A 49-year-old otherwise healthy male presented to an outside hospital with sudden onset of chest pain. Pain started the night prior while the patient was resting. He says that he had a stressful day at work as an IT specialist. Pain was substernal and across entire chest with a "squeezing" feeling. It did not radiate outside of his chest. He denies having similar symptoms prior to this episode. The pain was increased with deep breaths or excessive movement. Other than a 45- minute commute to the suburbs each day for work, he denies any recent travel. He denies any recent illnesses. He recently started playing in a tennis league but denies any recent injuries. He tried Tylenol and some over the counter antacids without relief. He presented to the emergency department the next morning when CP had not resolved overnight.
Review of Systems
Negative for shortness of breath, dizziness/lightheadedness, syncope, diaphoresis, nausea/vomiting, recent fever/chills, night sweats. Positive for 40 lbs weight loss over the past 6 months.
Social history:
He has been intermittently exercising 2-3 times weekly. He smokes half a pack of cigarettes a day. He has a past history of cocaine use.
Family history:
Father had myocardial infarction at age of 60.
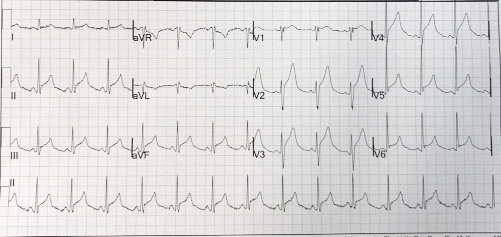
On physical exam the patient seemed uncomfortable. Vital signs showed temp 98F, BP 114/60 mmHg, HR 80 bpm, RR 20/min, SPO2 100% on RA. ECG is shown in Figure 1. CXR was normal. Labs: BUN 16, Cr 0.5. CBC 5, Hgb13, Plt 170. Troponin: 0.021 ng/mL (normal 0-0.05).
ECG is shown in Figure 1. The patient underwent an emergent coronary angiogram which demonstrated moderate lesions in the mid LAD and mid RCA which were negative by fractional flow reserve. A transthoracic echocardiogram showed normal left ventricular ejection fraction, no pericardial thickening or effusion.
Additional labs showed: Hep C Antibody Neg, HIV negative, TB Quantiferon negative, ANA undetectable, CRP 6.5 (normal 0-0.8) TSH 0.02 (normal 0.35-4), FT4 5.0 (normal 0.6-1.7), FT3 15.0 (normal 2.4-4.2).
Figure 1: Initial Presenting ECG
The correct answer is: E. Thyroiditis.
This is a rare case of a patient with a new diagnosis of Graves' disease complicated by acute pericarditis who initially presented with symptoms concerning for acute coronary syndrome. The patient had very low TSH levels and high FT3 and FT4 levels. In addition, the patient had a positive assay for TPO (thyroperoxidase antigen). A thyroid ultrasound showed hypoechogenicity and intense vascularity of thyroid goiter consistent with Graves' disease. The patient was started on methimazole for Graves' disease. He also began treatment for pericarditis with colchicine 0.6 mg twice a day and ibuprofen 800 mg three times a day.
Hyperthyroidism has major effects on the cardiovascular system including association with atrial fibrillation and heart failure. Acute pericarditis as a complication of hyperthyroidism is less known; however, acute pericarditis has been identified as a rare complication of thyrotoxicosis. A few case reports have noted the co-existence of Graves' thyrotoxicosis and pericarditis. The earliest cases were reported in 1958. As of recently there are about 20 case reports suggesting a relationship between pericardial disease and hyperthyroidism. A clear mechanism of the association between the two diseases has not been identified. However, an autoimmune process where autoantibodies involved in Graves' disease initiate an inflammatory process with the pericardium is thought to be involved.
After initiation of the above treatment, the patient had complete resolution of chest pain in the first week. A repeat ECG in the cardiology clinic was normal without any ST or T-wave abnormalities. He continues to remain symptom free 4 months later and has returned back to his normal activities.
References
- Airel PS, Steele MB, Lin AH, Seidensticker DF, Shwayhat AF. Pericarditis, thymic hyperplasia, and Graves' thyrotoxicosis: case report and review of the literature. Mil Med 2013;178:e865-9.
- Chhabra L, Spodick DH. A comment on thyrotoxic pericarditis. Int J Cardiol 2014;173:587.
- Clarke NR, Banning Ap, Gwilt DJ, Scott AR. Pericardial disease associated with Grave's thyrotoxicosis. QJM 2002;95:188-9.
- Gupta P, Chihabra L, Hiendlmayr B, Spodick DH. Thyrotoxic pericarditis: an underappreciated phenomenon. Int J Cardiol 2015;198:32-3.
- Inami T, Seino Y, Goda H, et al. Acute pericarditis: unique comorbidity of thyrotoxic crisis with Graves' disease. Int J Cardiol 2014;171:e129-30.
- Sugar SJ. Pericarditis as a complication of thyrotoxicosis. Arch Intern Med 1981;141:1242.
- Treusch JV, Jaffe HL. Hyperthyroidism associated with presumptive acute pericarditis; a report of three cases. Calif Med 1958;89:217-21.