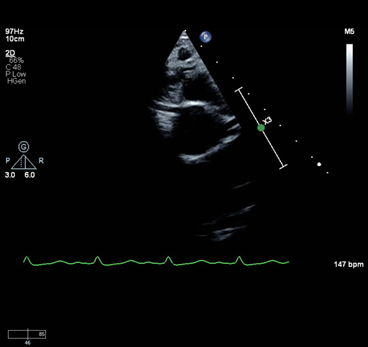
A previously healthy 11-year-old male presents after a witnessed cardiac arrest during a non-contact football practice. He was lining up for a play and suddenly dropped to the ground. There was no preceding trauma. An automated external defibrillator was placed and demonstrated a non-shockable rhythm. After several rounds of bystander CPR, a shockable rhythm was detected, and return of spontaneous circulation (ROSC) was achieved. Upon arrival to the hospital, his neurologic examination demonstrated no spontaneous movement, no breaths over the ventilator rate as well as absent gag reflex. His post-arrest electrocardiogram (ECG) was significant for sinus tachycardia and ST depression in the inferolateral and anterolateral leads. His echocardiogram showed a structurally normal heart with a mild to moderately dilated left ventricle with moderately depressed systolic function. His coronary artery origins were normal (Figure 1).
Figure 1
The correct answer is: B. Non-contrast head computed tomography (CT) scan
Sudden death in a young athlete is always a striking and devastating event. The broad category of sudden death has been defined as death within 1 hour of the onset of symptoms.1 Within this category, the occurrence of sudden death due to a cardiac etiology varies widely in the literature from 16% to up to 72% in studies where an autopsy was performed. More recently, smaller studies have been conducted to delineate the rates and causes of sudden death due to non-cardiac causes.1
When patients present after aborted sudden cardiac death, initial testing is often aimed at identifying a potential cardiac cause. An ECG is performed to evaluate cardiac rhythm and look for abnormalities such as a prolonged QTc interval. If present, this may provide a clue to the cause of the aborted sudden death. An echocardiogram is also often performed to evaluate cardiac structure, function, and coronary artery origins. In this case, post-arrest ECG was significant for sinus tachycardia and ST depression in the inferolateral and anterolateral leads, consistent with ischemic changes. Echocardiogram showed a mild to moderately dilated left ventricle with moderately depressed systolic function. Coronary artery origins were normal. If tests results are suggestive of no structural cardiac abnormality nor long QT, as in this case, one must begin to evaluate for non-cardiac causes of sudden death versus other rare channelopathies. Advanced imaging is often needed to completely rule out coronary anomalies as a cause, especially in the setting of ischemic changes in the ECG, but careful neurologic evaluation is imperative and part of the differential diagnosis.
In general in young athletes, the most common causes of non-cardiac sudden death include heat stroke, drug use, pulmonary disease, acute cerebral disease, and sickle cell disease.2,3 Determining the next best test for each patient requires the care of a multidisciplinary team including critical care, cardiology/electrophysiology, pulmonary, and neurology. This patient was scheduled for advanced cardiac imaging to further evaluate the distal coronary arteries and myocardial structure. However, neurologic exam findings were concerning for cerebral herniation, thus a portable head CT was performed at the bedside, which demonstrated abnormal increased attenuation within the sulci, cisterns, dural sinuses, and ventricular system consistent with subarachnoid hemorrhage (SAH) and intraventricular hemorrhage.
Several mechanisms of cardiac arrest secondary to SAH have been proposed including profound catecholamine release leading to cardiac stunning or a sudden spike in intracranial pressure leading to brainstem dysfunction and respiratory arrest, which leads to hypoxia and triggers the release of adenosine that leads to decreased atrioventricular conduction and eventually pulseless electrical activity or asystole.4,5 Although the patient's ECG changes were suggestive of myocardial ischemia, reflective of myocardial injury at the time of the arrest, the absence of brainstem reflexes suggested a neurologic process as the primary cause.
Choice A is a reasonable test but often takes several weeks to result and will not change the immediate plan of care for the patient. Furthermore, the clinical signs suggest a different etiology.
Choice C has been considered gold standard for coronary imaging, though CT angiography has proven to define with precision ostial morphology and intramural/interarterial and/or intraseptal/intramyocardial course of anomalous coronaries. In this case, given that the coronary origins were normal on echocardiographic imaging, a head CT should take precedence to rule out intracranial pathology prior to proceeding with a cardiac catheterization which would require heparin.
Similarly, a chest CT with pulmonary embolism protocol could be considered but would not be the next best test in a young, healthy patient with no history of clotting disorder and with neurologic findings on examination. Additionally, the echocardiogram did not have significant right ventricular changes such as enlargement, dysfunction and associated with right ventricular hypertension as would be the case in pulmonary embolism.
This case demonstrates the importance of considering a wide differential diagnosis combined with a targeted clinical examination to guide advanced testing. Any sudden cardiac arrest with the features of this case should increase clinical suspicion for a neurologic etiology.
References
- Risgaard B, Lynge TH, Wissenberg M, et al. Risk factors and causes of sudden noncardiac death: a nationwide cohort study in Denmark. Heart Rhythm 2015;12:968–74.
- Lippi G, Favaloro E, Sanchis-Gomar F. Sudden cardiac and noncardiac death in sports: epidemiology, causes, pathogenesis, and prevention. Semin Thromb Hemost 2018;44:780–86.
- Harmon KG, Asif IM, Klossner D, Drezner JA. Incidence of sudden cardiac death in National Collegiate Athletic Association athletes. Circulation 2011;123:1594–1600.
- Kim AS, Moffatt E, Ursell PC, Devinsky O, Olgin J, Tseng ZH. Sudden neurologic death masquerading as out-of-hospital sudden cardiac death. Neurology 2016;87:1669–73.
- Zachariah J, Stanich JA, Braksick SA, et al. Indicators of subarachnoid hemorrhage as a cause of sudden cardiac arrest. Clin Pract Cases Emerg Med 2017;1:132–35.