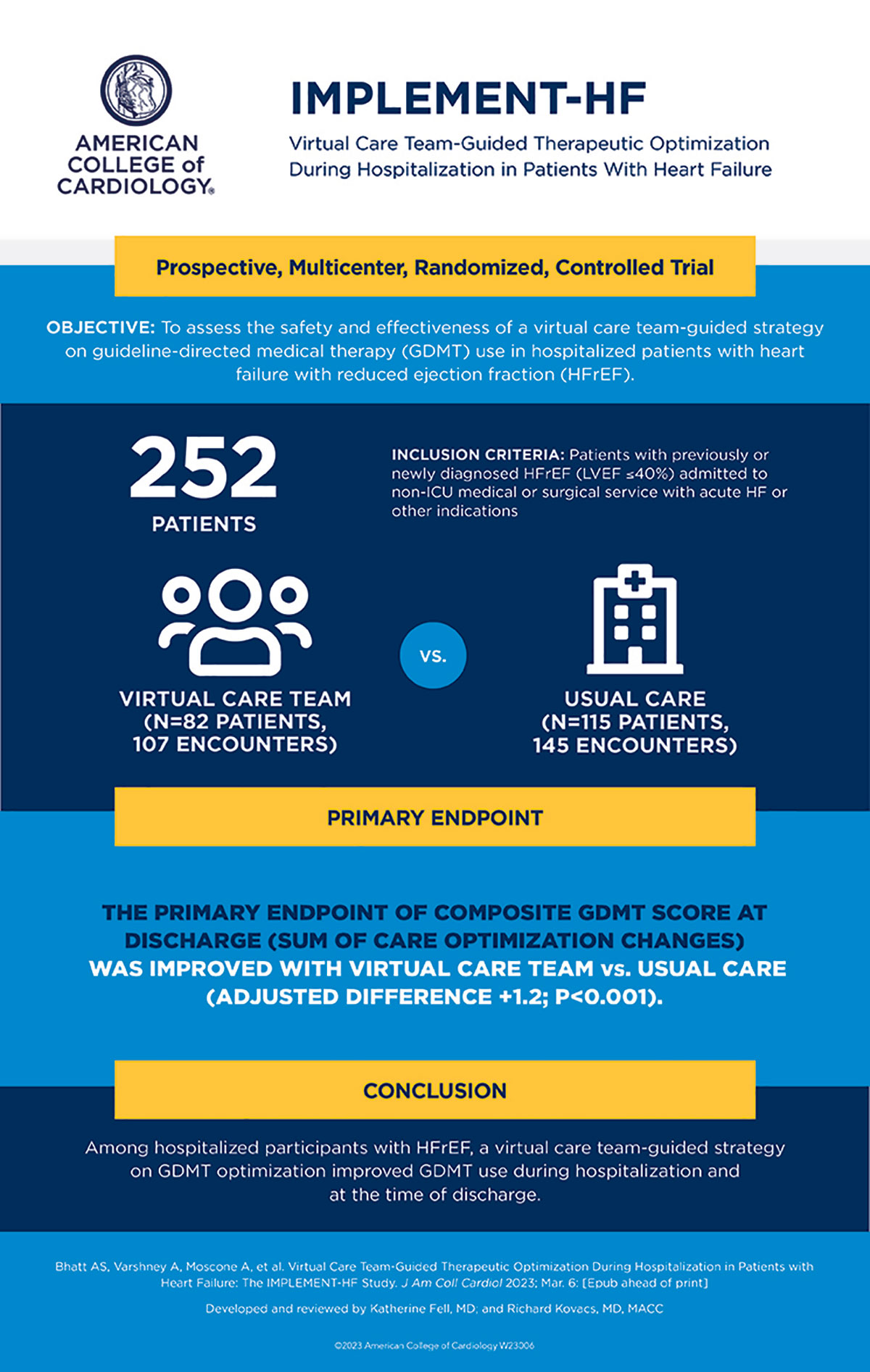
In the IMPLEMENT-HF trial, a virtual care team-guided strategy optimized the use of GDMT in patients hospitalized with HFrEF. The patients were from three centers in an integrated health care delivery system. Their mean age was 69 years, 34% were women, 14% were Black and 17% were Hispanic.
Clinicians in the virtual care team group received up to once daily recommendations for optimizing GDMT from a physician-pharmacist team. The primary goal was to improve early treatment of four major drugs classes (beta-blockers; ACE inhibitors/ARB/ARNI; MRAs; SGLT2i). Effectiveness was measured by the in-hospital change in the optimization score (+2 initiations, +1 dose uptitrations, –1 downtitrations, –2 discontinuations summed across classes), and in-hospital safety outcomes were analyzed by an independent clinical events committee.
GDMT optimization scores improved with the virtual care team strategy vs. usual care (adjusted difference +1.2; p<0.001). In these groups respectively, there was a higher rate of new initiation of GDMT (44% vs. 23%; p=0.001) and intensifications of ≥one GDMT (50% vs. 28%; p=0.001). This translated to a number-needed-to-intervene of five encounters to optimize GDMT during hospitalization.
"This strategy represents a potential highly effective, scalable intervention that can lead to accelerated implementation of guideline concordant HFrEF care," write Ankeet S. Bhatt, MD, MBA, MSc, et al., in the simultaneous publication in JACC.
Another study, PCDS Statin, showed that an automated reminder significantly improved prescribing of guideline-recommended high-intensity statin therapy in patients with atherosclerotic cardiovascular disease. The reminder included information about a patient's cardiovascular disease history, prior statin use and history of statin-associated side effects.
The study, led by Salim S. Virani, MD, FACC, used machine learning algorithms to parse clinician notes for evidence of statin-associated side effects and generate summaries of relevant patient history to create the model. Then they randomized 14 clinics (117 clinicians treating 18,427 patients) to implement the reminders and 13 clinics (128 clinicians treating 18,214 patients) to continue usual care for a 15-month period.
The primary outcome, change in high-intensity statin use between sites, increased by 3.8% across all clinics in the intervention arm compared with usual care (odds ratio, 1.06). In the intervention arm, the absolute change in the primary outcome was a 10.1% increase for those who received a reminder vs. a 0.18% decrease in those who did not. Statin adherence, a secondary outcome, was higher in the reminder group (odds ratio, 1.12).
"We found that if you're able to send reminders that have information that is personally relevant to the patient, it works," said Virani. "Our data also show it is important to be mindful of how reminders fit in with the clinical workflow to avoid creating alert fatigue."
In the NUDGE-FLU trial, reminders were shown to increase rates of flu vaccination by making a connection between the flu and risk of subsequent heart problems via an electronic letter from the physician to their patients.
Researchers randomized 964,870 Danish citizens aged 65 or older across 691,820 households to receive one of nine electronic letters, each featuring a specific message about the upcoming flu season and the need for vaccination.
The primary endpoint, getting a flu vaccine by Jan. 1, 2023, was significantly higher in the group receiving the letter vs. no letter (81% vs. 80.12%; p<0.0001). The group receiving repeated letters (one at the start of the study and one at day 14) with a general reminder to get vaccinated also saw a significant increase in vaccine uptake (80.85 vs. 80.12%; p=0.0006).
"As cardiologists, it's very interesting that just telling people that we can also prevent other downstream issues like cardiovascular outcomes was what worked the best of all the nudge strategies – even better than the reminder, which we expected would be positive," said the study's lead author Tor Biering-Sørensen, MD, MSc, MPH, PhD.
Clinical Topics: Diabetes and Cardiometabolic Disease, Dyslipidemia, Heart Failure and Cardiomyopathies, Prevention, Nonstatins, Novel Agents, Statins, Acute Heart Failure
Keywords: ACC Publications, Cardiology Magazine, ACC Annual Scientific Session, ACC23, Mineralocorticoid Receptor Antagonists, Heart Failure, Angiotensin-Converting Enzyme Inhibitors, Angiotensin Receptor Antagonists, Stroke Volume, Pharmacists, Incidence, Pharmaceutical Preparations, Adrenergic beta-Antagonists, Ventricular Dysfunction, Left, Cardiovascular Diseases, Physicians, Hispanic Americans, Dyslipidemias, Hydroxymethylglutaryl-CoA Reductase Inhibitors, Cardiologists, Vaccination, Hospitalization
< Back to Listings