Redevelopment of Pulmonary Artery Hypertension With Resumption of Dasatinib
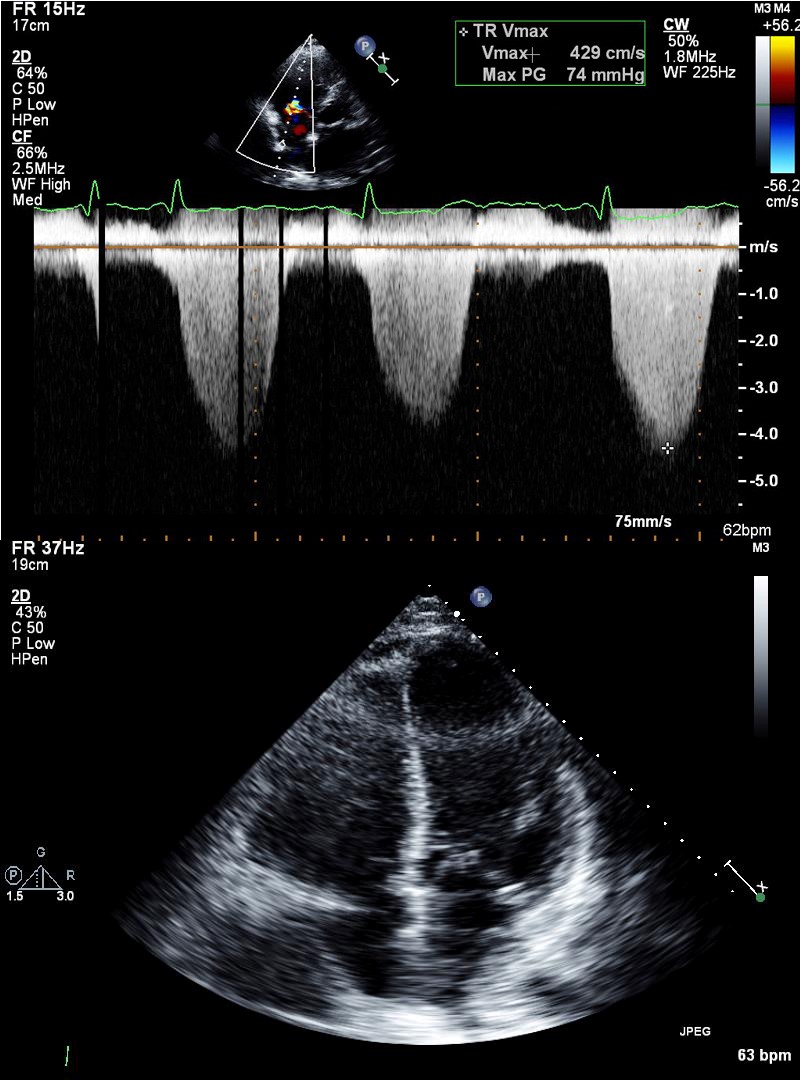
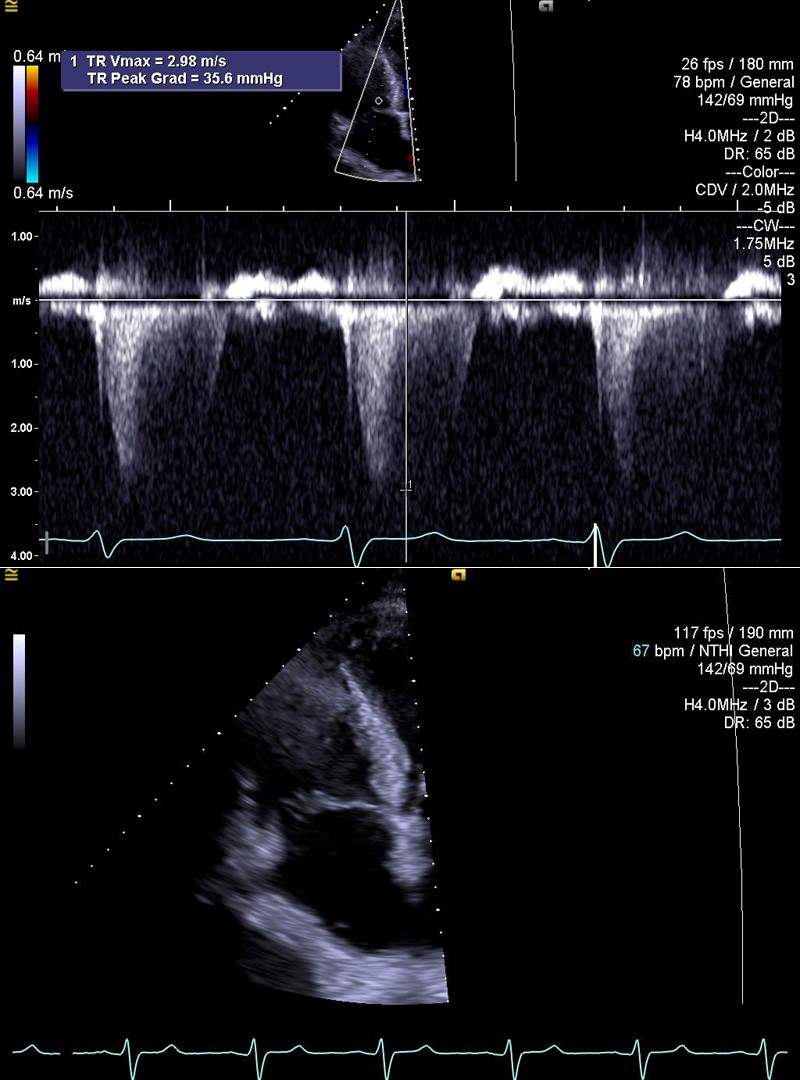
A 75-year-old male patient with a medical history of coronary artery disease and chronic myeloid leukemia being treated with dasatinib presented with worsening fatigue and dyspnea on exertion. Review of systems was positive for new bilateral lower extremity swelling. Physical examination revealed jugular venous distention and bilateral crackles at the lung bases. Chest x-ray revealed small bilateral pleural effusions. Transthoracic echocardiography (TTE) revealed ejection fraction of 40-45%, moderately to severely enlarged right ventricle (RV) with moderately reduced RV systolic function and severely elevated pulmonary artery systolic pressure of 100 mmHg (Figure 1). These findings were new from a previous TTE performed 10 months prior to presentation. After consultation with the oncology team, the patient's dasatinib was discontinued. A TTE performed 1 month later demonstrated an ejection fraction of 45-50%, mildly to moderately enlarged RV, mildly reduced RV function, and pulmonary artery systolic pressure of 40 mmHg (Figure 2).
Figure 1
Figure 2
Following this episode, the patient was started on a lower dose of dasatinib because his initial symptoms were attributed to systolic heart failure. He presented again 7 months later with dyspnea and lower extremity swelling. TTE at that time demonstrated an ejection fraction of 55-60%, mildly reduced RV function, and pulmonary artery systolic pressure of 119 mmHg.
Considering the presentation above, what is the likely etiology of the patient's pulmonary hypertension?
Show Answer