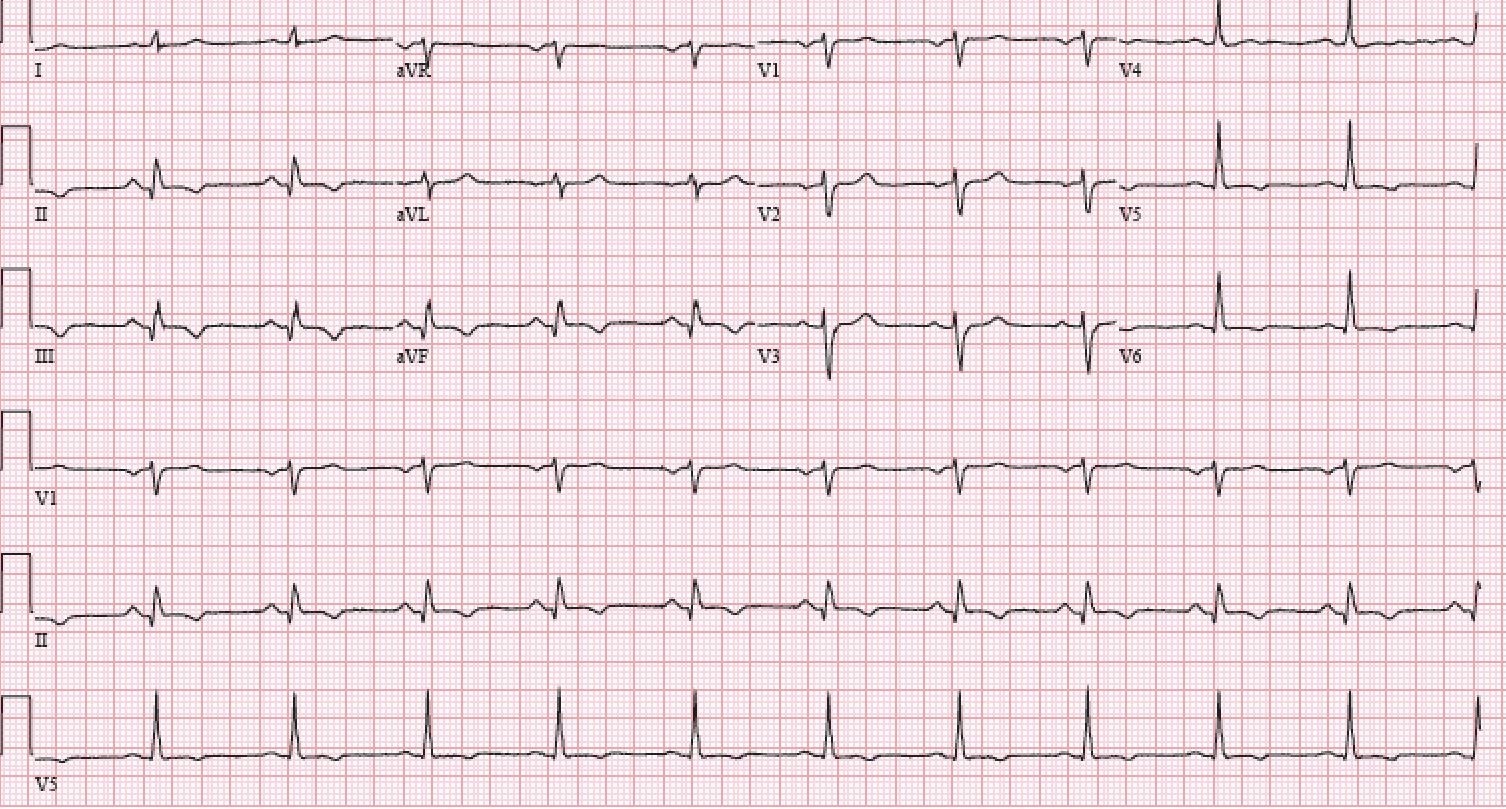
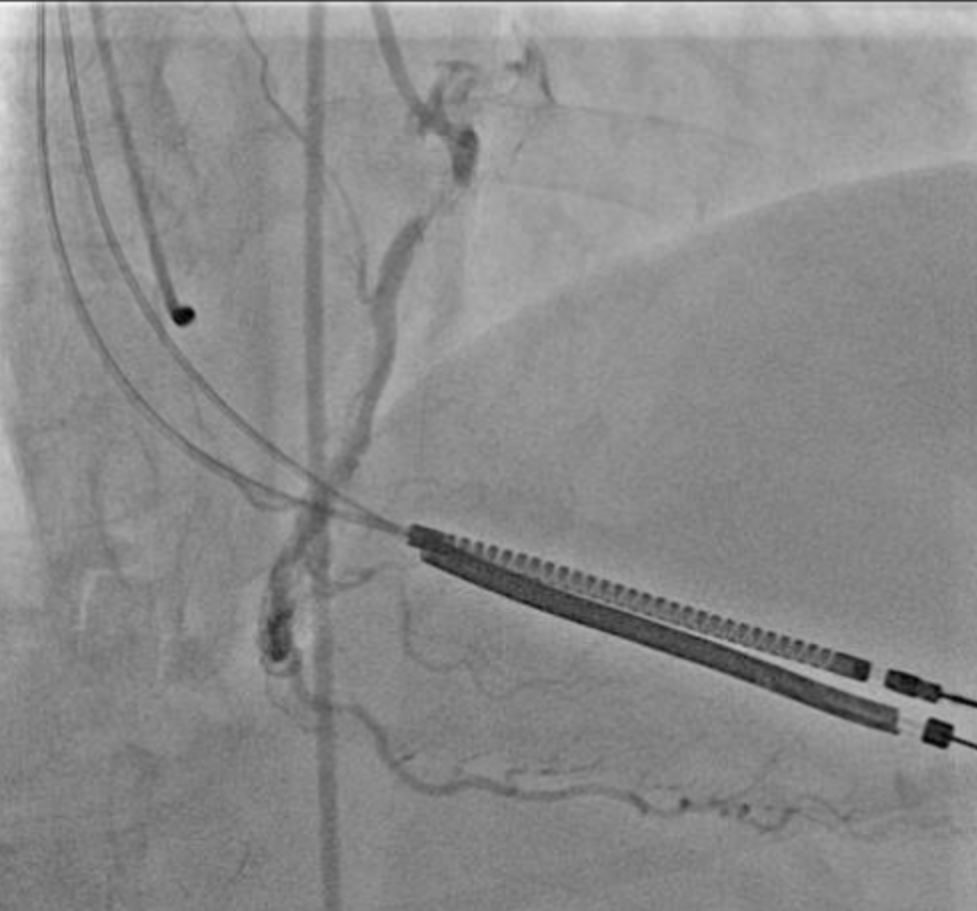
A 76-year-old female patient with hypertension, paroxysmal atrial fibrillation (AF) (AF burden of 58% on recent event monitor), and coronary artery disease with prior percutaneous coronary intervention (PCI) to the right coronary artery presented with symptoms of exertional chest pressure and dyspnea for the past 5 days. Her home medications included aspirin 81 mg/d, lisinopril 10 mg/d, warfarin 3.5 mg/d, and atorvastatin 80 mg/d. Her examination noted a regular rhythm with heart rate of 94 bpm and blood pressure of 135/78 mmHg. Her lung fields were clear to auscultation, and there was no gallop. An electrocardiogram showed normal sinus rhythm with Q waves and T wave inversions in inferior leads (Figure 1). Initial cardiac troponin I was 1.8 ng/ml (reference range <0.057 ng/ml). Coronary angiography revealed 95% stenosis in a previously stented segment of the right coronary artery (Figure 2). PCI was performed with placement of a 3.0 mm second-generation everolimus-eluting stent.
Figure 1
Figure 2
The correct answer is: C. Change warfarin to apixaban, add clopidogrel, and stop aspirin
In this case, we see an elderly woman with concomitant AF and coronary artery disease undergoing PCI in the setting of a non-ST-segment elevation myocardial infarction (MI). Oral anticoagulation is clearly indicated for stroke prophylaxis due to a CHA2DS2-VASc score of 5. Dual antiplatelet therapy (DAPT) also has a well-established role in the prevention of ischemic cardiovascular events following PCI. However, the use of triple therapy (i.e., a combination of warfarin with DAPT) has been shown to increase the risk of major bleeding without additional protection against ischemic events in the modestly sized WOEST (What is the Optimal Antiplatelet and Anticoagulant Therapy in Patients With Oral Anticoagulation and Coronary Stenting) trial.1
Dual therapy with direct acting oral anticoagulants (DOAC) and a P2Y12 inhibitor was compared with triple therapy with aspirin, P2Y12 inhibitor and vitamin K antagonists (VKA) in the REDUAL-PCI (Randomized Evaluation of Dual Antithrombotic Therapy With Dabigatran vs. Triple Therapy With Warfarin in Patients With Nonvalvular Atrial Fibrillation Undergoing Percutaneous Coronary Intervention) and PIONEER-AF (An Open-Label, Randomized, Controlled, Multicenter Study Exploring Two Treatment Strategies of Rivaroxaban and a Dose-Adjusted Oral Vitamin K Antagonist Treatment Strategy in Subjects With Atrial Fibrillation Who Undergo Percutaneous Coronary Intervention) trials.2,3 Both trials demonstrated a significant reduction in major bleeding events with dual therapy (DOAC + P2Y12 inhibitor) compared with triple therapy. In each trial, no significant increase in ischemic events was observed. However, it was unclear if the reduced bleeding risk was derived from use of DOAC or from the omission of aspirin. Furthermore, both studies were underpowered for important secondary endpoints such as stent thrombosis.
The AUGUSTUS trial was a two-by-two factorial randomized clinical trial of patients with AF undergoing PCI.4 A total of 4,614 patients was randomized to either apixaban or VKA in an open-label fashion and either aspirin or placebo. Mean CHA2DS2-VASc score was 3.9. There was a significant reduction in major bleeding in patients receiving apixaban compared with VKA (10.5% vs. 14.7%; hazard ratio 0.69; 95% confidence interval [CI], 0.58-0.81). Bleeding events were significantly higher in patients receiving aspirin compared with placebo (16.1% vs. 9.0%; hazard ratio 1.89; 95% CI, 1.59-2.24). There were no differences in the rates of ischemic events between apixaban- and VKA-treated patients, but there was a trend toward higher rates of MI, stent thrombosis, and urgent revascularization in the placebo versus aspirin comparison. In a recently published risk-benefit analysis of the AUGUSTUS trial, Alexander et al. reported consistently similar or lower rates of bleeding and ischemic events among patients receiving apixaban in the first 30 days and from 30 days to 6 months after randomization.5 In the first 30 days from PCI, the use of aspirin resulted in an increase in bleeding (absolute risk difference 0.97% [95% CI, 0.23-1.70]) and a reduction in ischemic events (absolute risk difference -0.91% [95% CI, -1.74 to -0.08]). The magnitude of these effects was similar, suggesting an overall neutral effect. From 30 days to 6 months, the risk of ischemic events was similar (absolute risk difference -0.17% [95% CI, -1.33 to 0.98]), but bleeding events were more frequent in the aspirin group (absolute risk difference 1.25% [95% CI, 0.23-2.27]), suggesting net harm.
A meta-analysis of three randomized controlled trials involving patients with AF with acute coronary syndrome or undergoing PCI demonstrated significant reduction in major bleeding with dual therapy with DOAC + P2Y12 inhibitor compared with triple therapy.6 However, omission of aspirin was shown to be associated with higher rates of MI (3.8% vs. 3.0%; odds ratio 1.29; 95% CI, 1.02-1.63) and stent thrombosis (1.2% vs. 0.7%; odds ratio 1.61; 95% CI, 1.02-2.53). Given the low incidence of ischemic events following contemporary PCI, each individual trial was underpowered to detect subtle differences, which highlights the importance of pooled data.
Based on the above trials, updated guidelines give a Class IIa recommendation to the combination of anticoagulation, either a DOAC or warfarin, with a P2Y12 alone (preferably clopidogrel) without aspirin to reduce bleeding risk in patients with AF undergoing PCI.
In our patient, the best regimen seems to be dual therapy with a DOAC such as apixaban and a P2Y12 inhibitor to reduce risk of major bleeding while providing adequate stroke prophylaxis from AF. The risk-benefit analysis of the AGUSTUS trial and the meta-analysis by Luo et al. suggest a possible role for aspirin, especially in the first month after PCI. However, an appropriately powered randomized trial to confirm this finding is needed. Considering the currently available data, individual patient characteristics can be used to tailor antiplatelet therapy in the first 30 days after PCI. Patients with low bleeding risk and high ischemic risk, such as those presenting with acute coronary syndromes or undergoing complex interventions, may benefit from triple therapy consisting of a DOAC, aspirin, and a P2Y12 inhibitor for the first 30 days.
References
- Dewilde WJ, Oirbans T, Verheugt FW, et al. Use of Clopidogrel With or Without Aspirin in Patients Taking Oral Anticoagulant Therapy and Undergoing Percutaneous Coronary Intervention: An Open-Label, Randomised, Controlled Trial. Lancet 2013;381:1107-15.
- Cannon CP, Bhatt DL, Oldgren J, et al. Dual Antithrombotic Therapy With Dabigatran After PCI in Atrial Fibrillation. N Engl J Med 2017;377:1513-24.
- Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban Versus Warfarin in Nonvalvular Atrial Fibrillation. N Engl J Med 2011;365:883-91.
- Lopes RD, Heizer G, Aronson R, et al. Antithrombotic Therapy After Acute Coronary Syndrome or PCI in Atrial Fibrillation. N Engl J Med 2019;380:1509-24.
- Alexander JH, Wojdyla D, Vora AN, et al. Risk/Benefit Tradeoff of Antithrombotic Therapy in Patients With Atrial Fibrillation Early and Late After an Acute Coronary Syndrome or Percutaneous Coronary Intervention: Insights From AUGUSTUS. Circulation 2020;141:1618-27
- Luo CF, Mo P, Li GQ, Liu SM. Aspirin-omitted Dual Antithrombotic Therapy in Nonvalvular Atrial Fibrillation Patients Presenting With Acute Coronary Syndrome or Undergoing Percutaneous Coronary Intervention: Results of a Meta-Analysis. Eur Heart J Cardiovasc Pharmacother 2020;Mar 4:[Epub ahead of print].