A 36-year-old woman with past medical history of pericarditis, asthma, pulmonary embolism, hypothyroidism and iron deficiency anemia due to menorrhagia presents to clinic for a follow up visit with complaints of recurrent chest pain on deep breathing. Chest pain is worse on lying down and improved when leaning forward. It is also associated with fever and mild shortness of breath. She was first diagnosed with pericarditis about 5 years ago and was initially treated with high dose ibuprofen and short prednisone bursts. She has been having more severe and frequent recurrences for the last 2 years and has been on a combination of ibuprofen, colchicine and methylprednisone. She has recurrence of chest pain each time her steroids are weaned. She required pericardiocentesis twice in the last 5 years. She gained 30 pounds since being started on steroids. Workup was negative for autoimmune disease, tuberculosis and familial Mediterranean fever.
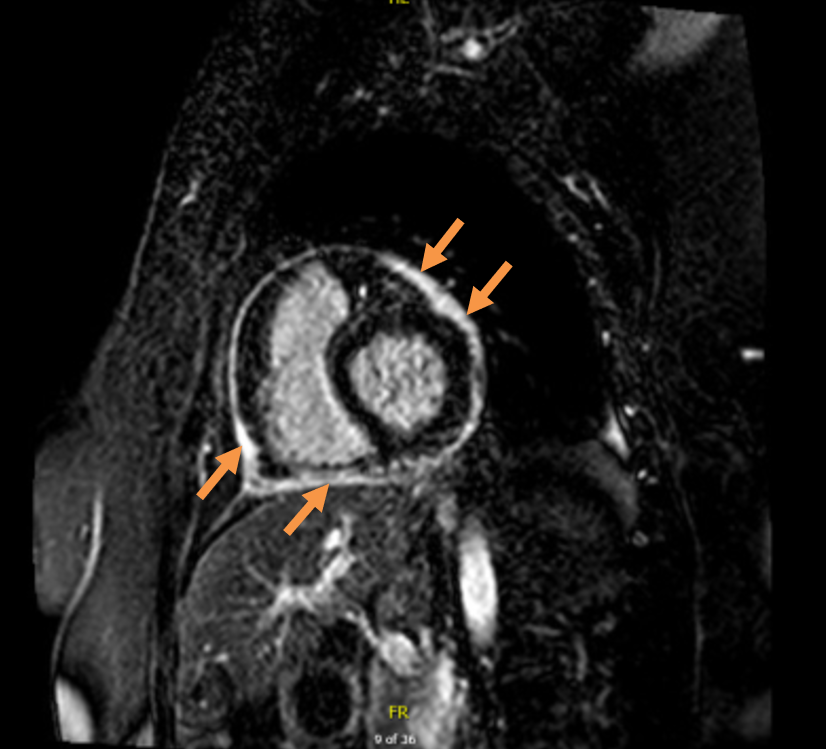
At her prior clinic visit, she was started on azathioprine for steroid sparing effect. She did well initially and was able to wean her methylprednisone to 20 mg daily. However, a week ago, she was diagnosed with right foot metatarsal fracture and a right hip fracture. Current medications include methylprednisone 20 mg daily, colchicine 0.6 mg BID, ibuprofen 200 mg BID, levothyroxine 75 mcg daily, cholecalciferol 1000 units daily, warfarin 5 mg daily and azathioprine 100mg daily. At this visit, she has a blood pressure of 150/78 mmHg, pulse of 92 beats per minute, respiratory rate of 14 per minute and BMI of 39.38 kg/m2. Physical exam revealed obesity, abdominal striae and few old bruises. Lungs were clear to auscultation, there was no jugular venous distention or pericardial rub but had trace pitting pedal edema. C-reactive protein is 29.5 mg/dL (Normal: <1 mg/dL), sedimentation rate is 47 mm/hr (Normal: 0-15 mm/hr). There are no ECG changes and an echocardiogram showed trivial pericardial effusion, normal left ventricular systolic and diastolic function, no significant valvular abnormalities, mild septal bounce, respiratory variation across the tricuspid valve of -63% and across mitral valve of 30%. IVC is dilated at 2.6 cm but collapses with inspiration. Cardiac MRI with gadolinium is shown in figure 1.
Figure 1: Cardiac MRI with gadolinium. Delayed enhancement image.
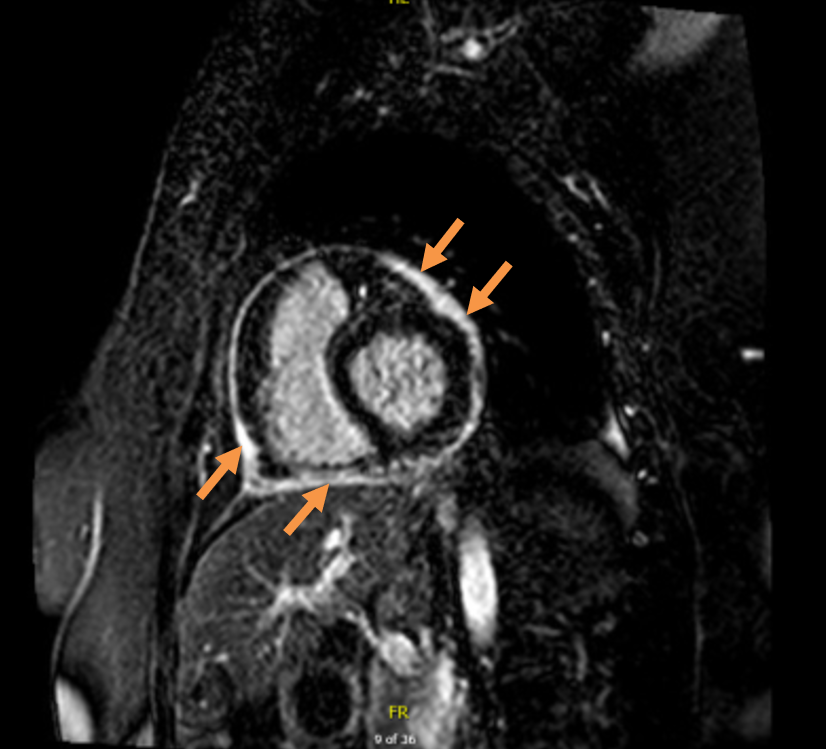 Pericardial delayed hyperenhancement (late gadolinium enhancement) on fat suppressed sequence with gadolinium.
Pericardial delayed hyperenhancement (late gadolinium enhancement) on fat suppressed sequence with gadolinium.
The correct answer is: C. Start anakinra.
This patient is having a flare up of idiopathic recurrent pericarditis (IRP). She has the typical pericarditic chest pain, trivial pericardial effusion, elevated inflammatory markers and moderate to severe pericardial delayed hyperenhancement on cardiac MRI along with some early features of constrictive physiology. Her MRI also showed mild pericardial thickening and circumferentially increased pericardial signal intensity on T2 STIR weighted imaging suggestive of pericardial edema. Given the intractable disease and significant complications of long-term steroid use, starting anakinra in the place of azathioprine is the best option for her at this time. Once the pericarditis is controlled and inflammatory markers have normalized, other medications starting with corticosteroids followed by nonsteroidal anti-inflammatory drugs (NSAIDs) can be weaned off successfully.
The 2015 European Society of Cardiology (ESC) pericardial disease guidelines define recurrent pericarditis as recurrence of pericarditis after a first episode of acute pericarditis (diagnosed by two out of four criteria of: 1) pericarditic chest pain; 2) pericardial rub; 3) new diffuse ST-elevation or PR depression on ECG; or 4) new or worsening pericardial effusion) and a symptom free interval of at least 4-6 weeks.1 About 15-30% of patients have recurrences after an initial episode and the rate is higher in patients treated with corticosteroids or those not treated with colchicine.1,2 Workup includes complete blood count, comprehensive metabolic profile, inflammatory markers such as C- reactive protein, sedimentation rate and an electrocardiogram. Echocardiogram is first line imaging test and a CT scan or more often a cardiac MRI with contrast may be obtained on a case by case basis.3
NSAIDs or aspirin and colchicine dual therapy with exercise restriction is the first line of treatment for recurrent pericarditis.1 Colchicine has been shown in three randomized clinical trials to reduce the rate of recurrence (relative risk 0.49, 95% CI 0.24-0.65; p = 0.0009, NNT:5) and is considered first-line therapy for recurrent pericarditis.4-8 Corticosteroids are second line therapy and are used at low to moderate doses as an add on therapy to NSAIDs and colchicine; also known as "triple therapy" unless one or more of them are contraindicated.9 Though corticosteroids act fast and are very effective at controlling the inflammation, chronicity and recurrences are common, especially with rapid tapers, and so are not recommended. Corticosteroids are best tapered over many weeks or months and some patients may have difficulty weaning off the corticosteroids especially at doses around 10mg daily.10 Further long-term use of corticosteroids may lead to many side effects such as immunosuppression causing infections, weight gain, osteoporosis, ulcers, adrenal insufficiency and mood changes. Currently, although there are no FDA approved medications specifically for recurrent pericarditis, few disease-modifying anti-rheumatic agents and biologics as described below have shown efficacy and have been safely used to treat patients with steroid dependent and colchicine resistant idiopathic recurrent pericarditis.
Azathioprine (Option B) is an oral anti-metabolite medication that was found to be effective in reducing risk of recurrence in steroid dependent recurrent pericarditis as reported in case reports and case series.10-12 In a retrospective study of 46 patients with idiopathic recurrent pericarditis, azathioprine allowed most patients to discontinue steroids, though at the end of the follow up period, 24% of patients still required azathioprine. It is a common choice for steroid dependent recurrent pericarditis patients or those with autoimmune recurrent pericarditis due to its oral dosing which allows weaning of corticosteroids. Infections, GI toxicity, elevated transaminases and hematologic toxicity may complicate therapy. White cell counts need to be monitored regularly with this medication. Azathioprine is slow acting, and in this patient, a dose increase is not the best option given that she had a recurrence while tapering the corticosteroid on the medication.
Other medications like methotrexate, hydroxychloroquine or etanercept (option E) may be used selectively in patients where the etiology of recurrent pericarditis is autoimmune such as systemic lupus erythematosus or rheumatoid arthritis requiring better control of the underlying disease process. Idiopathic recurrent pericarditis is, however, much more common than autoimmune etiology of recurrent pericarditis. Adalimumab is a tumor necrosis factor alpha antagonist (option D) that has not been studied for treatment of pericarditis and was even implicated as causing pericarditis and pericardial effusion.13,14 Intravenous immunoglobulin (IVIG) has been used in patients with idiopathic recurrent pericarditis as described in case reports and case series. It is rapid acting, given as an infusion over 5 days and has a long half-life of 35 days. IVIG is costly with the possibility of requiring repeat infusions and hospitalization, while infusion reactions are common and hypersensitivity reactions may occur.12
Anakinra (option C) is a recombinant human interleukin-1 receptor antagonist which is FDA approved for rheumatoid arthritis and cryopyrin-associated periodic syndromes (CAPS) such as neonatal onset multisystem inflammatory disease.15 It competitively blocks the pro-inflammatory cytokine, interleukin-1 beta and alpha by binding to the interleukin-1 type I receptor. For adults, it is given as a daily injection of 100mg by subcutaneous injection and is well tolerated by most patients. Common adverse events include mild injection site reactions, upper respiratory tract infection, headache, nausea and vomiting. Neutrophil counts should be checked before starting and monitored on a regular basis. As with any biologic drug, monitoring for serious infections is also indicated. Anakinra was first noted to be effective in treating recurrent pericarditis in the pediatric population and later in few case series. The AnakInRa for Treatment of Recurrent Idiopathic Pericarditis (AIRTRIP) study is the only randomized double-blind study for anakinra with an open-label medication withdrawal design in 21 patients with recurrent idiopathic pericarditis in which anakinra reduced the risk of recurrence over a median of 14 months compared to placebo.16 Anakinra also allowed for discontinuation of the corticosteroids and NSAID in all the study patients. A recent systematic review and meta-analysis also showed the efficacy of anakinra in allowing the discontinuation of steroids and reducing the risk of recurrence.17 The usual duration of treatment is 6-9 months followed by a slow taper over many months.11,18
Canakinumab is a monoclonal antibody against interleukin-1 beta, also approved for CAPS and may be an option for patients who are unable to take anakinra daily injections. More recently in a small pilot study, rilonacept, a soluble decoy receptor given once a week subcutaneously, which binds to interleukin-1 beta and alpha, thereby preventing them from binding to the normal receptor, has shown promise in idiopathic recurrent pericarditis.19
Pericardiectomy (option F) may be a final and effective option in patients with intractable recurrent pericarditis, but the data is limited for inflammatory pericarditis without constriction. A single center retrospective study of 184 patients showed that it was safe and those who underwent pericardiectomy for recurrent pericarditis had a lower recurrence rate as well as a lower need for anti-inflammatory medications.20 Advances in surgical technique such as radical pericardiectomy have been shown to be safe and beneficial.21 However, pericardiectomy during acute inflammation may not be the best option for obvious reasons and chronic or high doses of steroids may lead to delayed wound healing and increased risk of infection.
In conclusion, interleukin-1 antagonism or blockade with anakinra has been shown to be an effective and appropriate option for patients with steroid dependent and colchicine resistant recurrent pericarditis. Co-management with a rheumatologist especially in low volume centers, or referral to an experienced center is recommended when biologics are used. Further studies are needed to assess the optimal duration of treatment and long-term usage of anakinra.
References
- Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases: the Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC) endorsed by: the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2015;36:2921-64.
- Cremer PC, Kumar A, Kontzias A, et al. Complicated pericarditis: understanding risk factors and pathophysiology to inform imaging and treatment. J Am Coll Cardiol 2016;68:2311-28.
- Klein AL, Abbara S, Agler DA, et al. American Society of Echocardiography clinical recommendations for multimodality cardiovascular imaging of patients with pericardial disease: endorsed by the Society for Cardiovascular Magnetic Resonance and Society of Cardiovascular Computed Tomography. J Am Soc Echocardiogr 2013;26:965-1012.
- Imazio M, Bobbio M, Cecchi E, et al. Colchicine as first-choice therapy for recurrent pericarditis: results of the CORE (COlchicine for REcurrent pericarditis) trial. Arch Intern Med 2005;165:1987-91.
- Agarwal SK, Vallurupalli S, Uretsky BF, Hakeem A. Effectiveness of colchicine for the prevention of recurrent pericarditis and post-pericardiotomy syndrome: an updated meta-analysis of randomized clinical data. Eur Heart J Cardiovasc Pharmacother 2015;1:117-25.
- Imazio M, Belli R, Brucato A, et al. Efficacy and safety of colchicine for treatment of multiple recurrences of pericarditis (CORP-2): a multicentre, double-blind, placebo-controlled, randomised trial. Lancet 2014;383:2232-7.
- Imazio M, Brucato A, Belli R, et al. Colchicine for the prevention of pericarditis: what we know and what we do not know in 2014 - systematic review and meta-analysis. J Cardiovasc Med 2014;15:840-6.
- Imazio M, Brucato A, Cemin R, et al. Colchicine for recurrent pericarditis (CORP): a randomized trial. Ann Intern Med 2011;155:409-14.
- Imazio M, Brucato A, Cumetti D et al. Corticosteroids for recurrent pericarditis: high versus low doses: a nonrandomized observation. Circulation 2008;118:667-71.
- Imazio M, Battaglia A, Gaido L, Gaita F. Recurrent pericarditis. Rev Med Interne 2017;38:307-11.
- Xu B, Harb SC, Cremer PC. New insights into pericarditis: mechanisms of injury and therapeutic targets. Curr Cardiol Rep 2017;19:60.
- Schwier NC, Hale GM, Davies ML. Treatment of adults with idiopathic recurrent pericarditis: novel use of immunotherapy. Pharmacotherapy 2017;37:305-18.
- Kelly D, O'Connell O, Henry M. Adalimumab-induced lupus serositis. BMJ Case Rep 2015.
- Ozkan H, Cetinkaya AS, Yildiz T, Bozat T. A rare side effect due to TNF-Alpha blocking agent: acute pleuropericarditis with adalimumab. Case Rep Rheumatol 2013;2013:985914.
- Highlights of Prescribing Information: Kineret ® (anakinra). https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/103950s5136lbl.pdf. accessed Apr 25, 2019
- Brucato A, Imazio M, Gattorno M, et al. Effect of anakinra on recurrent pericarditis among patients with colchicine resistance and corticosteroid dependence: the AIRTRIP randomized clinical trial. JAMA 2016;316:1906-12.
- Furqan M, Abdullah R, Verma B, et al. Effect of anakinra on colchicine resistant and steroid dependent recurrent pericarditis: a systemic review and meta-analysis. J Am Coll Cardiol 2019;73.
- Buckley LF, Viscusi MM, Van Tassell BW, Abbate A. Interleukin-1 blockade for the treatment of pericarditis. Eur Heart J Cardiovasc Pharmacother 2018;4:46-53.
- Klein A, Lin D, Cremer P, et al. Rilonacept in recurrent pericarditis: first efficacy and safety data from an ongoing phase 2 pilot clinical trial. J Am Coll Cardiol 2019;73:1261.
- Khandaker MH, Schaff HV, Greason KL, et al. Pericardiectomy vs. medical management in patients with relapsing pericarditis. Mayo Clin Proc 2012;87:1062-70.
- Johnston DR. Surgical management of pericardial diseases. Prog Cardiovasc Dis 2017;59:407-16.