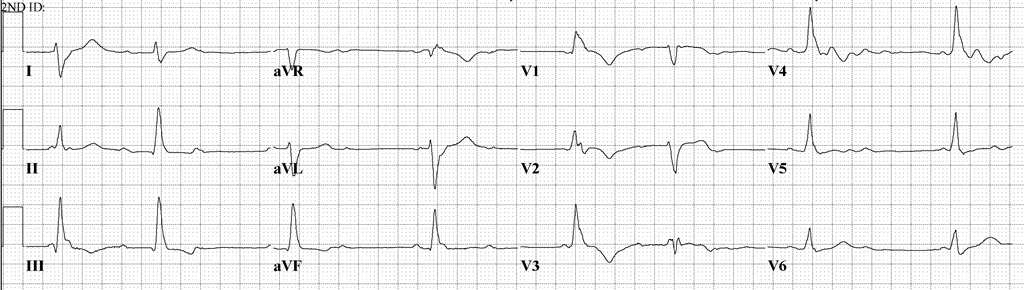
A 68-year-old man with no significant cardiac history undergoing chemo-radiation for esophageal cancer with pembrolizumab, carboplatin, and paclitaxel presented to the emergency department with new onset right eyelid drooping, double vision, generalized weakness, and achiness. Review of systems was negative for chest pain, dyspnea, orthopnea, syncope, and pedal edema. Initial examination, however, revealed bradycardia in the 40s with a new high-degree atrioventricular block seen on electrocardiogram (ECG) (Figure 1).
Figure 1
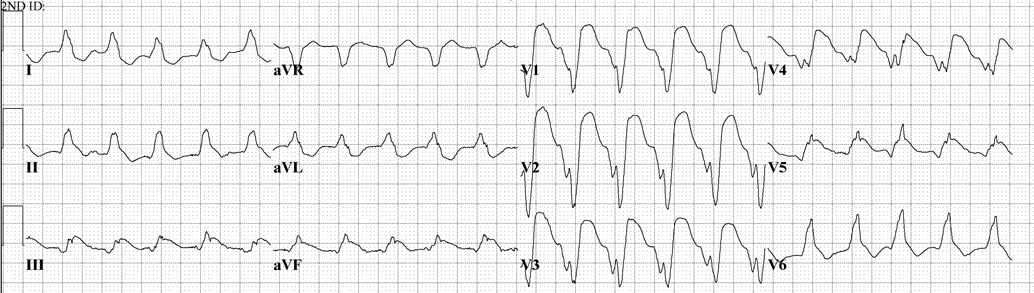
Serum cardiac troponin T was elevated at 2.1 ng/ml. Transthoracic echocardiogram (TTE) was normal, with an ejection fraction (EF) of 61%, and coronary angiography was without obstructive disease. Cardiac magnetic resonance imaging (MRI) showed a normal left ventricular EF and no other abnormality. Autoimmune serology revealed elevated anti-striated muscle and indeterminate anti-heart antibody titers. An electromyography-directed biopsy of the left biceps showed a focal perimysial lymphohistiocytic infiltrate with myofiber necrosis. Head MRI showed pituitary gland inflammation. He subsequently developed multiple episodes of slow ventricular tachycardia alternating with complete heart block, requiring the insertion of a permanent pacemaker (Figure 2).
Figure 2
His troponin peaked at 3.1 over the next week. A repeat TTE showed an EF of 37% with global hypokinesis. A repeat cardiac MRI showed decreased EF but still without significant inflammation.
The correct answer is: C. Initiate therapy with intravenous steroids
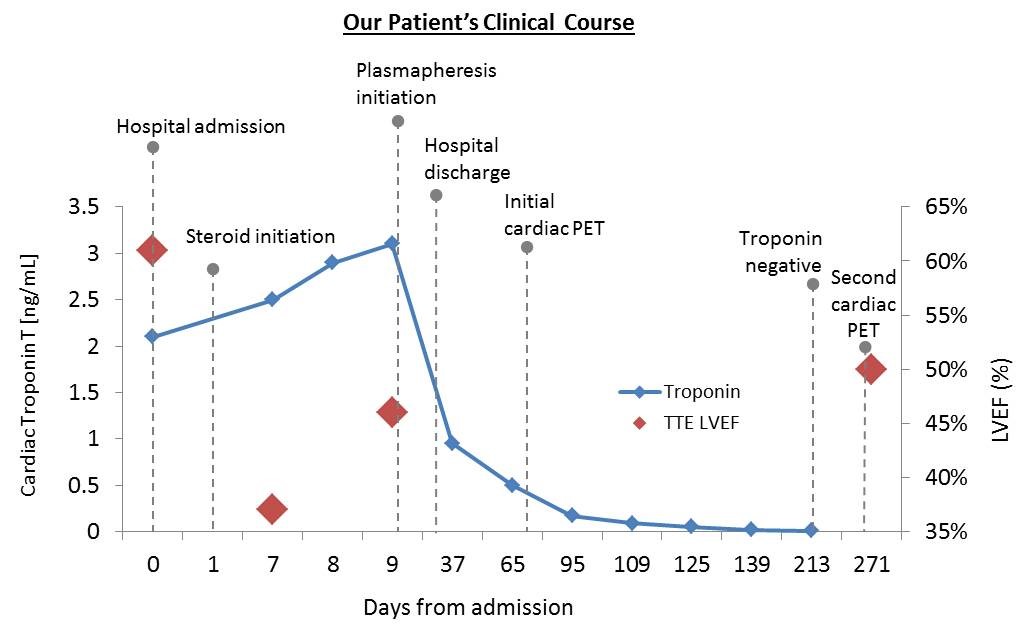
This patient had hypophysitis, myositis, and myocarditis associated with pembrolizumab use. Pembrolizumab and other immune checkpoint inhibitors are a relatively new class of antibody-based anti-cancer therapies that are associated with immune-related adverse events. These include myocarditis, pneumonitis, colitis, nephritis, hepatitis, thyroiditis, and hypophysitis. Patients with pembrolizumab-related myocarditis can have no cardiac symptoms until life-threatening complications evolve, as in this case. This patient's bradycardia was incidentally noted when he presented with neurologic symptoms; ECG changes and elevated troponin were subsequently recognized. Cardiac MRI was indeterminate for myocarditis, as was his anti-heart antibody titer due to very high levels of striated muscle autoantibodies. Cardiac positron emission tomography (PET), however, was consistent with myocarditis, and the inflammatory activity on PET decreased in tandem with declining troponin levels. High-dose steroids are the first line of therapy and should be considered early in the setting of unexplained myocarditis and check point inhibitor use. In this case, clinical recovery was not noted until initiation of plasmapheresis despite initial steroid use (Figure 3). Likewise, recent reports in the literature point out that some patients may require more aggressive immunosuppressive therapy or even mechanical circulatory support device therapy as a bridge to recovery. Though rare, the risk of evolution to life-threatening, fulminant myocarditis warrants serial cardiac surveillance measures such as cardiac troponin and ECG in patients using immune checkpoint inhibitors.
Figure 3
References
- Mahoney KM, Rennert PD, Freeman GJ. Combination cancer immunotherapy and new immunomodulatory targets. Nat Rev Drug Discov 2015;14:561-84.
- Marrone KA, Ying W, Naidoo J. Immune-Related Adverse Events From Immune Checkpoint Inhibitors. Clin Pharmacol Ther 2016;100:242-51.
- Johnson DB, Balko JM, Compton ML, et al. Fulminant Myocarditis with Combination Immune Checkpoint Blockade. N Engl J Med 2016;375:1749-55.
- Nishimura H, Okazaki T, Tanaka Y, et al. Autoimmune dilated cardiomyopathy in PD-1 receptor-deficient mice. Science 2001;291:319-22.
- Ahamadi M, Freshwater T, Prohn M, et al. Model-Based Characterization of the Pharmacokinetics of Pembrolizumab: A Humanized Anti-PD-1 Monoclonal Antibody in Advanced Solid Tumors. CPT Pharmacometrics Syst Pharmacol 2017;6:49-57.
- Arangalage D, Delyon J, Lermuzeaux M, et al. Survival After Fulminant Myocarditis Induced by Immune-Checkpoint Inhibitors. Ann Intern Med 2017;167:683-4.