Small Heart, Big Problem
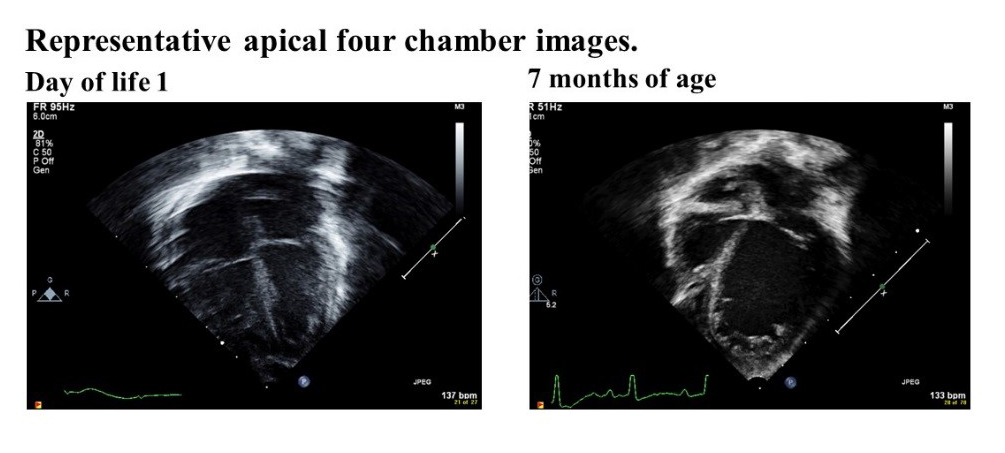
A full-term male infant with Apgar scores of 6 and 9 developed duskiness at 40 mins of life and was subsequently determined to have an enlarged liver. Initial evaluation included a complete blood count with a white blood cell count of 180 x 109/L (6% neutrophils, 4% lymphocytes, 1% myelocyte, 2% nucleated red blood cells, and 87% blasts), Hemoglobin of 10.6 g/DL, hematocrit of 33%, and platelet count of 102,000/mL of blood, concerning for neonatal leukemia. Blood smears demonstrated undifferentiated leukemia, most likely acute myeloid leukemia. Prechemotherapy echocardiogram on day of life 1 demonstrated normal intraventricular connections, normal biventricular function, patent foramen ovale with left-to-right flow, tiny posterior muscular ventricular septal defect with left-to-right shunting, and a flattened interventricular septum suggestive of at least mildly elevated right ventricular (RV) pressures.
Chemotherapy was initiated on day of life 2, according to the COG-AALL0631, a clinical trial to assess whether the FLT3 tyrosine kinase inhibitor to postinduction chemotherapy will enhance the effectiveness of chemotherapy. The patient received 1 dose of methotrexate and 7 days of methylprednisolone before transitioning to AML0531-armA with intrathecal cytarabine, intravenous cytarabine, daunomycin, and etoposide on day of life 10 due to lack of initial response. At 2 months of age, bone marrow aspirate demonstrated residual disease, and the patient was admitted for Induction II. Overall, a cumulative dose of 300mg/m2 of daunomycin was given.
An echocardiogram done prior to Intensification II, around 4 months of age, demonstrated severely decreased left ventricular (LV) systolic wall motion (shortening fraction 28%, LV ejection fraction 39%), increased LV size, and mild increase in pulmonary artery pressure. There was preserved RV wall motion and no evidence of thrombus. Chemotherapy was postponed and oral captopril initiated. Despite the addition of captopril, cardiac function continued to be poor, and digoxin, furosemide, and lovenox were initiated at 5 months of age, 2 days prior to the start of Intensification II. On day 12 after Intensification II with cytarabine and L-asparaginase, systemic hypoperfusion and congestive heart failure was apparent with increased serum lactate, elevated B-type natriuretic peptide of 2,394, decreased SvO2, emesis, and hypervolemia. He was transferred to the cardiac intensive care unit for milrinone initiation. During his stay in the cardiac intensive care unit, he had episodes of ventricular arrhythmia for which amiodarone was added. Poor cardiac function persisted despite high-dose milrinone, and, at 6 months of age, dobutamine was added.
Which of the following patients is at the highest risk for developing anthracycline-induced cardiotoxicity?
Show Answer