A 45-year-old otherwise healthy male presents to clinic for further management of recurrent pericarditis. Initial episode occurred 3.5 years ago when he presented with vague chest pressure that worsened with deep inspiration and supine positioning. Labs were notable for elevated white blood cell (WBC) 16.6K/mm3 with 81% neutrophils, C-reactive protein (CRP) 11.2 mg/dL (normal <0.9 mg/dL), and erythrocyte sedimentation rate (ESR) 39 mm/hr (normal <15 mm/hr). Troponin I, NT pro-BNP, and electrocardiogram were within normal limits. Computed tomography (CT) angiography of the chest was negative for pulmonary embolism. Transthoracic echocardiogram (TTE) showed normal ejection fraction and trivial pericardial effusion. Treadmill stress testing showed no ischemia. He was discharged on naproxen 500 mg as needed for presumed idiopathic pericarditis.
One month later, he was readmitted for 12 hours of worsening chest pain with dyspnea and found to have large circumferential pericardial effusion without tamponade. Repeat labs showed elevated WBC 13.8K/mm3, CRP 13.3 mg/dL, and ESR 90 mm/hr, with normal troponin I and negative rheumatologic workup, including antinuclear antibody (ANA), rheumatoid factor, anti-CCP, anti-Ro, and anti-La antibodies. Subxiphoid pericardial window was performed by cardiothoracic surgery with 500ml blood-tinged fluid, noting very thickened pericardium with epicardial inflammation. Surgical pathology reported benign fibromuscular and adipose tissue with mild perivascular chronic inflammation. He was started on colchicine 0.6 mg daily and naproxen 500 mg twice a day.
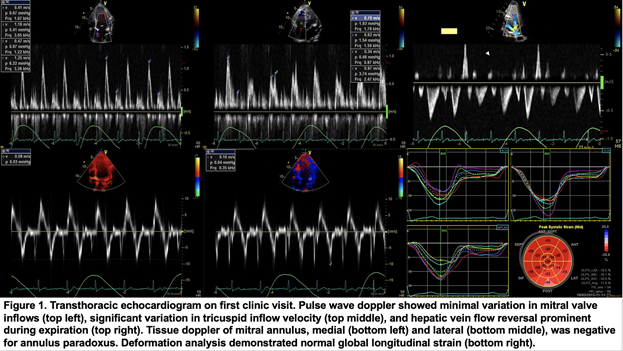
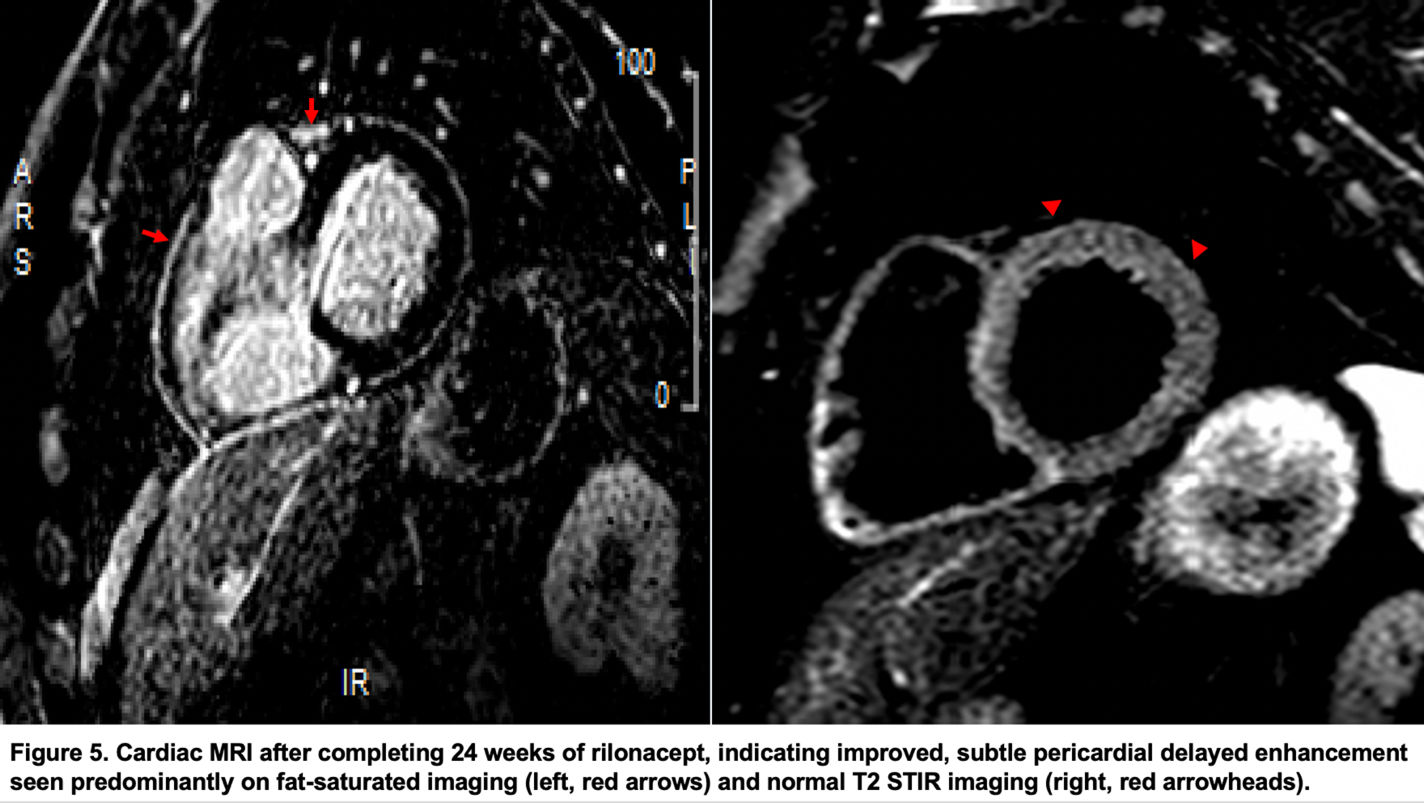
Two weeks post-discharge, during his first visit to pericardial clinic, labs showed persistently elevated ultrasensitive CRP (usCRP) 165.9 mg/L (normal <3.1 mg/L) and ESR 58 mm/hr. TTE (Figure 1) revealed trivial pericardial effusion, septal bounce, minimal respiratory variation of mitral valve inflows but significant variation in tricuspid inflow velocity, and some diastolic reversal seen in hepatic veins and superior vena cava.
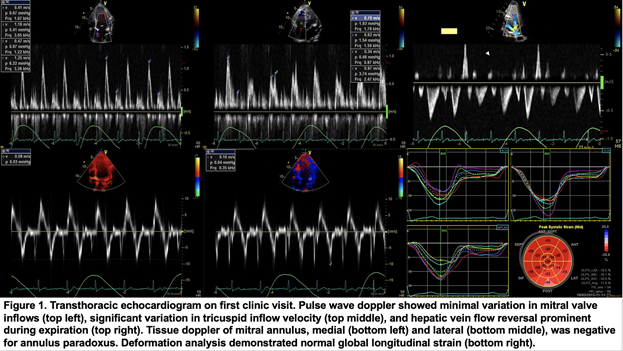
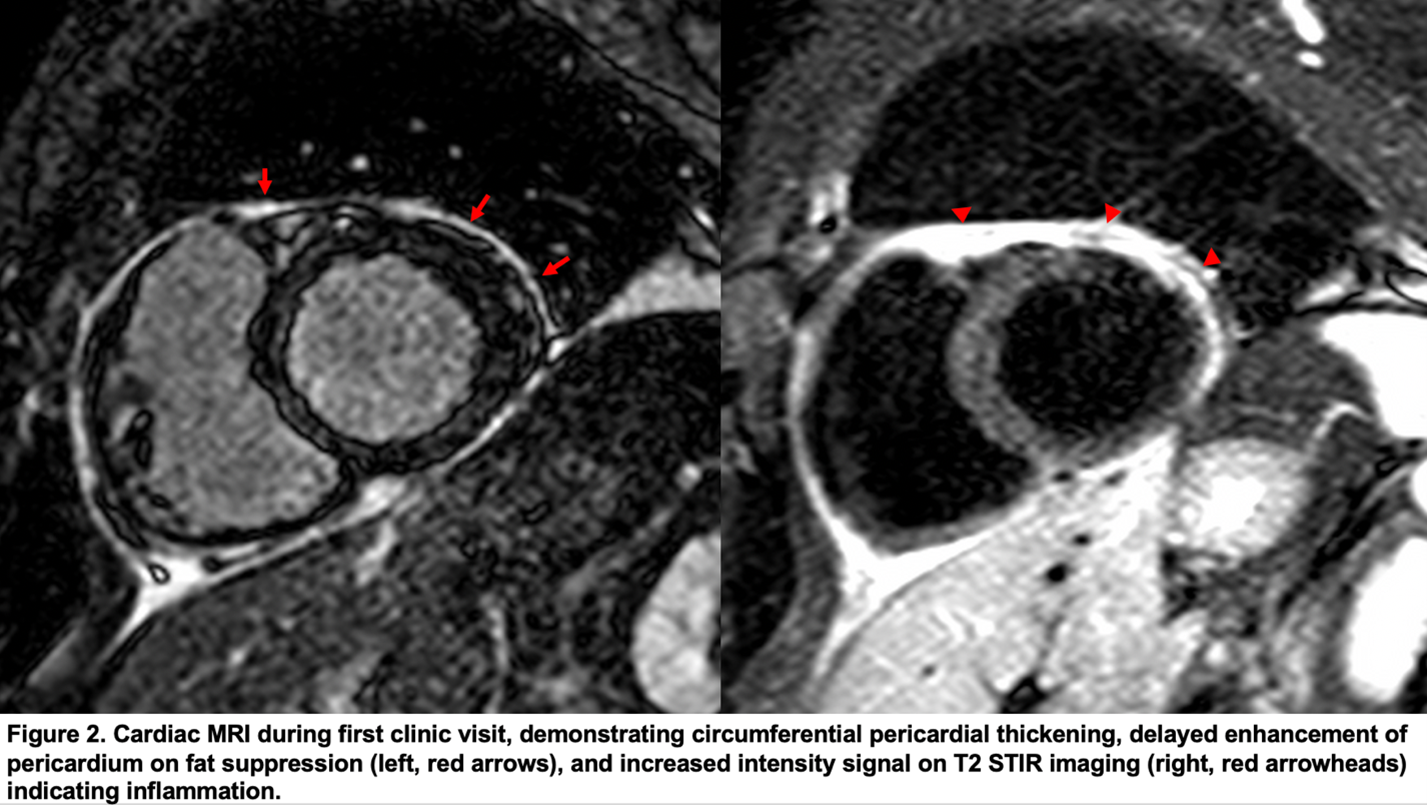
Cardiac magnetic resonance imaging (MRI) (Figure 2) noted circumferential pericardial thickening, delayed enhancement, and increased intensity signal on T2 STIR imaging indicating inflammation, without features of constrictive physiology. Based on these findings, he was started on intensive triple therapy of colchicine 0.6 mg BID, ibuprofen 400 mg TID, and prednisone 40 mg daily, with clinical improvement and corresponding downtrend in inflammatory biomarkers (usCRP 1.5 mg/L, ESR 5 mm/hr) at his 4-month follow up. Concurrently, his cardiac MRI at that time also demonstrated substantial improvement in observed inflammation, with subtle diastolic septal bounce, so patient was slowly tapered off steroids, weaned by 5mg every 2 weeks.
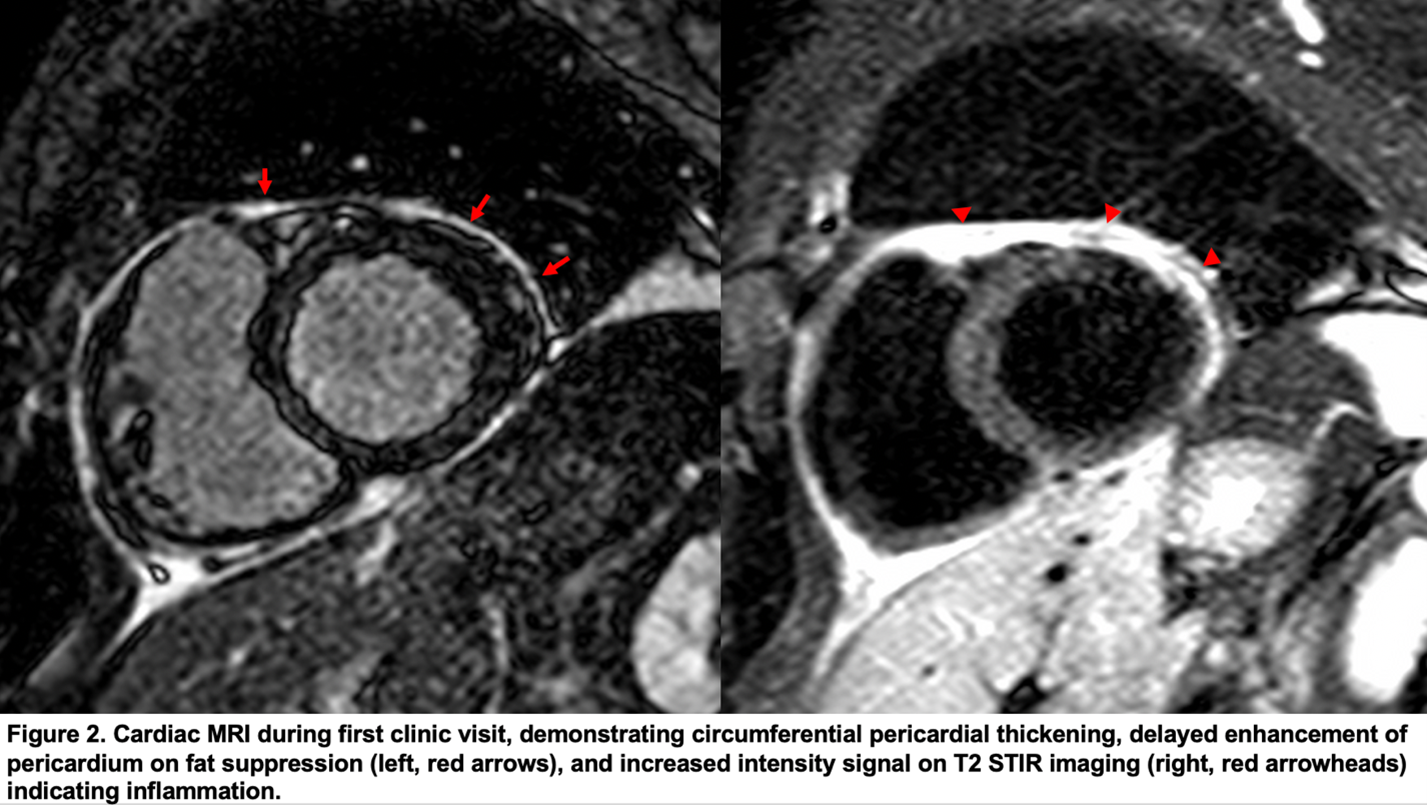
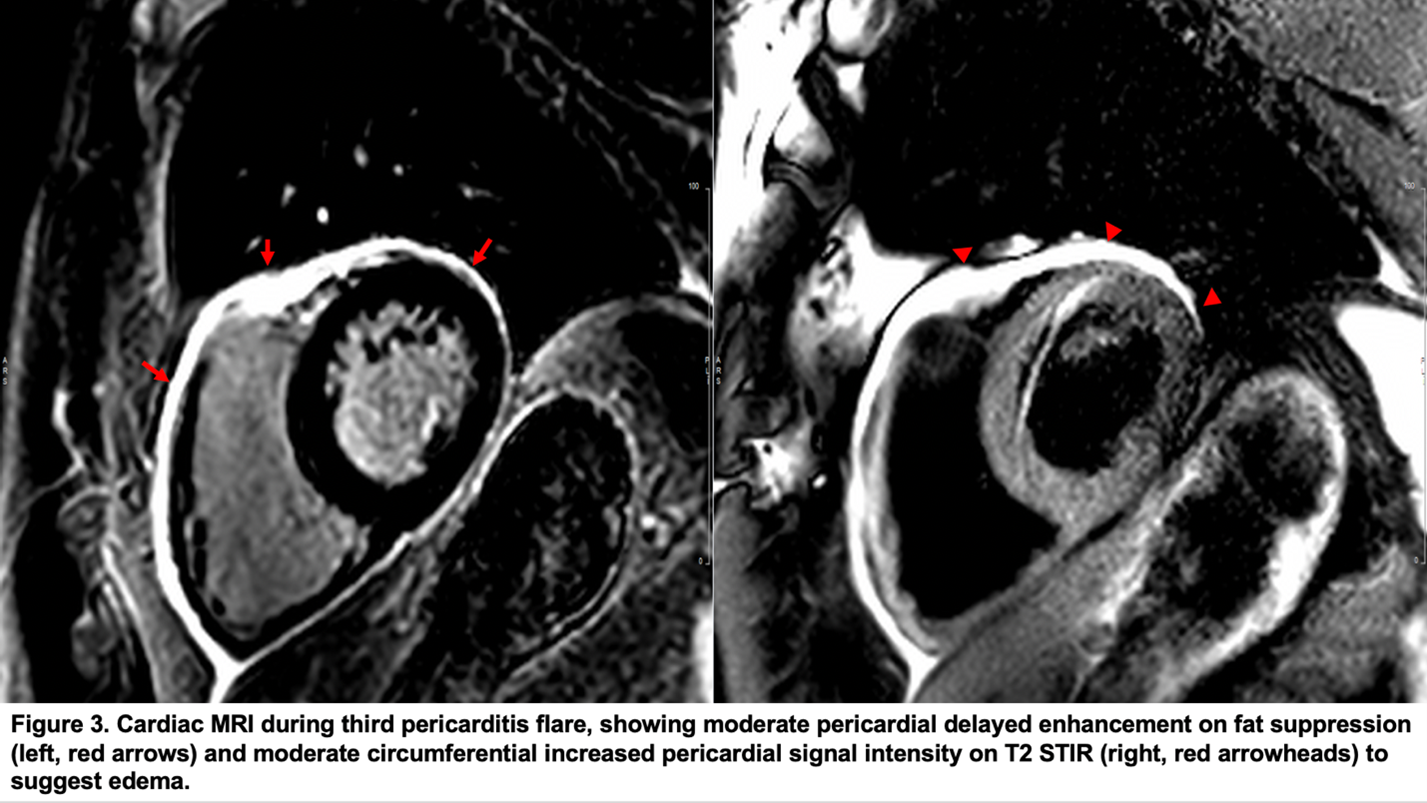
One year after his first episode of pericarditis, patient unfortunately had a second flare, corroborated by usCRP 69 mg/L and ESR 30 mm/hr. He was continued on colchicine, but up-titrated from ibuprofen 400mg TID to 800 mg TID and reinitiated on prednisone 10 mg daily. Given recurrent steroid dependence, he was trialed on immunosuppression regimen with azathioprine 150 mg daily and subsequently successfully weaned off after 2 years due to improvement in clinical status and inflammatory biomarkers (usCRP 1.2 mg/L, ESR 2 mm/hr). However, 6 months after being off all meds, he again suffered from recurrence of symptoms, with usCRP 86.2 mg/L, ESR 109 mm/hr, and the following cardiac MRI (Figure 3).
The correct answer is: D. Rilonacept (interleukin-1 receptor antagonist)
Recurrent pericarditis (RP) may occur in up 30% of patients after an initial episode of acute pericarditis.1,2 It can often be difficult to treat, resulting in debilitating chest pain that leads to frequent emergency department visits and overall reduced quality of life. RP is defined by the presence of two of the following diagnostic criteria, following a symptom-free period of ≥4-6 weeks1: characteristic pleuritic chest pain; presence of friction rub; diffuse ST elevations and PR depressions on electrocardiogram; new or worsening pericardial effusion. Often times, elevated inflammatory biomarkers are considered a supporting finding of a recurrent flare.
Initial treatment usually consists of nonsteroidal anti-inflammatory drugs (NSAID), tapered over 2-4 weeks after symptoms resolve, and ≥6 months of colchicine. Immunosuppression with corticosteroids or azathioprine are indicated for those with refractory symptoms despite NSAID plus colchicine therapy.1 In individuals with refractory, corticosteroid-dependent disease, as illustrated by our case with recurrent symptoms and elevated inflammatory biomarkers despite a pericardial window and (unsuccessful) prednisone taper, biologics such as anti-interleukin 1 therapy have emerged as a beneficial option in these patients due to their rapid, sustained effect on RP pain and safety profile.2 Pericardiectomy is almost always a last resort after all medical treatment have been exhausted as outcomes remain uncertain based on current available data.
Rilonacept, a dimeric fusion protein, inhibits IL-1 signaling by acting as a soluble decoy receptor to IL-1 alpha and beta to prevent interactions with native receptors, with the goal of reducing pericardial inflammation and injury.2 Recent phase 3 double-blind, placebo-controlled, randomized withdrawal study (RHAPSODY3) for treatment of RP patients showed a 96% reduction in risk of RP. Moreover, treatment with rilonacept allowed for discontinuation of corticosteroids without pericarditis recurrences, including patients who had been corticosteroid-dependent for disease control, and reduced annual incidence of pericarditis episodes from 3.9 episodes/year prior to the study to <0.18 episodes/year.4
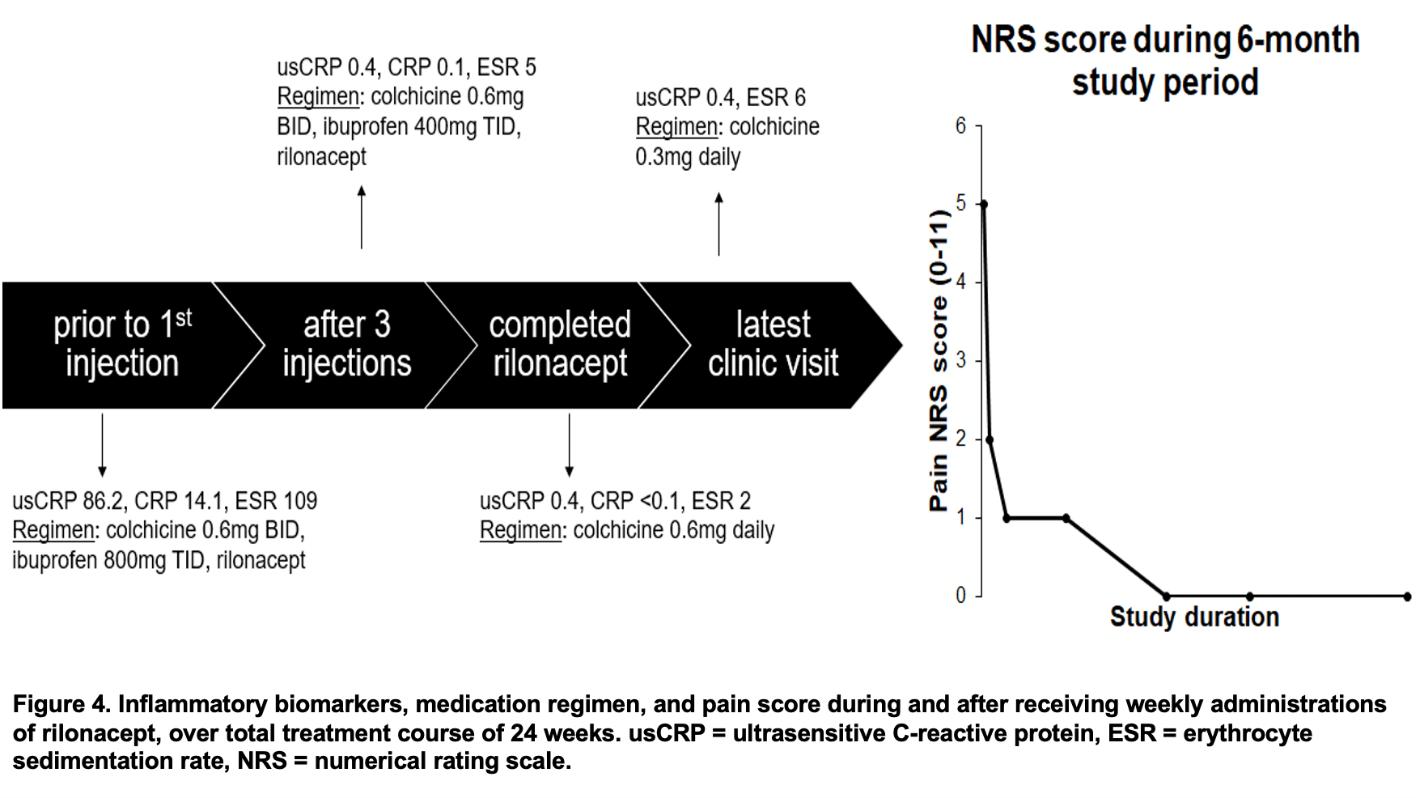
Returning to our patient, his most recent episode of symptoms represented his third pericarditis flare, as supported by the elevated inflammatory biomarkers (usCRP 86.2 mg/L, ESR 10 mm/hr) and cardiac MRI (Figure 3), which demonstrated moderate circumferential increased pericardial signal intensity on T2 STIR imaging to suggest pericardial edema and mild to moderate pericardial delayed enhancement, changes related to pericarditis. Having previously failed the steroid taper, in addition to placing him back on colchicine and ibuprofen 800 mg TID, patient received weekly administrations of rilonacept. As he completed the 24 weeks of injections, inflammatory biomarkers decreased and medications down-titrated appropriately (Figure 4).
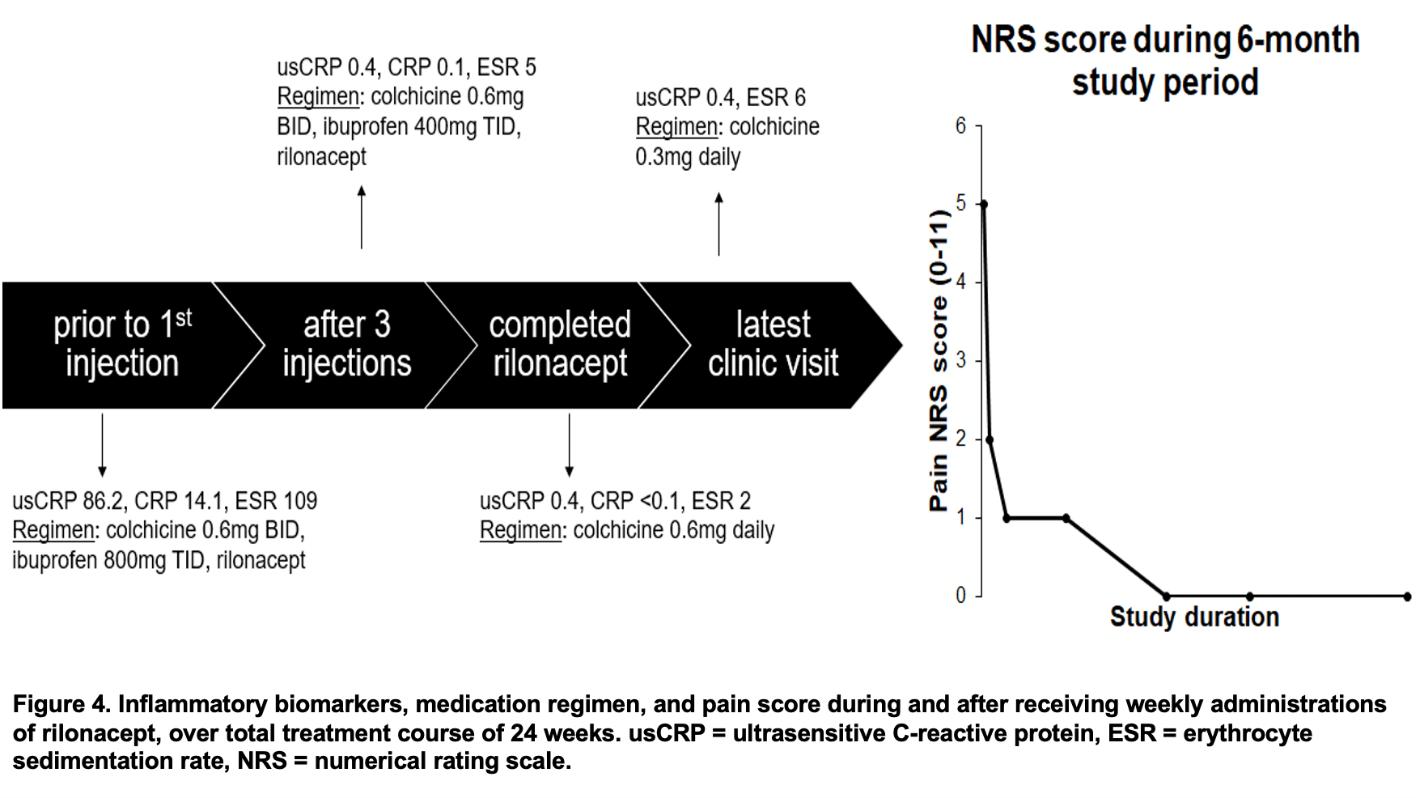
Repeat cardiac MRI showed interval improvement of previously noted moderate pericardial enhancement, with subtle pericardial delayed enhancement seen predominantly on fat saturated images (Figure 5). At his most recent follow-up, patient continued to do well clinically without further symptoms.
References
- Chiabrando JG, Bonaventura A, Vecchié A, et al. Management of acute and recurrent pericarditis: JACC State-of-the-Art Review. J Am Coll Cardiol 2020;75:76-92.
- Khayata M, Shah NP, Verma BR, et al. Usefulness of interleukin-1 receptor antagonists in patients with recurrent pericarditis. Am J Cardiol 2020;127:184-90.
- National Library of Medicine (U.S.). (2018, December – May, 2020). RHAPSODY Phase 3 Study to Assess the Efficacy and Safety of Rilonacept Treatment in Subjects with Recurrent Pericarditis (RHAPSODY). Identifier NCT03737110. www.clinicaltrials.gov/ct2/show/NCT03737110.
- Klein AL, Lin D, Cremer P, et al. Rilonacept in Recurrent Pericarditis: First Efficacy and Safety Data from an Ongoing Phase 2 Pilot Clinical Trial. J Am Coll Cardiol 2019;73:1261.