A 79-year-old male patient with a medical history of paroxysmal atrial fibrillation (AF), hypertension, and chronic kidney disease presents to the hospital after a mechanical fall resulting in a right intertrochanteric femur fracture. He undergoes right femur open reduction internal fixation surgery. After the successful operation, the patient experiences palpitations and is found to be in AF with rapid ventricular response. A transthoracic echocardiogram is performed while he is intermittently in AF.
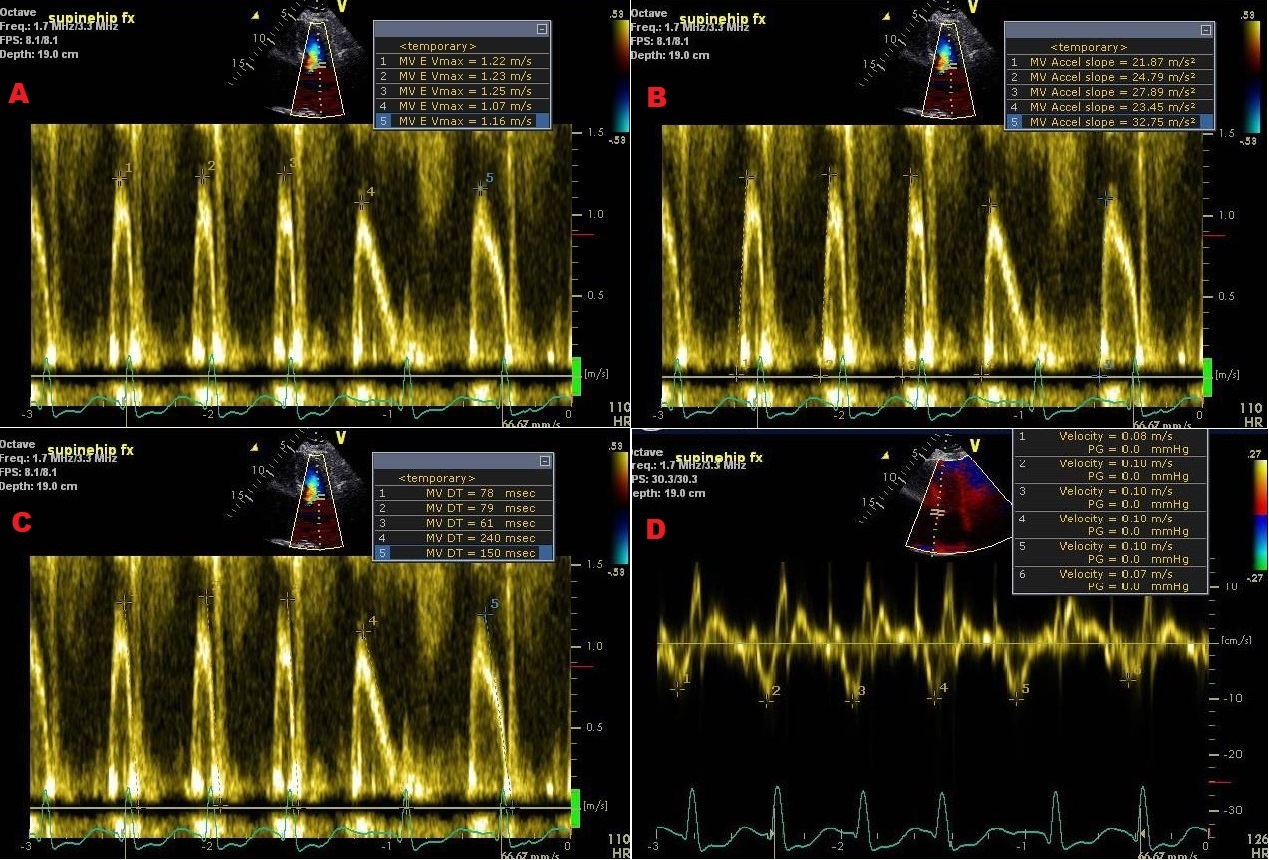
Figure 1: Atrial Fibrillation Rhythm
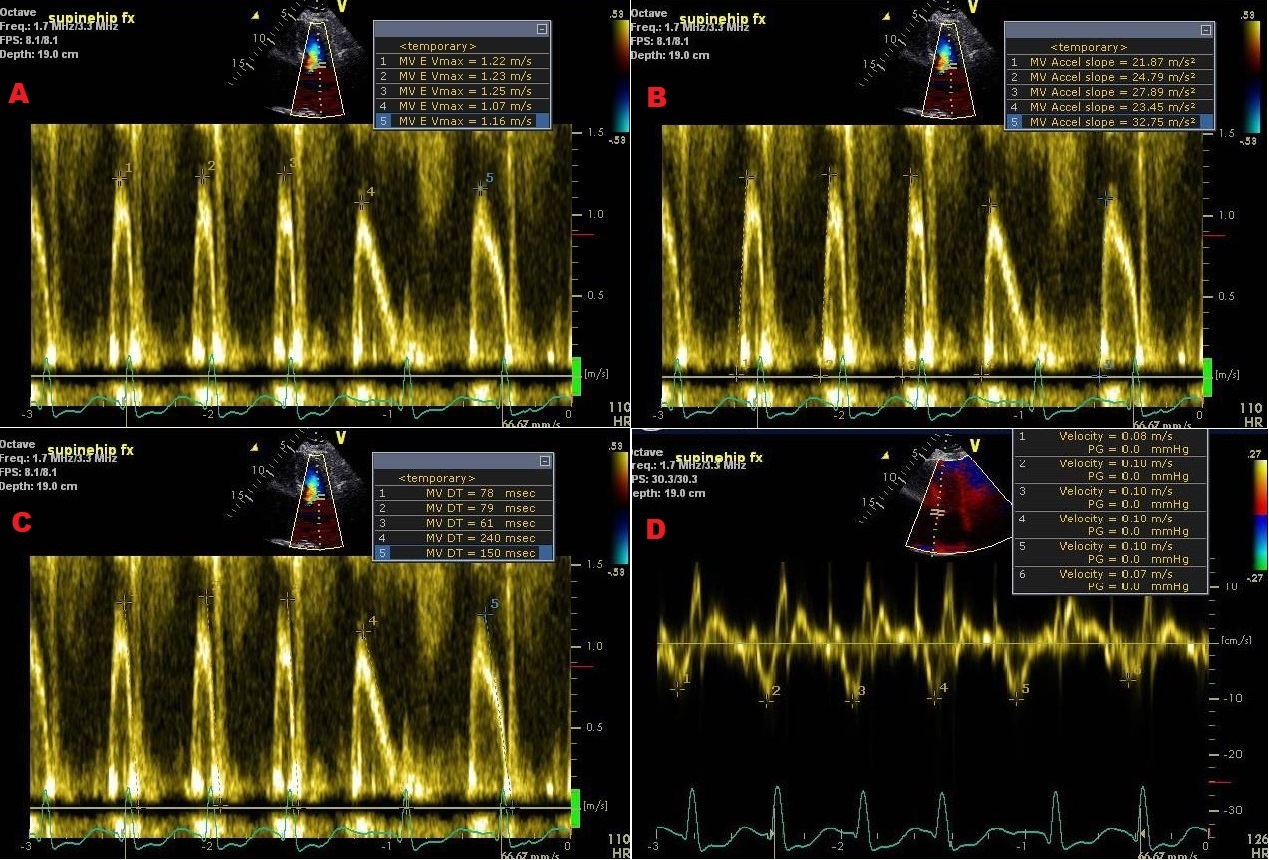 (A) Mitral E maximum velocity (1.19 m/s). (B) Mitral E velocity peak acceleration rate (2,615 cm/s2). (C) Mitral valve DT (122 msec). (D) Tissue Doppler septal e' velocity (9 cm/s).
(A) Mitral E maximum velocity (1.19 m/s). (B) Mitral E velocity peak acceleration rate (2,615 cm/s2). (C) Mitral valve DT (122 msec). (D) Tissue Doppler septal e' velocity (9 cm/s).
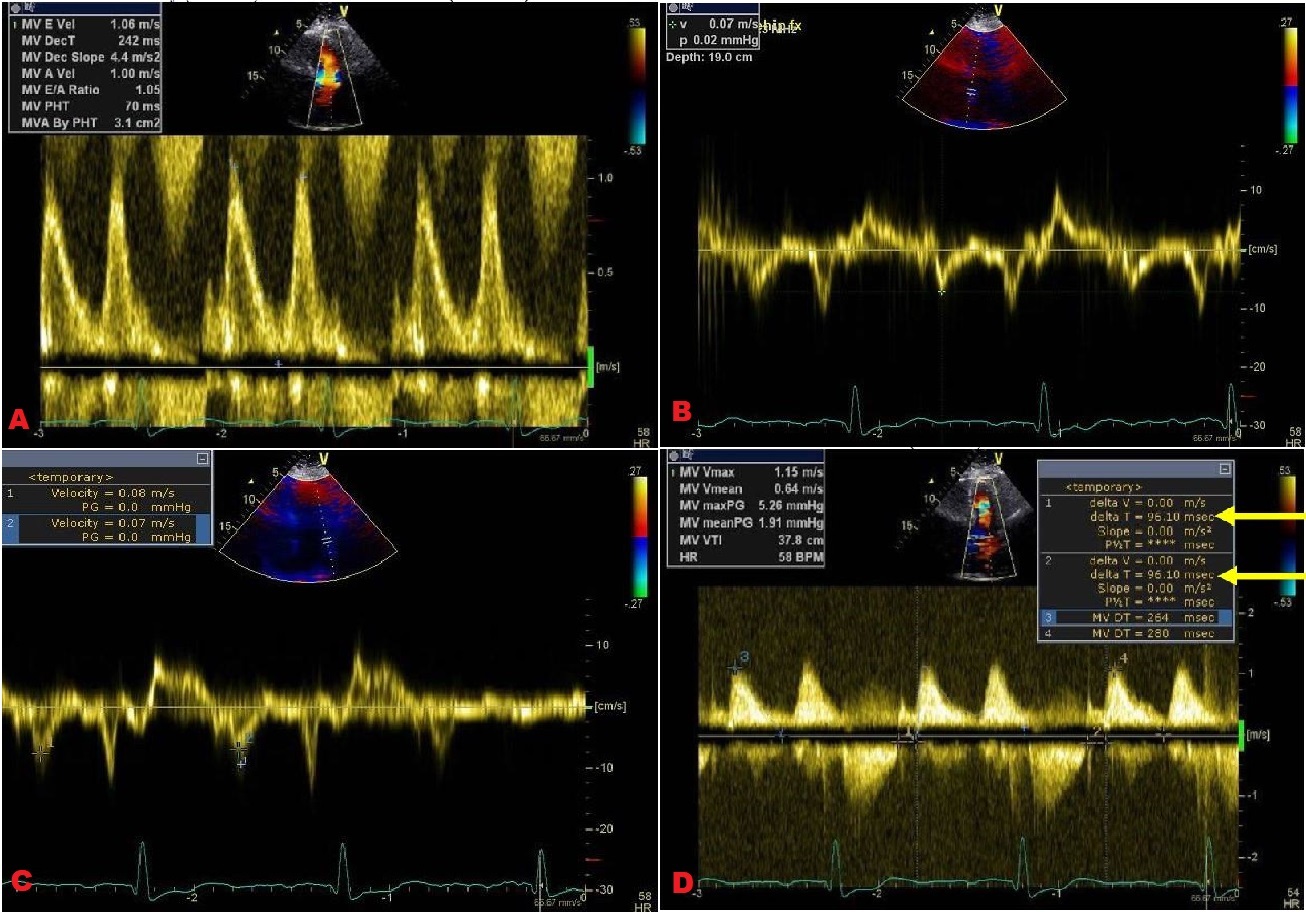
Figure 2: Sinus Bradycardia Rhythm
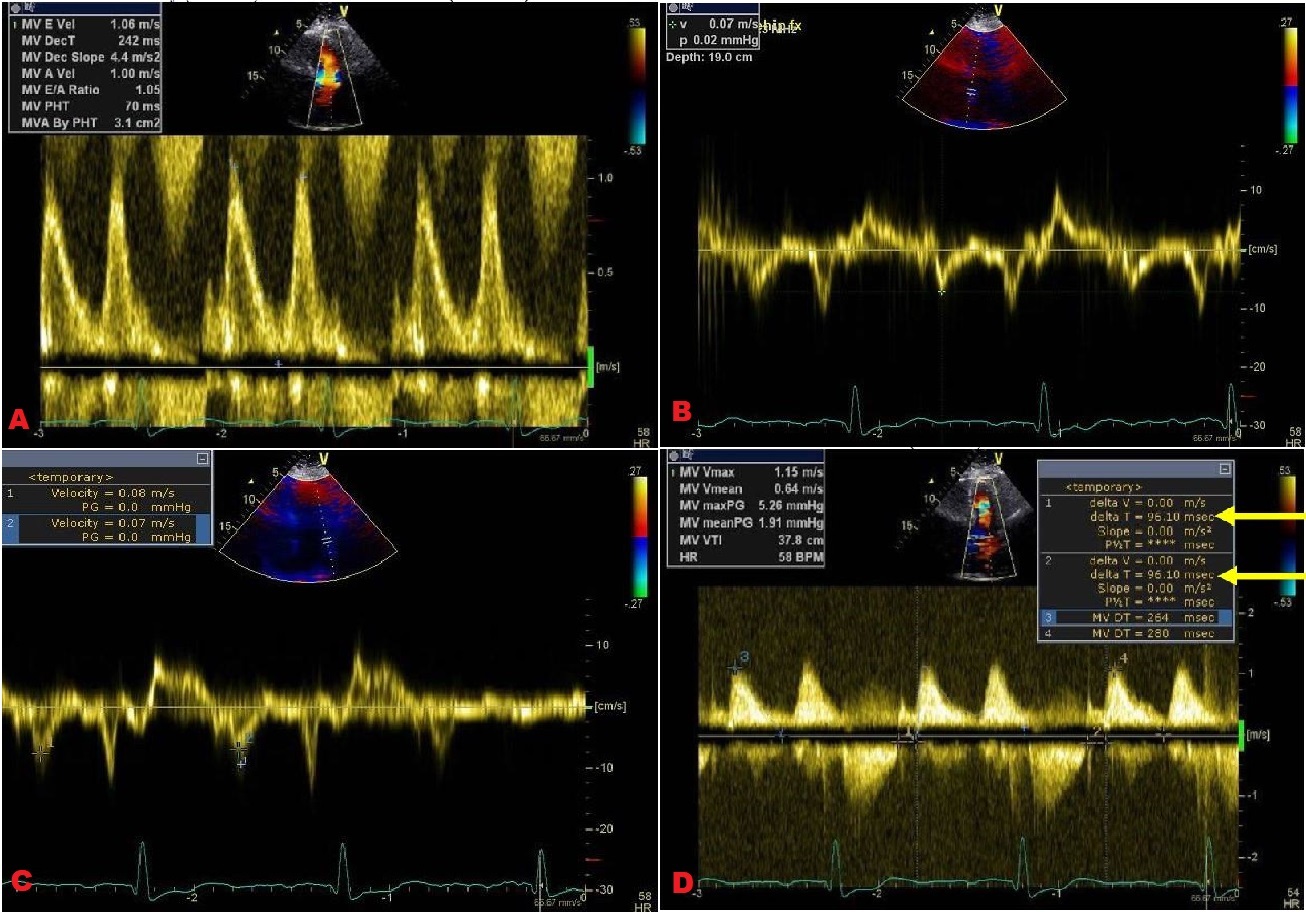 (A) Mitral E maximum velocity (1.06 m/s) and DT (242 msec). (B) Tissue Doppler septal e' velocity (7 cm/s). (C) Tissue Doppler lateral e' velocity (7.5 cm/s). (D) IVRT (96 msec).
(A) Mitral E maximum velocity (1.06 m/s) and DT (242 msec). (B) Tissue Doppler septal e' velocity (7 cm/s). (C) Tissue Doppler lateral e' velocity (7.5 cm/s). (D) IVRT (96 msec).
The correct answer is: B. Impaired LV relaxation, transiently elevated filling pressures
The 2016 diastolic function guidelines from the American Society of Echocardiography (ASE) and the European Association of Cardiovascular Imaging (EACVI)1 provide the following abnormal cut-off values of 5 parameters that can be used in the assessment of diastolic function in AF:
- Peak acceleration rate of mitral E velocity ≥1900 cm/sec2
- Isovolumic relaxation time (IVRT) of ≤65 msec
- Deceleration time (DT) of pulmonary venous diastolic velocity ≤220 msec
- E/Vp ratio of ≥1.4
- Septal E/e' ratio of ≥11
When obtaining measurements, multiple consecutive cardiac cycles should be averaged over 10 beats for more accurate interpretation, ideally with matched RR intervals for the E and e' velocities.1
In this patient, the peak acceleration rate is elevated, the septal e' velocity of 7 is borderline, the lateral e' velocity of 7.5 is reduced, and the septal E/e' ratio of 13 during AF (or average ratio of 15 in sinus rhythm) is elevated; all suggest probable diastolic dysfunction. One should note that although increased E/e' correlates with elevated left atrial (LA) pressures, values of approximately 8-14 fall under a "gray zone" of indeterminate significance regarding filling pressures. Therefore, other echocardiographic data should be investigated. For instance, the beat-to-beat variability noted in the mitral inflow peak E wave velocities suggests normal LV filling pressures because lower filling pressures (<15 mmHg) are associated with a higher coefficient of variation for this and other mitral inflow parameters.2 In addition, the normal LA size and the peak tricuspid regurgitation (TR) velocity of <2.8 point against chronically elevated LV filling pressures. The IVRT is mildly prolonged at 96 msec. The IVRT, normally <70 msec, prolongs in situations of impaired LV relaxation but normal filling pressures, ultimately shortening as LA pressure rises. Finally, the DT of 122 msec, averaged over 5 beats, is reduced. DT is a useful marker of LV end diastolic pressure in the setting of reduced ejection fraction and is less reliable in this case due to normal systolic function. However, one can observe that the fourth beat shown in AF occurs after a long RR interval and has a DT of 240 msec, like the DT obtained in sinus rhythm. This finding, in conjunction with the prolonged IVRT, suggests abnormal LV early relaxation. Finally, the elevated heart rate of 110 bpm while in AF should be noted. A lower heart rate would improve the utility of these mitral valve-related markers of diastolic dysfunction by allowing a longer LV filling time and revealing the true values for the various mitral inflow measurements.
Other parameters, such as E/Vp ratio and pulmonary vein diastolic velocity DT, were not provided and could have been helpful for diastolic assessment. LA global longitudinal strain values, which gradually decrease as diastolic dysfunction worsens, may also serve as a helpful tool for grading LV diastolic dysfunction in individuals with normal ejection fraction and in normal sinus rhythm.3 Despite lack of these values, the available information permits us to move beyond an assumption of "indeterminate diastolic function due to AF" and conclude that the patient likely has at least impaired relaxation, a finding that is not uncommon in this age group.
Because sinus rhythm was intermittently present during acquisition of Doppler images, the E/A ratio was acquired. This ratio can be used in conjunction with the 2016 guideline algorithm (see Figure 8 in the 2016 ASE/EACVI diastolic function guidelines1) to reach a conclusion regarding diastolic function.1 We start with Chart A given the patient's normal ejection fraction and lack of significant myocardial pathology, although one could consider starting with Chart B based on the degree of hypertensive heart disease present. Only points 1 and 2 (average E/e' >14 and lateral e' Doppler velocity <10 cm/s) are true, resulting in an indeterminate evaluation of LV diastolic function. Therefore, we move to Chart B for additional work-up. Given the sinus rhythm mitral inflow E/A ratio of 1.05, we are asked to evaluate the average E/e' ratio, TR velocity, and LA volume index. Only one criterion (average E/e' >14) is present, which suggests that the patient has grade 1 diastolic dysfunction with normal LA filling pressures.
There is a caveat to be considered here. Intermittent AF makes the use of conventional measures, such as LA size and TR velocity, that are problematic in assessing filling pressures. A patient with probable abnormal relaxation, as seen in this case, likely has at least transiently elevated filling pressures during periods of AF; the increased peak acceleration rate of the mitral E velocity during AF and borderline tissue Doppler e' velocity support this notion. Providers should be aware that filling pressures may vary in an individual depending on the clinical circumstance, such as AF, ischemia, or changes in heart rate and blood pressure. Therefore, we believe the best assessment of this patient's diastolic function is impaired relaxation with at least transiently elevated filling pressures during AF episodes.
Staging diastolic function becomes more challenging in the setting of AF. However, as this arrhythmia continues to be a common and growing occurrence, its presence during echocardiographic evaluation should not discourage the reader from attempting diastolic function assessment. Despite the loss of atrial mechanical function and the variability in cycle length, multiple parameters are available that can be utilized together to provide some measure of diastolic evaluation to guide clinical management.
References
- Nagueh SF, Smiseth OA, Appleton CP, et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 2016;29:277-314.
- Nagueh SF, Kopelen HA, Quiñones MA. Assessment of left ventricular filling pressures by Doppler in the presence of atrial fibrillation. Circulation 1996;94:2138-45.
- Singh A, Addetia K, Maffessanti F, Mor-Avi V, Lang RM. LA Strain for Categorization of LV Diastolic Dysfunction. JACC Cardiovasc Imaging 2017;10:735-43.