Feature | Familial Hypercholesterolemia: Clinician and Patient Insights
Hypercholesterolemia affects 12.1 percent of adults in the U.S.1 One in 250 U.S. adults have familial hypercholesterolemia (FH),2 90 percent of whom are not diagnosed. To better understand clinician and patient perspectives related to the treatment and management of dyslipidemia, the ACC conducted quantitative and qualitative surveys of both groups.
Clinician Quantitative Survey
Each week, clinicians surveyed see 54.7 patients on average, of whom they report 51.2 percent have dyslipidemia and 11.8 percent have FH. Patients with a previous myocardial infarction (MI) or coronary artery disease are identified by these clinicians as at the highest risk for cardiovascular events. Clinicians consider patients with only elevated LDL-C and no FH or other risk factors as being at low risk. They classify as moderate risk the patients with multiple cardiovascular risk factors but no documented MI and FH and no other risk factors.
The primary risk factors used by these clinicians for screening for FH are family history, LDL-C levels and physical signs (Figure 1). Lipid profiles, family history and medical history are the main tools used to determine FH, with cardiologists more likely to use lipid profiles than primary care physicians (PCPs) or Cardiovascular Team members.
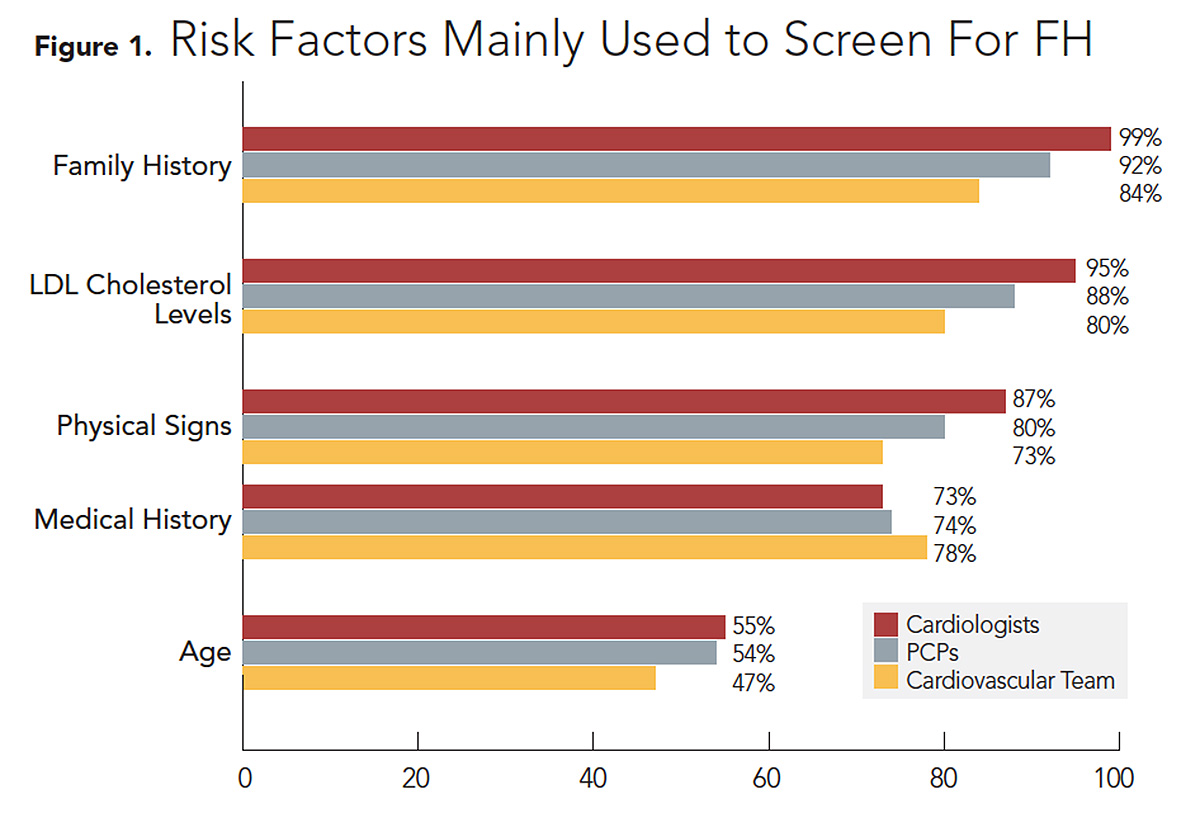
Cardiologists and Cardiovascular Team members mostly use cholesterol levels and family history to differentiate between other causes of hypercholesterolemia and FH, whereas PCPs primarily use family history and age at onset. Genotyping is used less often among each provider type, with only 24 percent of cardiologists, 26 percent of PCPs and 15 percent of Cardiovascular Team members ordering genetic testing. Only 42 percent of cardiologists, 32 percent of PCPs and 15 percent of Cardiovascular Team members conduct cascade family screening.
The clinicians identified several key issues in the management of patients with hypercholesterolemia:
- Access to care and gaps in care
- Difficulty getting insurance approval for PCSK9 inhibitors (PCSK9i)
- Lack of knowledge about diagnosis and management of FH
- Lack of education on treatments and guidelines
- Lack of familiarity with newer drugs
- Patient adherence to treatment
The top challenges in treating FH patients are cost of medication, prior authorization and insurance denials, along with underdiagnosis, among cardiologists and Cardiovascular Team members. Lack of education is cited by PCPs as their top challenge.
Regarding treatment, more than half of cardiologists (62 percent) and PCPs (61 percent) are very satisfied with the results obtained with their current treatment regimen. When asked how treatment could be improved, respondents expressed a desire for "lower cost and better availability of PCSK9i," "better reimbursement," "easier access to PCSK9i for primary prevention," "lower cost treatments," "improved continuity of care, follow-up with PCPs," and "more education for providers and patients."
Most clinicians are familiar with statins (93-99 percent), followed by ezetimibe (68-86 percent) and niacin (50-86 percent). Familiarity with PCSK9i was 70 percent among surveyed cardiologists, 41 percent of PCPs and 61 percent of Cardiovascular Team members. Clinicians are more likely to experience delays or denials for PCSK9i than statins, niacin or bile acid sequestrants (Table 1).
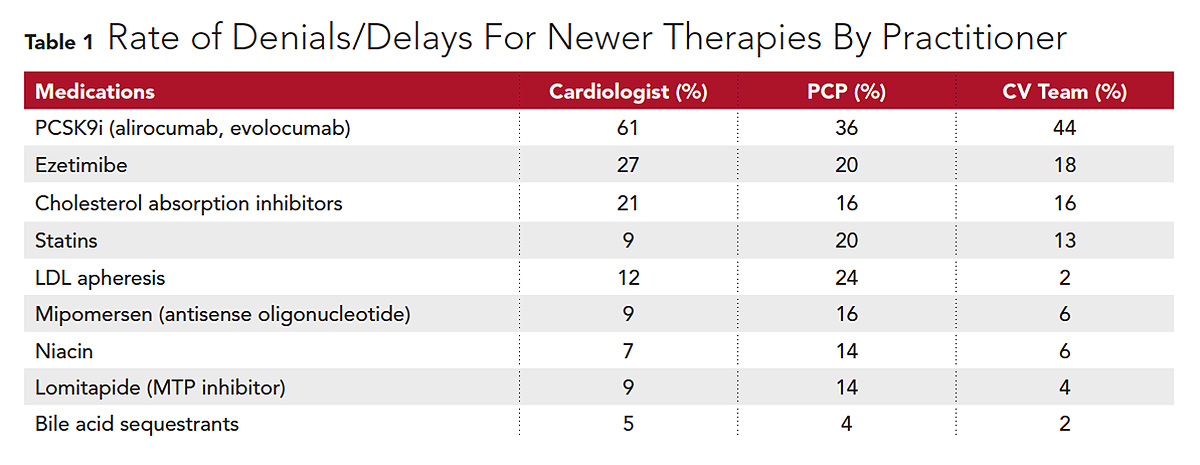
Intermittent denials for ezetimibe occur. Statins (50 percent) and PCSK9i (48 percent) are much more likely to be prescribed if clinicians do not experience denials or delays. Cardiologists are particularly more likely to prescribe PCSK9i (76 percent) and ezetimibe (65 percent) if no delays are experienced. Several clinicians stated a desire for advocacy by ACC for better access to therapies: "Lobby Congress regarding pharmaceutical costs," "Lobby for easier access to newer drugs," and "Convince insurance companies to loosen the coverage restrictions, particularly with PCSK9i."
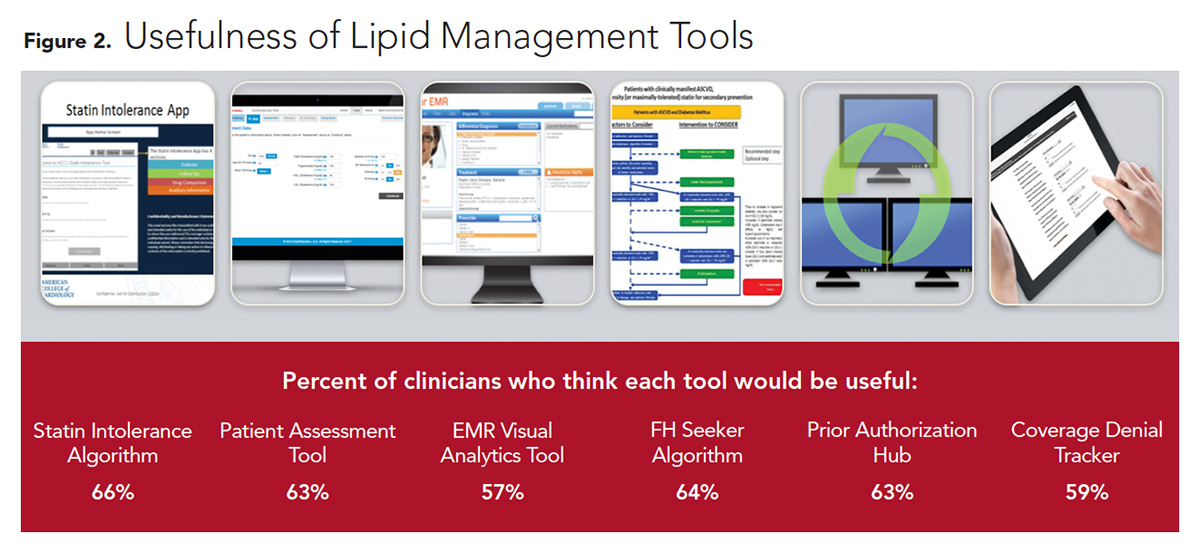
Confidence in their knowledge of FH was greater among cardiologists (52 percent) and PCPs (50 percent) than Cardiovascular Team members. The majority (74-80 percent) want to expand their FH knowledge base. "Increase educational activity at a national level about FH prevalence and cascade screening," stated one clinician. Clinicians were asked to rate the usefulness of six lipid management tools proposed by the ACC (Figure 2). The most popular were the Statin Intolerance Algorithm, FH Seeker Algorithm, Prior Authorization Hub, and Patient Assessment Tool. Clinicians also desire more patient resources.
Many clinicians expressed a desire for more FH educational support from ACC. "Raise awareness of the current appropriate diagnosis and recommended treatments," "More education on diagnosis and treatment options," "Better awareness of the incidence and diagnostic tools to help in making the diagnosis," and "Support development of lipid management tools that are deemed most useful, focusing on evidence based guidelines," are a few representative comments.
Patient Quantitative Survey
All patient respondents had been diagnosed with FH. Most FH Foundation respondents selected FH from a list of conditions without prompting (92 percent), while Research Now respondents were more likely to select FH after prompting (72 percent). Cascade screening was more commonly recommended for FH Foundation respondents (71 percent) than Research Now respondents (44 percent).
Most patients reported having to make adjustments because of their FH diagnosis, particularly taking new medications, dietary restrictions, medication side effects and health care costs. Cholesterol management is a challenge for most patients with FH, rated as extremely difficult by 36 percent of FH Foundation respondents and 14 percent of Research Now respondents. Those with the greatest difficulty are more likely to use specialists as their primary FH physician and are more likely to have had PCSK9i treatment recommended.
Ninety-five percent of respondents reported taking medication, with statins being the most prevalent. Without being aided, at least four-fifths of patients reported taking a statin to manage their dyslipidemia. After prompting, about 3 percent reported taking a statin; 5 percent reported their physician never recommended a statin as part of their treatment plan. The use of nonstatin medications is low, especially among Research Now participants (Figure 3).
While LDL-C levels were successfully lowered to below 100 mg/dL in less than half (40 percent) of FH patients, this was significantly more likely in those taking a PCSK9i. FH Foundation respondents are significantly more likely to be aware of PCSK9i, with 88 percent expressing awareness compared with 20 percent of Research Now respondents. FH Foundation respondents are also more favorable toward PCSK9i treatment vs. Research Now respondents (61 vs. 23 percent). More FH Foundation respondents (58 percent) have had PCSK9i treatment recommended by their physician compared with Research Now respondents (9 percent). Patients seeing a specialist are more likely to be prescribed a PCSK9i.
Most respondents in both populations reported being vigilant about taking their medications as prescribed. Insurance denial is an important issue for patients with FH. The FH Foundation respondents (28 percent) are twice as likely as Research Now respondents (13 percent) to have had a medication rejected by their insurance. PCSK9i were the most frequently denied medications.
The most important resources to patients for learning about and managing their hypercholesterolemia were the FH Foundation (72 percent), websites (64 percent) and clinicians (53 percent). The FH Foundation is a trusted resource primarily among its Listserv participants. Other resources selected as important are nutritionists (27 percent), handouts/pamphlets (23 percent) and textbooks (13 percent). Two-fifths of patients receive support at home to help manage their FH.
For the most part, FH Foundation and Research Now respondents rate tools similarly in terms of usefulness. The tools reported as most useful by both groups are:
- Clinical images discussed with patients and emailed to the patient or caregiver
- Decision aids focused on use of medications and procedures
- Web-based digital workbooks including embedded videos, easy-to-read checklists and quizzes
FH Foundation respondents were more likely than Research Now respondents to find value in an app that allows physicians to interactively review and discuss high cholesterol and treatment options with patients and caregivers. When asked to write down the challenges they face in managing their high cholesterol, the FH patients listed diet, side effects and costs as most significant. Other challenges include mental health, emotional impact, weight, stroke and genetics.
"This survey shows progress in FH care as well as current limitations for treatment of FH nationally," says Samuel S. Gidding, MD, a pediatric cardiologist and chief medical officer of the FH Foundation. "It is heartening that both patients and physicians are seeking more knowledge about this condition."
The FH Foundation creates a partnership between patients and providers to provide education, conduct research and advocate to make the FH care environment responsive to their needs. Responses of FH Foundation respondents in this survey reflect the value of the patient-provider partnership for education and future value of patient input into self management of FH care and FH research.
Highlights of Qualitative Research Survey
Ten health care professionals, including eight cardiologists (one lipid specialist) and two nurse practitioners were interviewed by telephone for 45-60 minutes. Interviews were also conducted among respondents in three primary audiences (cardiologists, nursing, front office) to develop a comprehensive picture of patient-practice interaction. Seventeen patients were interviewed in three focus groups in Baltimore, MD, and Tampa, FL.
The key findings of the clinician survey are:
- Tools used to identify and diagnose dyslipidemia include lipid panels, family medical history and risk screening.
- Statin therapy is the first choice to treat dyslipidemia to manage LDL-C.
- Most clinicians have had significant issues with prescribing newer therapies due to cost and insurance refusals, combined with substantial administrative time and effort.
- Gaps in care include medication costs, access to care and underdiagnoses or improper screening.
- Nonadherence to medications remains an obstacle to treatment.
- Education is considered the number one influencer of compliance.
The highlights of the patient survey are:
- Strategies for managing high cholesterol include diet, exercise, consistently taking prescribed medication, smoking cessation, keeping scheduled clinician appointments and stress management.
- Patients are generally satisfied with their current medication and did not feel that newer therapy was necessary. They also questioned the potential side effects, contraindications and cost of newer medications.
- Those at risk for FH feel they are not as educated on the condition as they would like.
- Primary challenges include managing healthy diet/exercise and taking medications.
- Their doctor is their primary trusted information source. More resources focusing specifically on their condition are desired. Favored tools are the digital booklet with its wellness strategies, number tracker and decision aids. The CardioSmart app is a favorite.
"That FH patients being seen by specialists and who are connected to the FH Foundation are more aware of their diagnosis, treatment options and the need for family screening demonstrates the value of being connected to educational resources and support," says Cat Davis Ahmed, vice president of Policy and Outreach at the FH Foundation.
References
- National Center for Health Statistics. Health, United States, 2016: With Chartbook on Long-Term Trends in Health. Hyattsville, MD. 2017.
- de Ferranti SD, Rodday, AM, Mendelson MM, et al. Circulation 2016;133:1067-72.
This research was funded by Amgen and is a component of the ACC Lipid Management Solution initiative.
Clinical Topics: Cardiovascular Care Team, Diabetes and Cardiometabolic Disease, Dyslipidemia, Prevention, Atherosclerotic Disease (CAD/PAD), Homozygous Familial Hypercholesterolemia, Lipid Metabolism, Nonstatins, Novel Agents, Primary Hyperlipidemia, Statins, Diet
Keywords: ACC Publications, Cardiology Magazine, Age of Onset, Algorithms, Bile Acids and Salts, Cardiovascular Diseases, Caregivers, Cholesterol, Continuity of Patient Care, Coronary Artery Disease, Decision Support Techniques, Dyslipidemias, Felis, Follow-Up Studies, Genetic Testing, Genotype, Health Care Costs, Diet, Hydroxymethylglutaryl-CoA Reductase Inhibitors, Hypercholesterolemia, Hyperlipoproteinemia Type II, Incidence, Knowledge Bases, Lipids, Mental Health, Medical History Taking, Myocardial Infarction, Niacin, Nurse Practitioners, Nutritionists, Pamphlets, Patient Compliance, Physicians, Primary Care, Prevalence, Primary Prevention, Qualitative Research, Risk Factors, Self Care, Smoking Cessation, Specialization, Stroke
< Back to Listings