19-Year-Old Male Athlete With Bicuspid Aortic Valve and Athletic Heart Needing Clearance Prior to Professional Soccer Tryout
|
|
Which of the following is the best option for management of this patient?
Show Answer

|
|
Show Answer
The correct answer is: G. Start beta blockade therapy, restrict from competitive sports, consider an AICD, and evaluate all first-degree relatives.
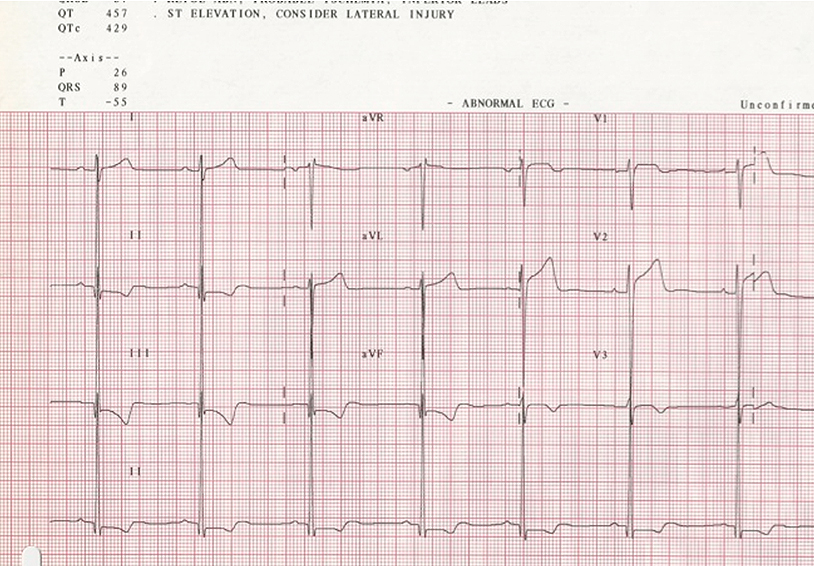
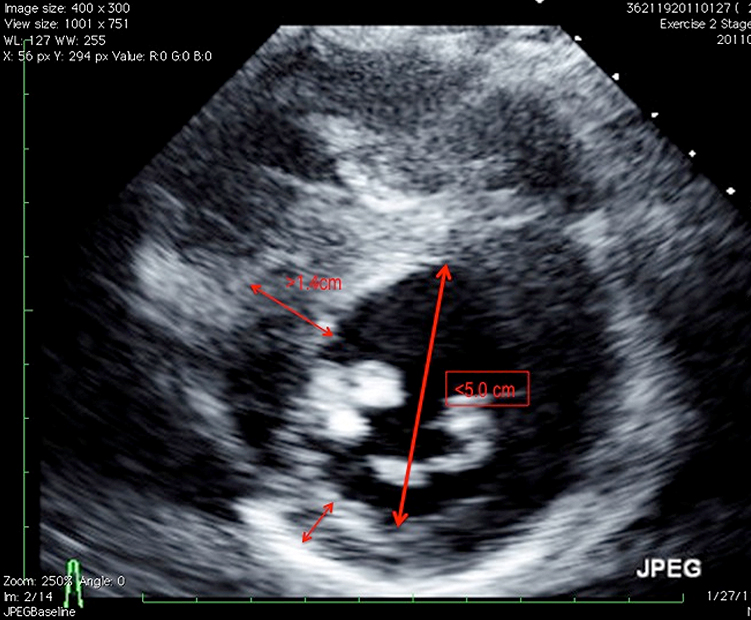
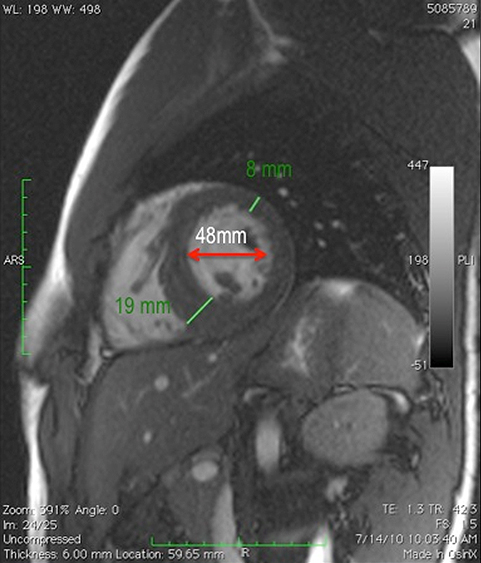
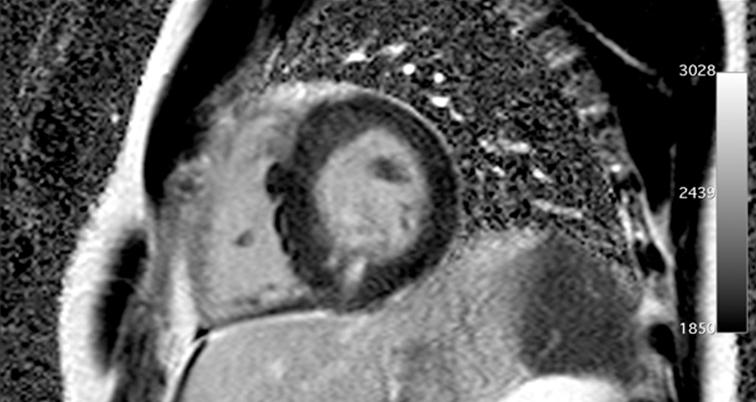
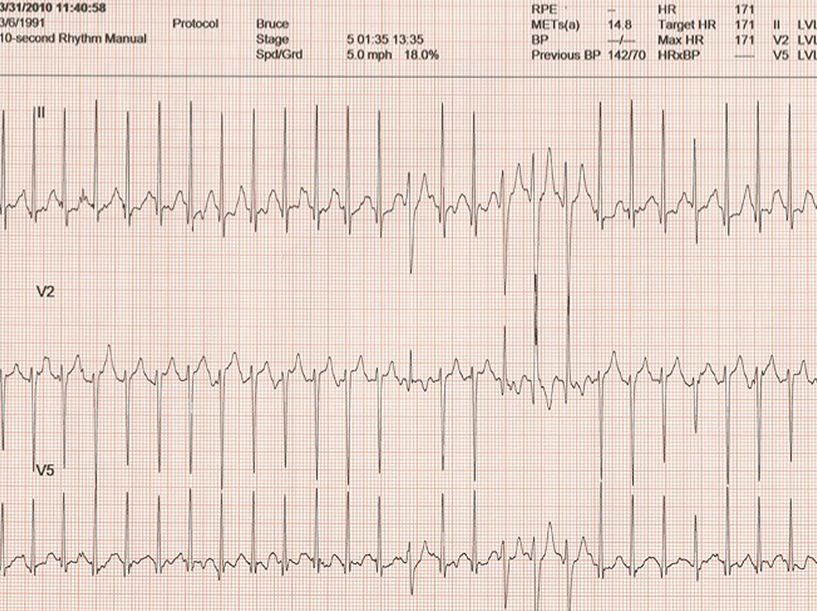
Criteria that would exclude this from being labeled as an athletic heart include unusual patterns of left ventricular hypertrophy (LVH) (asymmetric wall thickness), abnormal ECG findings (flipped T waves in inferior leads), family history of HCM, a smaller left ventricular cavity, evidence of scarring on MRI, and VT with exercise. Established guidelines clearly exclude participation in any competitive sports even with prior therapy and an ICD. Recent studies have shown that patients with an ICD can play competitive sports safely but guidelines currently in effect have not yet recognized this. Placement of an ICD in this scenario is less obvious. Risk factors for sudden death present in this patient include an abnormal blood pressure response to exercise and non-sustained VT on stress testing. ICD placement should be considered, but is not absolute. Discussion of risks and benefits of this intervention is necessary so that the patient and his family could develop an informed opinion for possible treatment. Use of beta blockade therapy is a primary treatment of HCM with symptomatic obstruction and ventricular tachycardia. Repeat stress testing in this case may guide adequacy of treatment but should not be used as another chance for sports clearance. The presence of aortic valve disease and HCM together has been reported previously. Careful evaluation of all first-degree relatives is warranted for the possibility of both diseases and all associated complications. Genetic testing may not have a definitive yield.
This case illustrates several valuable points. Clear understanding of screening ECG abnormalities indicative of myocardial disease is essential. Familiarity with standardized criteria (such as the Seattle criteria), though not perfect will improve disease detection and limit false-positive results. The degree of the LVH needs to be proportional to the amount of aortic stenosis. Abnormal patterns of LVH that are not concentric such as varying wall thickness as seen here should trigger further suspicion and testing. The type of sport and conditioning must be taken into consideration when assessing ventricular size and wall thickness. A period of deconditioning followed by repeat evaluation may clarify the diagnosis. The MRI has become routine in the evaluation of HCM. As shown above, MRI confirmed the abnormal echo findings and revealed delayed gadolinium enhancement suggestive of fibrosis. When present independently, these complex pathologies vary both in presentation and expression of disease. Deciphering the etiology becomes more daunting, due to the presence of multiple diseases.
References
© 2026 American College of Cardiology Foundation. All rights reserved.