A 53-year-old female is seen at our clinic as follow up for recurrent idiopathic pericarditis. Patient initial presentation was almost 6 years ago when she presented with left sided chest pain, pleuritic in nature, worsened with movement and deep breaths, radiating towards left shoulder which limited her daily activities to the extent that she was bedridden. She had no associated shortness of breath, orthopnea, weight gain, leg swelling or syncope. She had multiple recurrences requiring emergency room visits. Her medical history includes Factor V Leiden mutation and hypothyroidism. Her brother was diagnosed with pericarditis at age 27. Her physician told her that "some of your markers are suggestive of lupus". Chest computerized tomography (CT) scan performed at time of initial presentation showed moderate pericardial effusion. Erythrocyte sedimentation rate (ESR) was 44 mm/hr, ultrasensitive C-reactive protein (usCRP) was 170 mg/L. She was started on ibuprofen, colchicine and prednisone.
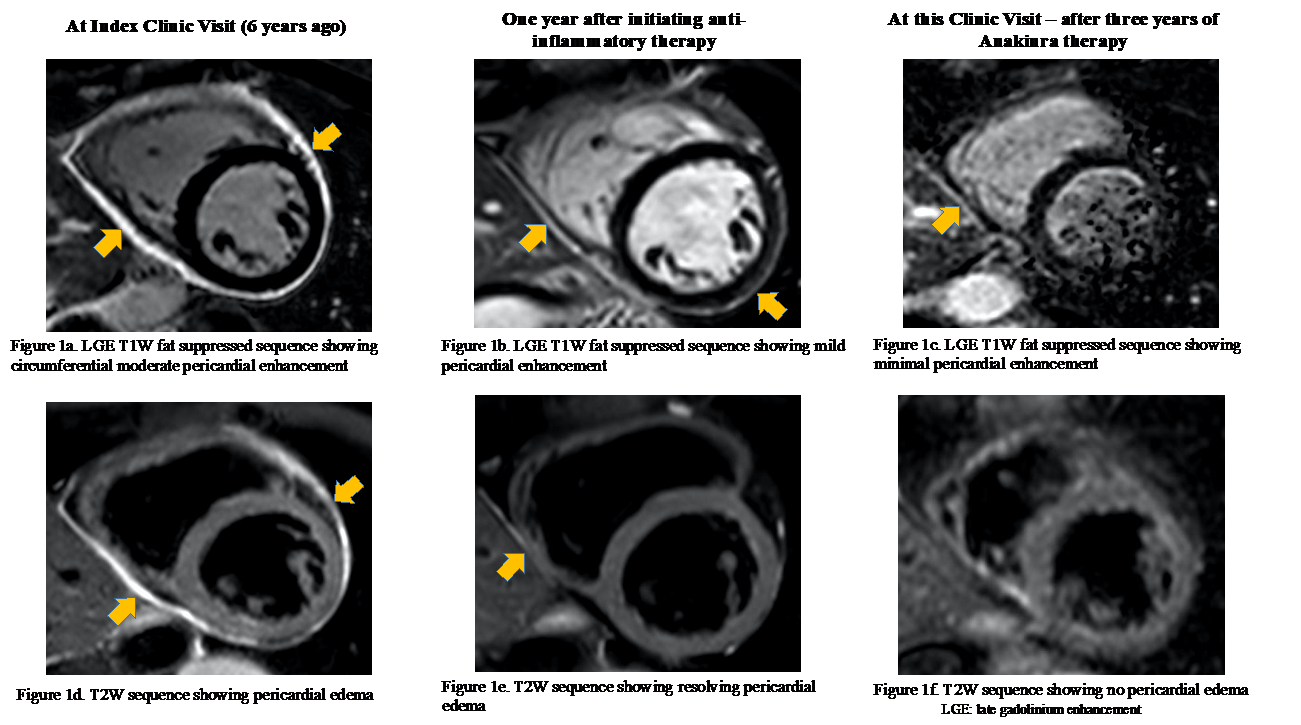
She was referred to our clinic and her initial work up showed ESR of 27mm/hr (normal 0-15 mm/hr), usCRP 31 mg/L (normal <3mg/L), NT pro BNP of 400 pg/mL and antinuclear antibody titer of 1:320 (normal ≤1:40). Electrocardiogram showed non-specific ST-T wave abnormalities. Viral testing for Coxsackie and echovirus was negative. Cardiac magnetic resonance imaging (CMR) showed moderate enhancement of the pericardium on late gadolinium enhancement T1 sequence, increased signal on T2 edema weighted imaging consistent with active pericarditis without any features of constriction (Figure 1a and 1d, respectively). We continued her triple therapy with colchicine, ibuprofen and prednisone.
During subsequent years, she developed multiple recurrences with pleuritic chest pains and elevated inflammatory markers. Follow-up CMR a year later showed mild circumferential delayed enhancement of pericardium and edema of pericardial layer (Figure 1b and 1e respectively). Prednisone dose was adjusted to attain better symptomatic control. Over subsequent months, attempt was made to taper her from steroids to avoid side effects She failed trial of azathioprine and was eventually started on anakinra after which prednisone and colchicine was gradually tapered off.
During this current office visit, she describes no chest pain. Her blood pressure was 90/62 mmHg, pulse 60 beats per minute, oxygen saturation 98% on room air. On examination, her lungs sounds were clear, S1 and S2 regular with no murmurs or pericardial knock. No jugular venous distention, Kussmaul's sign, and no peripheral edema was noticed. Her ESR was 2 mm/hr and usCRP was 1.1 mg/L. Her CMR showed only minimal pericardial enhancement, no pericardial edema or thickening or constriction (fFgure 1c & 1f, respectively). Since she had no further recurrences, her anti-inflammatory therapy, including anakinra, was gradually tapered off. Clinical recovery was evident as she can now tolerate her routine activities, walk 10,000 steps per week and perform pilates 2-3 times a week.
Figure 1a-1f
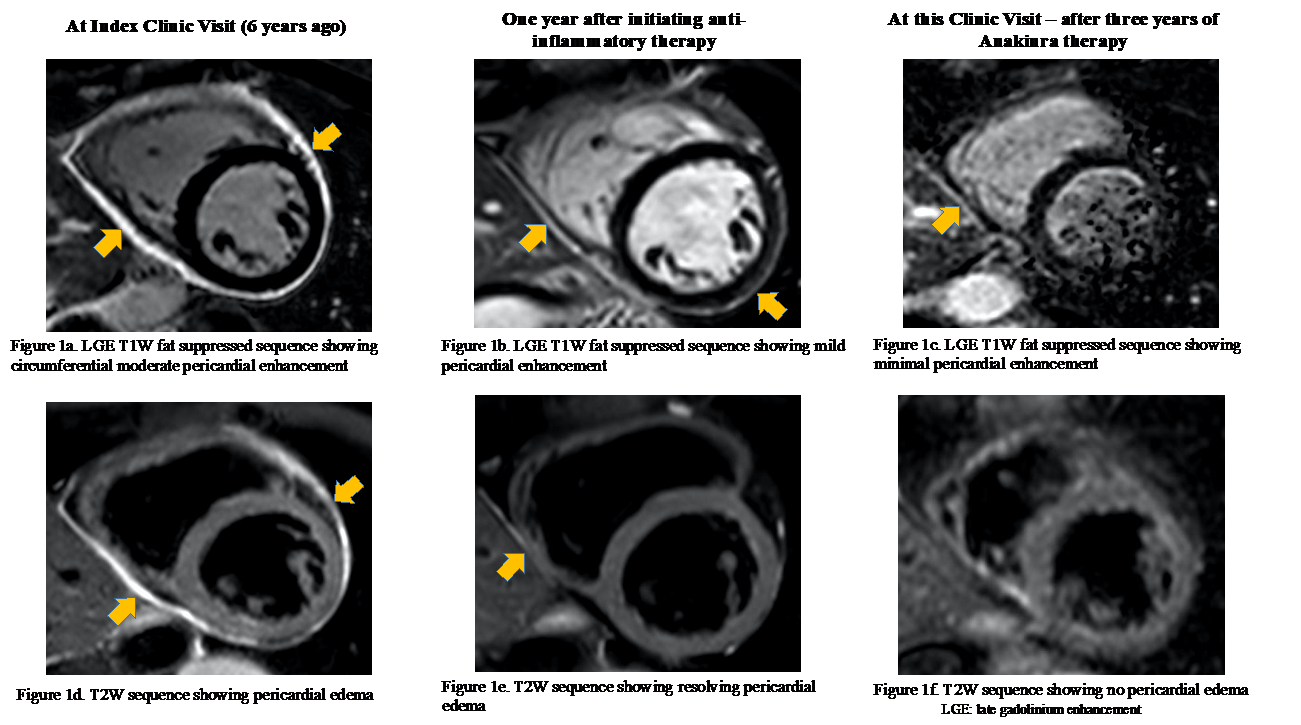 Figure 1a-1f: Late gadolinium enhancement T1 weighted imaging showing pericardial enhancement and T2 weighted imaging revealing pericardial edema during the clinical course. W: weighted
Figure 1a-1f: Late gadolinium enhancement T1 weighted imaging showing pericardial enhancement and T2 weighted imaging revealing pericardial edema during the clinical course. W: weighted
The correct answer is: D. All of the above
Recurrent pericarditis is a debilitating disease associated with increased morbidity and decreased quality of life.1 Underling etiology is predominantly idiopathic in majority of the cases and autoimmune in few. Its treatment is targeted towards reducing pericardial inflammation with non-steroidal anti-inflammatory agents and colchicine as the first line, steroids as the second line agent while azathioprine or biologics such as anakinra as third line agents.2 Patients who develop corticosteroid-dependence or colchicine resistant are at increased risk of side effects and benefit from anakinra.3
Our patient was initially started on second line anti-inflammatory therapy. She developed corticosteroid dependence, failed a trial of azathioprine and was then transitioned to anakinra (interleukin 1 antagonist). CMR performed at index clinic visit showed moderate enhancement of the pericardium on late gadolinium enhancement (LGE) T1 weight fat suppressed sequence. Subsequent CMRs revealed improvement in LGE to near resolution and ruled out the development of constrictive physiology. This information may not be accurately derived from the clinical features or inflammatory markers.
CMR is an important clinical decision-making tool in the management of pericarditis. T1 weighted sequences imaging of the pericardium in the delayed phase after administration of gadolinium as LGE can quantify inflammation as a volumetric parameter which can predict future recurrences and remissions.4,5 T2 weighted sequences can reveal presence of edema in the pericardial layer and is useful when contrast administration is not feasible.6 Information about tissue characterization obtained from CMR is unique as it can be used to guide therapy.5,6 It is technically not feasible to obtain from transthoracic echocardiography and cardiac CT. CMR can also identify hemodynamics changes such as development of constrictive physiology especially in transient constriction patients,7-9 which is a limiting feature of cardiac CT.10-12 In hemodynamically unstable scenarios, pregnancy, renal failure or in presence of cardiac devices, CMR use is contraindicated.6
Due to the prolonged inflammatory state of the pericardium in these patients, medical management with biologics requires close monitoring. Decision to adjust therapy such as steroids or anakinra is usually based on clinical symptoms and inflammatory markers.2 In our case beyond patient's clinical features and inflammatory markers, CMR provided incremental value such as tissue characterization, hemodynamics and response to therapy which we found useful in adjusting medications. It also depicted a potential role of CMR in predicting duration of treatment based on the extent of inflammation present at the index visit. Future studies are needed to better understand the benefit of performing serial CMRs in these patients and discover the utility of this novel approach.
References
- Cremer PC, Kumar A, Kontzias A, et al. Complicated pericarditis: understanding risk factors and pathophysiology to inform imaging and treatment. J Am Coll Cardiol 2016;68:2311–28.
- Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases. Eur Heart J 2015;36:2921–64.
- Imazio M, Andreis A, De Ferrari GM, et al. Anakinra for corticosteroid-dependent and colchicine-resistant pericarditis: The IRAP (International Registry of Anakinra for Pericarditis) study. Eur J Prev Cardiol 2020;27:956-64.
- Chetrit M, Xu B, Verma BR, Klein AL. Multimodality imaging for the assessment of pericardial diseases. Curr Cardiol Rep 2019;21:41.
- Kumar A, Sato K, Verma BR, et al. Quantitative assessment of pericardial delayed hyperenhancement helps identify patients with ongoing recurrences of pericarditis. Open Heart 2018;5:e000944.
- Chetrit M, Xu B, Kwon DH, et al. Imaging-guided therapies for pericardial diseases. JACC Cardiovasc Imaging 2020;13:1422–37.
- Zurick AO, Bolen MA, Kwon DH, et al. Pericardial delayed hyperenhancement with CMR imaging in patients with constrictive pericarditis undergoing surgical pericardiectomy: a case series with histopathological correlation. JACC Cardiovasc Imaging 2011;4:1180–91.
- Alraies MC, AlJaroudi W, Yarmohammadi H, et al. Usefulness of cardiac magnetic resonance-guided management in patients with recurrent pericarditis. Am J Cardiol 2015;115:542–7.
- Cremer PC, Tariq MU, Karwa A, et al. Quantitative assessment of pericardial delayed hyperenhancement predicts clinical improvement in patients with constrictive pericarditis treated with anti-inflammatory therapy. Circ Cardiovasc Imaging 2015;8:1–7.
- Bogaert J, Francone M. Pericardial disease: value of CT and MR imaging. Radiology 2013;267:340–56.
- Bogaert J, Francone M. Cardiovascular magnetic resonance in pericardial diseases. J Cardiovasc Magn Reson 2009;11:1–14.
- Taylor AM, Dymarkowski S, Verbeken EK, Bogaert J. Detection of pericardial inflammation with late-enhancement cardiac magnetic resonance imaging: initial results. Eur Radiol 2006;16:569–74.