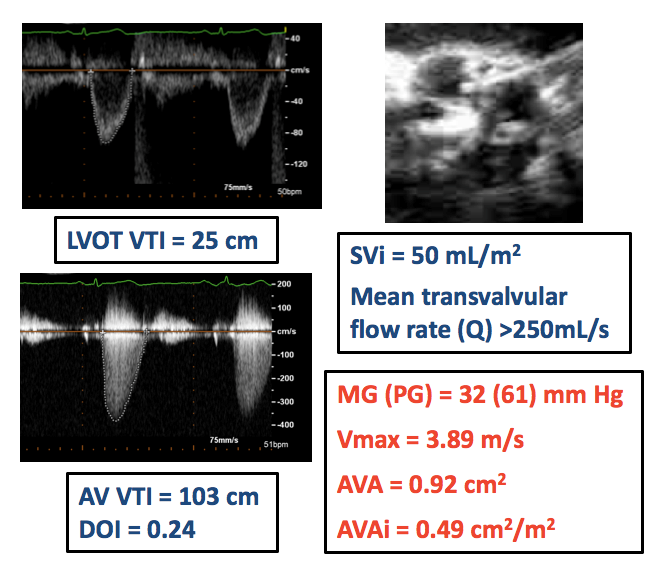
A 77-year-old female patient presents with progressively worsening dyspnea on exertion for the past year. She is symptomatic after walking half a block and has orthopnea, paroxysmal nocturnal dyspnea, and increasing lower extremity edema. She reports no chest pain or syncope. Her history is notable for prior coronary artery bypass surgery and hypertension. She is on optimal medical therapy, and her blood pressure is controlled. On exam, she has a harsh mid-peaking systolic murmur at the base, clear lung fields, and bilateral lower extremity pitting edema. Her B-type natriuretic peptide is 224 pg/mL. A transthoracic echocardiogram (TTE) shows a preserved left ventricular ejection fraction (LVEF) of 65%, diastolic dysfunction, and a calcified aortic valve (AV). Accompanied Doppler findings are outlined in Figure 1. Coronary angiography shows patent grafts and no obstructive disease. Invasively, her left ventricular end-diastolic pressure is 28 mmHg, and mean AV gradient is 33 mmHg. Despite judicious blood pressure control and diuresis, she remains symptomatic.
Figure 1
The correct answer is: C. Calcium score of the AV
The most reasonable next step is to obtain an AV calcium score, which is useful in confirming the severity of aortic stenosis (AS) when there is discordant grading (i.e., small AV area with low mean gradient [MG]) and normal flow.
The patient's TTE findings show a preserved LVEF and normal stroke volume index but discordant grading (i.e., small AV area and low MG) in the severity of her AS. This phenomenon is referred to as normal-flow, low-gradient severe AS. It is the most prevalent form of low-gradient severe AS because the two types of low-flow states (classical and paradoxical low-flow) represent only half of all patients with low-gradient AS.1,2
Determining whether normal-flow, low-gradient AS is a moderate form of AS or severe AS can be challenging and is sometimes a matter of debate. For example, up to 30% of patients with AS have incongruity in the cut-points for severe AS at TTE (i.e., AV area <1.0 cm2 but MG or Vmax consistent with non-severe stenosis).3 Within the normal-flow, low-gradient subset, overlaps between moderate and severe classes exist, but it is estimated that 40-50% of normal-flow, low-gradient patients have true severe AS.4
Normal-flow, low-gradient AS is defined by an AV area <1.0 cm2, MG <40 mmHg, and LVEF >50% with normal flow (stroke volume index >35 mL/m2). Such a pattern of AS may occur as a result of normal stroke volume but reduced arterial compliance and systolic hypertension. Other factors include the incongruity in the AV area/MG severity criteria proposed in the guidelines (for example, AV area 1.0 cm2 = MG ~30 mmHg; MG 40 mmHg = AV area ~0.8 cm2) and reduced mean transvalvular flow rate due to a prolonged left ventricular ejection time.5,6 In this case, both the patient's systolic hypertension and reduced systemic arterial compliance, at least in part, explain the discordant grading.
Key steps in evaluating for normal-flow, low-gradient AS include first ruling out measurement errors and ensuring correct estimation of stroke volume, AV area, and/or MG. Commonly, errors may occur with an oblique measure of the left ventricular outflow tract diameter, pulsed-wave Doppler sampling too close to the AV, subvalvular flow acceleration due to a septal bulge, improper left ventricular outflow tract velocity-time integral tracing, and failure to perform multi-window valve interrogation with continuous-wave Doppler while ensuring proper alignment with the direction of transaortic flow. The second step is to assess for the presence of symptoms because it is reasonable to pursue conservative management and close follow-up in asymptomatic patients. The third step is confirming stenosis severity. In the current American College of Cardiology and American Heart Association guidelines, no specific recommendation is given for symptomatic patients with normal-flow, low-gradient severe AS, but the 2017 European Society of Cardiology and European Association for Cardio-Thoracic Surgery guidelines recognize this entity and suggest an integrative approach to confirm severity.6
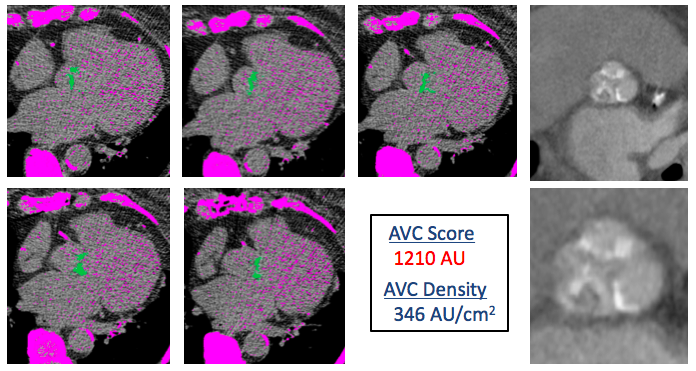
In this case, answer D is incorrect because the patient has New York Heart Association Class III symptoms despite efforts at continued medical therapy. With her ongoing symptoms, a treadmill stress test would also be of no added benefit, making answer A incorrect as well. Utilizing low-dose dobutamine stress echocardiography in the setting of a low-flow status (stroke volume index ≤35 mL/m2) or low mean transvalvular flow rate (Q = SV ÷ left ventricular ejection time) can be used to differentiate true-severe from pseudo-severe stenosis. However, this patient's mean transvalvular flow rate is normal (>250 mL/s). Thus, dobutamine stress echocardiography has limited utility, making answer B incorrect. Answer E is incorrect because the severity of the patient's AS must first be confirmed before referral for AV replacement. This may be done with calcium scoring of the AV by multi-detector computed tomography (Figure 2) and should be considered. AV calcium scoring is done using the modified Agatston method. Cut-point values used to identify severe AS in men are ≥2,000 AU and ≥1,200 AU in women.6,7 These criteria have been shown to be strongly associated with hemodynamic severity and outcomes.8
Figure 2
In summary, normal-flow, low-gradient AS is a heterogeneous entity and represents a moderate-to-severe form of AS. Clinical judgement is often needed, and making this determination can be challenging. Hence, when assessing a patient who is symptomatic, additional quantitative imaging is crucial to confirm the severity of stenosis. In this case presentation, the patient's AV calcium score was borderline, but it was ≥1,200 AU, and other findings were consistent with severe AS. Ultimately, it was felt that AV replacement was warranted.
References
- Clavel MA, Magne J, Pibarot P. Low-gradient aortic stenosis. Eur Heart J 2016;37:2645-57.
- Clavel MA, Burwash IG, Pibarot P. Cardiac Imaging for Assessing Low-Gradient Severe Aortic Stenosis. JACC Cardiovasc Imaging 2017;10:185-202.
- Berthelot-Richer M, Pibarot P, Capoulade R, et al. Discordant Grading of Aortic Stenosis Severity: Echocardiographic Predictors of Survival Benefit Associated With Aortic Valve Replacement. JACC Cardiovasc Imaging 2016;9:797-805.
- Clavel MA, Guzzetti E, Annabi MS, Salaun E, Ong G, Pibarot P. Normal-Flow Low-Gradient Severe Aortic Stenosis: Myth or Reality? Structural Heart 2018;2:180-7.
- Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014;63:2438-88.
- Baumgartner H, Falk V, Bax JJ, et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J 2017;38:2739-91.
- Clavel MA, Messika-Zeitoun D, Pibarot P, et al. The complex nature of discordant severe calcified aortic valve disease grading: new insights from combined Doppler echocardiographic and computed tomographic study. J Am Coll Cardiol 2013;62:2329-38.
- Tastet L, Enriquez-Sarano M, Capoulade R, et al. Impact of Aortic Valve Calcification and Sex on Hemodynamic Progression and Clinical Outcomes in AS. J Am Coll Cardiol 2017;69:2096-8.