Rock Climbing Leads to. . .
A previously healthy 38-year-old male smoker presents to the emergency room with a 48-hour history of acute onset of right upper extremity swelling, erythema, and discomfort. On further questioning, he had gone rock climbing as he does on many nights, with symptom onset about 12 hours later. Due to symptoms persisting for an additional 36 hours with increasing right arm discomfort, he presented to the emergency department. He denies any prior history of blood clots or family history of clotting disorders. Physical examination is remarkable for right upper extremity non-pitting edema with overlying erythema from the shoulder to the wrist and mild distention of the superficial arm veins. His right radial pulse is normal with full range of motion of the right upper extremity. A duplex is performed which is notable for thrombosis of the right brachial, axillary, and subclavian veins.
What is the most appropriate management for this patient?
Show Answer
The correct answer is: D. Consult vascular specialists for catheter-based venography, catheter-based thrombolysis, and thoracic outlet decompression.
This patient has developed an axillary-subclavian vein thrombosis (ASVT) (Figure 1) and should undergo a venogram with catheter-directed thrombolytic therapy.
Figure 1
Figure 1
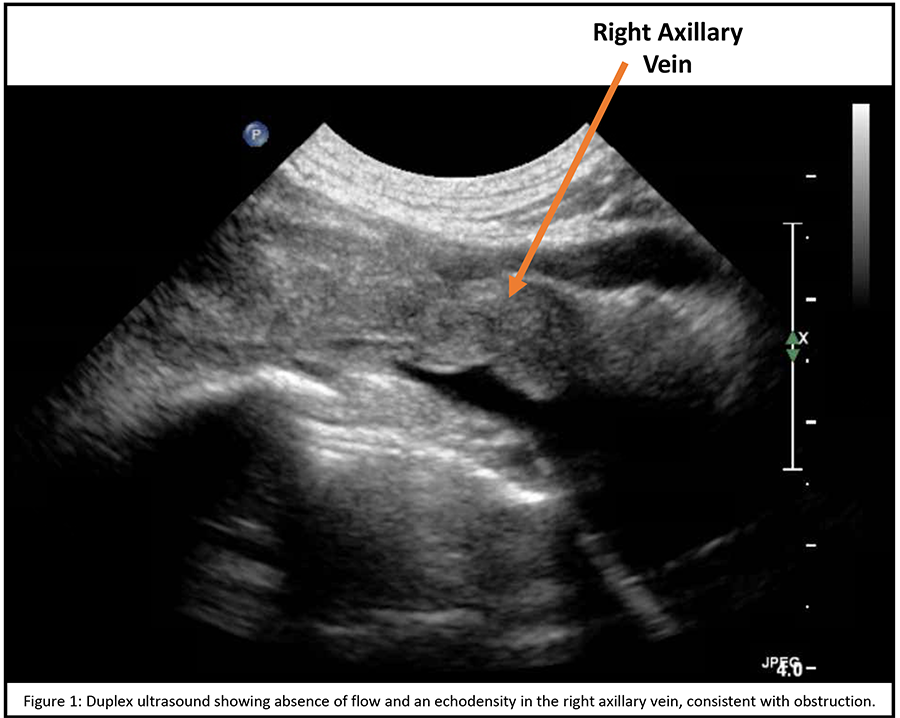
Also known as Effort Thrombosis or Paget-Schroetter Syndrome, ASVT is a rare entity that typically affects young, healthy individuals. Primarily affecting the subclavian vein at the costoclavicular junction, it preferentially involves the dominant arm.1-3
The pathophysiology is thought to be related to repetitive trauma of the upper extremity in the setting of an underlying anatomical abnormality at the thoracic outlet.3 As such, ASVT is thought to be a manifestation of venous thoracic outlet syndrome (VTOS), specifically related to a restricted anterior portion of the thoracic outlet region.2,3 Wrestling, basketball, gymnastics, and swimming have all been described as activities with repetitive upper extremity movements which can lead to ASVT,1,4 though non-athletes with frequent overhead activities such as painting and auto mechanics can also develop ASVT.3
In patients with VTOS, progressive fibrosis and focal stenosis can occur when the subclavian vein is repetitively compressed between the first rib, clavicle, anterior scalene muscle, subclavius muscle, and the costoclavicular ligament.2,3 Compression of the vein leads to stasis and restricted mobility of the subclavian vein, leading to a cycle of endothelial trauma, thrombosis and recanalization with subsequent intimal hyperplasia, inflammation, and fibrosis.1,2,5,6
Classically, individuals with ASVT present with sudden onset of arm discomfort and swelling, though they can also present with a constellation of symptoms known as Urschel's sign, which includes arm heaviness, erythema, and cyanosis of the affected upper extremity.3 If the occlusion is chronic, dilated visible superficial veins across the upper arm, chest wall, and shoulder may develop.3,7,8
Initial evaluation involves Doppler ultrasonography, but is limited by the position of the clavicle, depth of the vein, expanded collateral veins which may be mistaken for the subclavian vein, and is highly dependent on a skilled sonographer.3 Increasingly, computed tomography and magnetic resonance imaging venography are being utilized to identify and characterize ASVTs, although they should be protocoled appropriately to image the venous phase.5,9 Contrast venography is considered the gold standard, as it provides higher spatial and temporal resolution of collateral venous anatomy as well as the extent of thrombosis.1,5,9
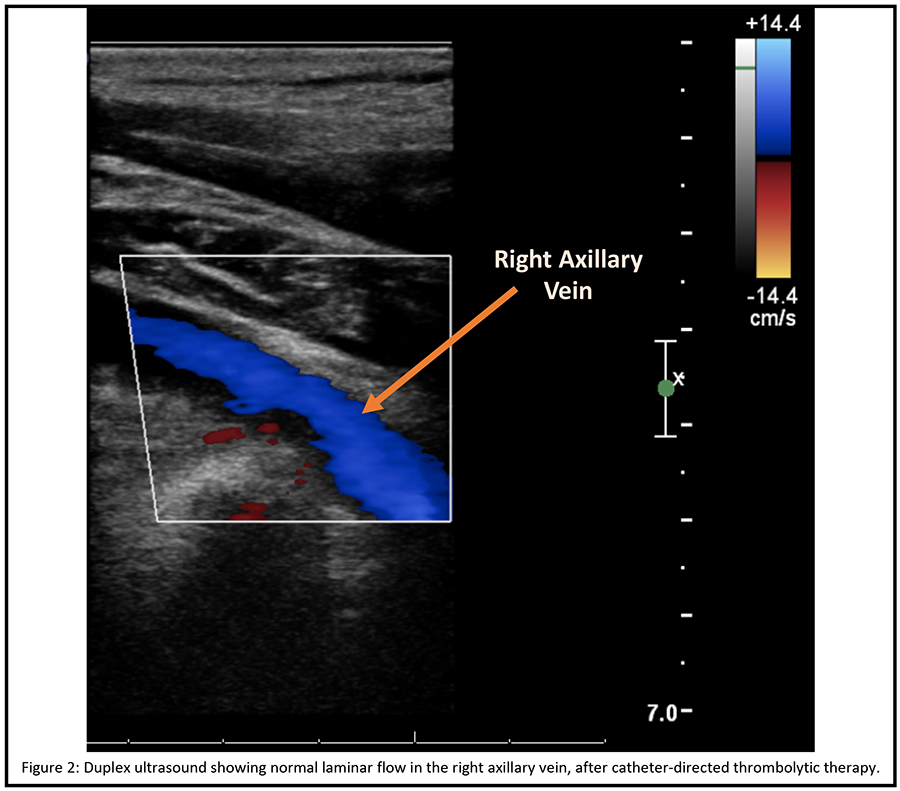
The management of ASVT has evolved over time, noting that leaving an ASVT untreated results in significant morbidity in most patients.3 Treatment with anticoagulation alone is also insufficient, leading to residual disability in the form of persistent symptoms due to chronic venous obstruction or even the development of acute pulmonary emboli,3,10-13 and is therefore not recommended.1,3,14 The mainstay of management is catheter-directed thrombolysis with subsequent thoracic outlet decompression.1 The earlier catheter-directed thrombolysis is performed, the more likely the procedure is to be successful, nearing 100% if initiated within a few days (and less than ten days) of symptom onset.3 Without subsequent thoracic outlet decompression, recurrent ASVT occurs in up to a third of patients,3,14 though there is significant controversy regarding the need for decompression. Decompression most commonly involves resection of the first rib with good long-term outcomes.14,15 A majority of experts agree that decompression is necessary to prevent recurrence and that early decompression has been shown to be effective and safe.3,14-17
Our patient with an ASVT had successful recanalization of his axillary and subclavian veins by catheter-directed thrombolytic therapy. Two weeks after his hospitalization, he underwent successful first right rib resection with anterior scalenectomy and venolysis. Five weeks after his presentation, he is doing well with complete resolution of his right upper extremity swelling and discomfort. A duplex at that time revealed laminar flow in the right axillary vein without evidence of thrombus (Figure 2). He has resumed more vigorous activities, but has not yet returned to rock climbing. Preventative contralateral evaluation and intervention was discussed, but not pursued due to lack of evidence.
Figure 2
Figure 2
References
- Alla VM, Natarajan N, Kaushik M, Warrier R, Nair CK. Paget-schroetter syndrome: review of pathogenesis and treatment of effort thrombosis. West J Emerg Med 2010;11:358-62.
- Vemuri C, Salehi P, Benarroch-Gampel J, McLaughlin LN, Thompson RW. Diagnosis and treatment of effort-induced thrombosis of the axillary subclavian vein due to venous thoracic outlet syndrome. J Vasc Surg Venous Lymphat Disord 2016;4:485-500.
- Illig KA, Doyle AJ. A comprehensive review of Paget-Schroetter syndrome. J Vasc Surg 2010;51:1538-47.
- Zell L, Kindermann W, Marschall F, Scheffler P, Gross J, Buchter A. Paget-Schroetter syndrome in sports activities:case study and literature review. Angiology 2001;52:337-42.
- Thompson RW. Comprehensive management of subclavian vein effort thrombosis. Semin Intervent Radiol 2012;29:44-51.
- Aziz S, Straehley CJ, Whelan TJ, Jr. Effort-related axillosubclavian vein thrombosis. A new theory of pathogenesis and a plea for direct surgical intervention. Am J Surg 1986;152:57-61.
- Horattas MC, Wright DJ, Fenton AH, et al. Changing concepts of deep venous thrombosis of the upper extremity--report of a series and review of the literature. Surgery 1988;104:561-67.
- Prandoni P, Bernardi E. Upper extremity deep vein thrombosis. Curr Opin Pulm Med 1999;5:222-26.
- Desjardins B, Rybicki FJ, Kim HS, et al. ACR Appropriateness Criteria® Suspected upper extremity deep vein thrombosis. J Am Coll Radiol 2012;9:613-19.
- Aburahma AF, Sadler DL, Robinson PA. Axillary subclavian vein thrombosis. Changing patterns of etiology, diagnostic, and therapeutic modalities. Am Surg 1991;57:101-07.
- Becker DM, Philbrick JT, Walker FB. Axillary and subclavian venous thrombosis: prognosis and treatment. Arch Intern Med 1991;151(10):1934-43.
- Heron E, Lozinguez O, Emmerich J, Laurian C, Fiessinger JN. Long-term sequelae of spontaneous axillary-subclavian venous thrombosis. Ann Intern Med 1999;131:510-13.
- Hingorani A, Ascher E, Lorenson E, et al. Upper extremity deep venous thrombosis and its impact on morbidity and mortality rates in a hospital-based population. J Vasc Surg 1997;26:853-60.
- Urschel HC, Jr., Razzuk MA. Paget-Schroetter syndrome: what is the best management? Ann Thorac Surg 2000;69:1663-68.
- Molina JE, Hunter DW, Dietz CA. Paget-Schroetter syndrome treated with thrombolytics and immediate surgery. J Vasc Surg 2007;45:328-34.
- Lee JT, Karwowski JK, Harris EJ, Haukoos JS, Olcott C 4th. Long-term thrombotic recurrence after nonoperative management of Paget-Schroetter syndrome. J Vasc Surg 2006;43:1236-43.
- Urschel HC, Jr., Patel AN. Surgery remains the most effective treatment for Paget-Schroetter syndrome: 50 years' experience. Ann Thorac Surg 2008;86:254-60.
