From the Member Sections | Navigating Radiation Safety During Pregnancy: Practical Guidance For FITs

At the end of my first year of cardiology training, I (Melo) learned I was pregnant and faced a pivotal decision: continue with my current schedule or change my rotations to avoid radiation exposure. I had to quickly educate myself on best practices, current recommendations for fetal exposure and the experience of those with similar circumstances.
Although I had attended a lecture on radiation exposure and safety during my first year of training, I still felt I didn't know enough to make an informed decision. In fact, I had no sense of how much radiation exposure I already had because I hadn't worn a dosimeter. It turns out I'm not alone.
In a work-life survey conducted by the ACC, nearly one in three women cardiologists reported working in a department with no official policy for radiation safety in pregnancy; another one in three women were unaware of whether their department had any such policy.1
The survey also revealed that radiation reduction and surveillance strategies are underutilized during pregnancy, with only 20% reporting wearing fetal badges and 24% using additional lead protection. There is a dire need to overcome the gap in knowledge about radiation safety and implementation of radiation safety practices among trainees.
Radiation exposure is a concern for all trainees, especially for those who are pregnant or are considering pregnancy. The decision to participate in rotations with a risk of radiation exposure during pregnancy can be daunting. Trainees must balance their desire to participate in cases and procedures with their desire to minimize risk to the fetus. This decision is very challenging and personal.
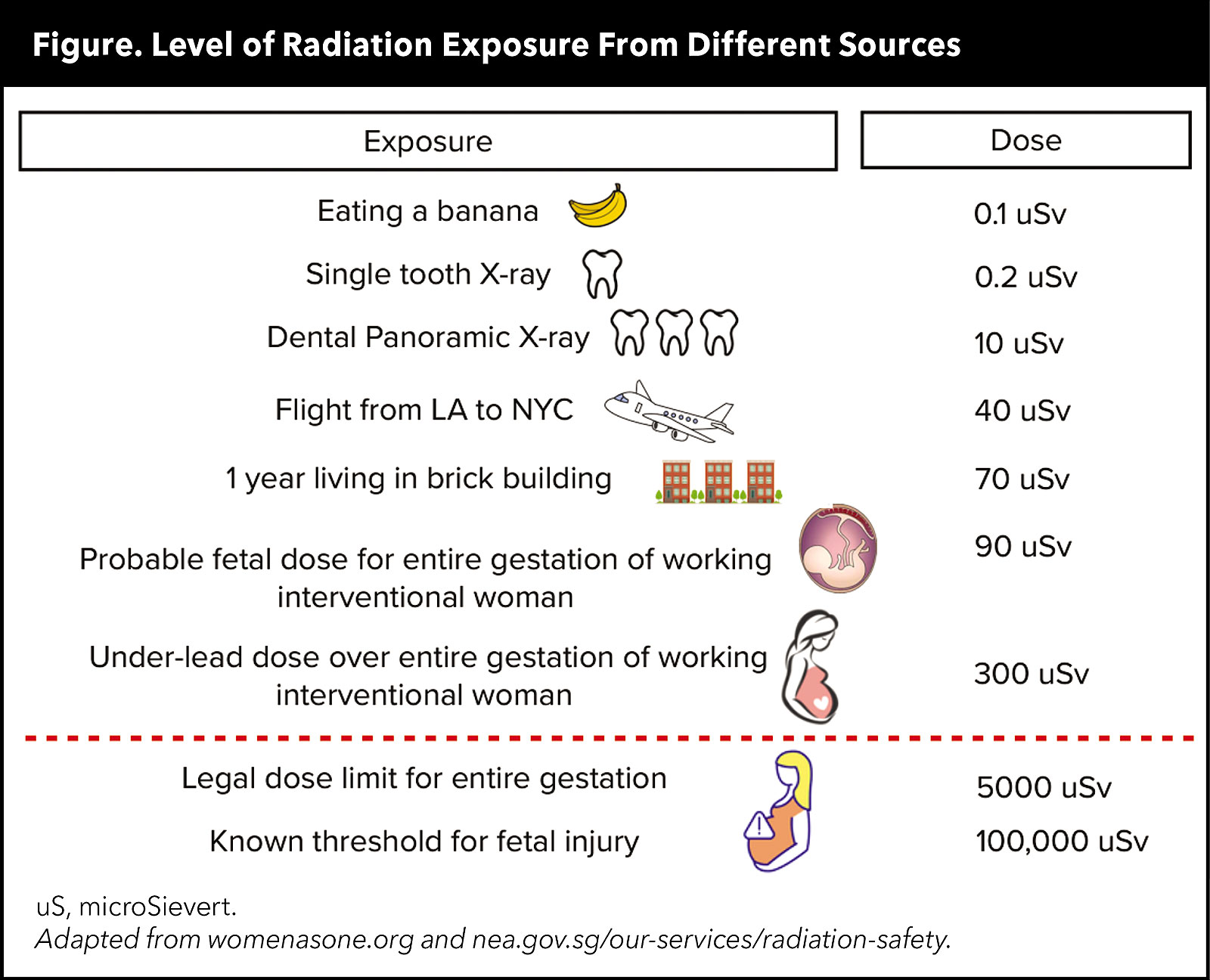
Surprisingly, fetal dose exposure is very minimal, according to data from a radiation safety module developed by Women as One (Figure).2 Furthermore, the risk of radiation exposure in the cath lab can be minimized by wearing appropriate protective gear and understanding basic radiation physics.
It's important to understand that a 0.25 mm lead apron absorbs approximately 96% of scatter radiation and a 0.5 mm lead apron absorbs about 98%. Wearing two lead aprons, also known as "double leading," can lead to musculoskeletal and back issues during pregnancy because of the added weight. To ensure tracking of potential radiation exposure to the fetus, trainees also should wear an additional dosimeter under their lead apron.
Of note, it's recommended that trainees discuss access to a dosimeter and any other concerns during pregnancy with their medical physicist and/or radiation safety officer. A dose report can be helpful in tracking monthly radiation expoure,3 and gauging the effectiveness of the lead apron.
Greater efforts should be made to increase radiation safety education and radiation exposure tracking during fellowship. Fellows can then feel empowered to make informed decisions regarding radiation exposure and practices to minimize exposure.
I chose to work in the cath lab during the second and third trimesters of my pregnancy because I had researched and reviewed the data and knew how best to mitigate potential risk. One of my proudest moments in training was answering a STEMI call at 36 weeks. While in the lab, I knew it would be a moment I would tell my daughter about one day because I felt so empowered!
Radiation Safety Tips in Pregnancy
- Notify your radiation officer about your pregnancy as early as possible to review safety measures and request a fetal dosimeter badge.
- Wear fetal monitoring badge at waist level under protective garment in addition to regular radiation badge per institution policy.
- Ensure lead apron is ≥0.5 mm lead equivalency. For pelvic protection, consider wearing additional lead (e.g., lead apron + lead skirt); be aware additional weight can increase musculoskeletal strain.
- Adjust fit of protective gear as needed throughout pregnancy.
- Track radiation exposure monthly.
- Make use of protective equipment like lead shields, lead curtains and lead wall. If available, technologies like RADPAD and EggNest systems can further minimize scatter radiation.
- Understand and optimize fluoroscopic equipment positioning to increase distance from radiation source, minimize fluoro-pedal time, and adjust frame rate, collimation and magnification.

This article was authored by Diana Melo, MD, a FIT at Stanford University in Palo Alto, CA, and Priyanka Bhugra, MD, a FIT at Houston Methodist Hospital in Texas. They are members of ACC's FIT Section. Click here to join!
References
- Sarma AA, Nkonde-Price C, Gulati M, et al. Cardiovascular medicine and society: The pregnant cardiologist. J Am Coll Cardiol 2017;69:92-101.
- Women as One. Radiation Safety in the Practice of Cardiology: What Every Woman Needs to Know. May 17, 2023. Available here.
- Best PJ, Skelding KA, Mehran R, et al. SCAI consensus document on occupational radiation exposure to the pregnant cardiologist and technical personnel. Heart Lung Circ 2011;20:83-90.
Clinical Topics: Cardiovascular Care Team, Stable Ischemic Heart Disease, Vascular Medicine, Chronic Angina
Keywords: ACC Publications, Cardiology Magazine, Pregnancy, Radiation Dosimeters, ST Elevation Myocardial Infarction
< Back to Listings